Слайд 2
Objectives
Demonstrate a basic understanding of key health literacy
concepts.
Communicate the importance of health literacy to colleagues, grantees,
and contractors.
Identify specific ways to integrate health literacy into your work.
At the end of this presentation, you will be able to:
Слайд 3
Overview
What is health literacy and why is it
important?
Health literacy at HHS
Strategies for improving health literacy
Integrating health
literacy into your work
Resources
Слайд 4
What Is Health Literacy and Why Is It
Important?
Слайд 5
What Is Health Literacy?
This slide contains video clips
of patients discussing their health literacy experiences. Patients describe
in their own words their difficulties reading medication labels, understanding informed consent forms, and following a drug regimen. In the words of one patient, "It's just a language that I'm not familiar with." The video is produced by the Academy of Educational Development in collaboration with the Institute of Medicine with special thanks to the American Medical Association Foundation and the National Center for the Study of Adult Learning and Literacy.
Слайд 6
What Is Health Literacy?
Health literacy is the degree
to which individuals have the capacity to obtain, process,
and understand basic health information and services needed to make appropriate health decisions.
Health literacy is dependent on both individual and systemic factors:
Communication skills of lay people and professionals
Knowledge of lay people and professionals of health topics
Culture
Demands of the healthcare and public health systems
Demands of the situation/context
Слайд 7
What Factors Affect Health Literacy?
Health literacy is dependent
on the communication skills of lay people and health
professionals.
Communication skills include literacy skills (e.g., reading, writing, numeracy), oral communication skills, and comprehension.
Communication skills are context specific.
Слайд 8
What Factors Affect Health Literacy?
2. Health literacy is
dependent on lay person and professional knowledge of various
health topics.
People with limited or inaccurate knowledge about the body and the causes of disease may not:
Understand the relationship between lifestyle factors (such as diet and exercise) and health outcomes
Recognize when they need to seek care
Health information can overwhelm people with advanced literacy skills.
Слайд 9
What Factors Affect Health Literacy?
3. Health literacy is
dependent on culture.
Culture affects:
How people communicate and understand
health information
How people think and feel about their health
When and from whom people seek care
How people respond to recommendations for lifestyle change and treatment
Слайд 10
What Factors Affect Health Literacy?
4. Health literacy is
dependent on the demands of the healthcare and public
health systems.
Individuals need to read, understand, and complete many kinds of forms in order to receive treatment and payment reimbursement.
Individuals need to know about the various types of health professionals and services as well as how to access care.
Слайд 11
What Factors Affect Health Literacy?
5. Health literacy is
dependent on the demands of the situation/context.
Health contexts are
unusual compared to other contexts because of an underlying stress or fear factor.
Healthcare contexts may involve unique conditions such as physical or mental impairment due to illness.
Health situations are often new, unfamiliar, and intimidating.
Слайд 12
What health literacy is NOT…
Health literacy is NOT…
Plain
Language. Plain language is a technique for communicating clearly.
It is one tool for improving health literacy.
Cultural Competency. Cultural competency
is the ability of professionals to work
cross-culturally. It can contribute to health literacy by improving communication and building trust.
Слайд 13
Why Is Health Literacy Important?
Health literacy is important
because it affects people’s ability to:
Navigate the healthcare system,
including locating providers and services and filling out forms
Share personal and health information with providers
Engage in self-care and chronic disease management
Adopt health-promoting behaviors, such as exercising and eating a healthy diet
Act on health-related news and announcements
These intermediate outcomes impact:
Health outcomes
Healthcare costs
Quality of care
Слайд 14
Health Literacy and Health Outcomes
Persons with limited health
literacy skills have:
Higher utilization of treatment services
Hospitalization
Emergency
services
Lower utilization of preventive services
Higher utilization of treatment services results in higher healthcare costs.
Слайд 15
Health Literacy and Quality of Care
Health literacy affects
the quality of health care.
“Good quality means providing patients
with
appropriate services, in a technically competent
manner, with good communication, shared
decisionmaking, and cultural sensitivity.”*
* From IOM. Crossing the Quality Chasm: A New Health System for the 21st Century. 2001.
Слайд 16
Health Literacy and Shame
People with limited health literacy
often report feeling a sense of shame about their
skill level.
Individuals with poor literacy skills are often uncomfortable about being unable to read well, and they develop strategies to compensate.
Слайд 17
Measuring Health Literacy
Health literacy is a new component
of the 2003 National Assessment of Adult Literacy (NAAL).
Nationally
representative sample of more
than 19,000 adults aged 16 and older in the United States
Assessment of English literacy using prose, document, and quantitative scales
Слайд 18
Measuring Health Literacy
Tasks used to measure health literacy
were organized around three domains:
Clinical: Filling out a patient
form
Prevention: Following guidelines for age-appropriate preventive health services
Navigation of the healthcare system: Understanding what a health insurance plan will pay for
Слайд 19
Measuring Health Literacy
Proficient: Can perform complex and challenging
literacy activities.
Intermediate: Can perform moderately challenging literacy activities.
Basic: Can
perform simple everyday literacy activities.
Below Basic: Can perform no more than the most simple and concrete literacy activities.
Nonliterate in English: Unable to complete a minimum number of screening tasks or could not be tested because did not speak English or Spanish.
Слайд 20
Percentage of Adults in Each Literacy
Level: 2003
Source:
National Center for Education Statistics, Institute for Education Sciences
Слайд 21
Nonliterate in English
Source: National Center for Education Statistics,
Institute for Education Sciences
Слайд 22
Difficulty of Selected Health
Literacy Tasks
Below Basic
Basic
Intermediate
Proficient
Circle the
date of a medical appointment on a hospital appointment
slip. (101)
Give two reasons a person should be tested for a specific disease, based on information in a clearly written pamphlet. (202)
Determine what time a person can take a prescription medication, based on information on the drug label that relates the timing of medication to eating. (253)
Calculate an employee’s share of health insurance costs for a year, using a table. (382)
Source: National Center for Education Statistics, Institute for Education Sciences
500
0
Слайд 23
Percentage of Adults in the Below Basic Health
Literacy NAAL Population: 2003
1 The “Did not obtain health
information over the Internet” category does not include prison inmates.
2 Disabilities include vision, hearing, learning disability, and other health problems.
Source: U.S. Department of Education, Institute of Education Sciences, National Center for Education Statistics, 2003 National Assessment of Adult Literacy (NAAL)
Слайд 24
Percentage of Adults in Each Health Literacy Level,
by Self-Assessment of Overall Health: 2003
Source: U.S. Department of
Education, Institute of Education Sciences, National Center for Education Statistics, 2003 National Assessment of Adult Literacy
Слайд 25
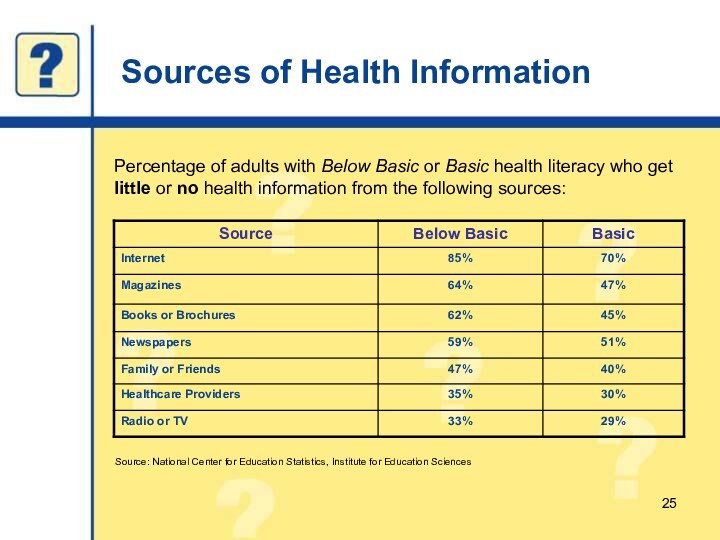
Sources of Health Information
Percentage of adults with Below
Basic or Basic health literacy who get little or
no health information from the following sources:
Source: National Center for Education Statistics, Institute for Education Sciences
Слайд 26
The Bottom Line
Only 12 percent of adults have
Proficient health literacy. In other words, nearly 9 out
of 10 adults may lack the skills needed to manage their health and prevent disease.
Fourteen percent of adults (30 million people) have Below Basic health literacy. These adults are more likely to report their health as poor
(42 percent) and are more likely to lack health insurance (28 percent) than adults with Proficient health literacy.
Слайд 27
Measuring Health Literacy
Measures of health literacy at the
individual level were developed in the 1990s:
Rapid Estimate of
Adult Literacy in Medicine (REALM)
Test of Functional Health Literacy in Adults (TOFHLA and S-TOFHLA)
Слайд 28
Measuring Health Literacy
Health literacy measures based on functional
literacy do not capture the full range of skills
needed for health literacy.
Current assessment tools (for populations and individuals) cannot differentiate among:
Reading ability
Lack of health-related background knowledge
Lack of familiarity with language and materials
Cultural differences in approaches to health.
Слайд 29
Who Is at Risk?
The problem of limited health
literacy is greater among:
Older adults
Those who are poor
People with
limited education
Minority populations
Persons with limited English proficiency (LEP)
Слайд 30
Who Is at Risk?
Many of the same populations
at risk for limited health literacy also suffer from
disparities in health status, illness (including heart disease, diabetes, obesity, HIV/AIDS, oral disease, cancer deaths, and low birth weight), and death.
Слайд 31
Health Literacy: Use of
Preventive Services
Persons with limited
health literacy skills* are more likely to skip preventive
measures such as:
Mammograms
Pap smears
Flu shots
*As defined by these studies
Слайд 32
Health Literacy: Knowledge About Medical Conditions and Treatment
Persons
with limited health literacy skills:
Are more likely to have
chronic conditions and less likely to manage them effectively.
Have less knowledge of their illness (e.g., diabetes, asthma, HIV/AIDS, high blood pressure) and its management.
Слайд 33
Health Literacy: Hospitalization and Health Status
Persons with limited
health literacy skills:
Experience more preventable hospital visits and
admissions.
Are significantly more likely to report their health as “poor.”
Слайд 34
Health Literacy: Healthcare Costs
Predicted inpatient spending for persons
with inadequate health literacy (measured by the
S-TOFHLA) was
$993 higher than that of persons with adequate health literacy.
An earlier analysis found that the additional healthcare resources attributable to inadequate health literacy were $29 billion (assuming that inadequate literacy was equivalent to inadequate health literacy):
This number would have grown to $69 billion if even one-half of marginally literate adults were also considered not health literate.
Слайд 36
Commitment to Health Literacy
Secretary Leavitt: Prevention and health
information technology (IT) are two big priorities for the
healthcare system.
Secretary Thompson’s Workgroup on Health Literacy
Prevention: A Blueprint for Action
“It is critical that individuals have access to health information in a way they can understand and make appropriate health decisions.”
Слайд 37
Office of the Surgeon General
Health literacy improvement is
one of the Surgeon General’s seven public health priorities.
“Health
literacy is the currency of success for everything I am doing as the Surgeon General.”
—Dr. Richard Carmona in his speech to the AMA House of Delegates, June 2003.
Слайд 38
Healthy People 2010 Health Communication Objectives
11-1. Internet access
in the home
11-2. Health literacy
11-3. Research and evaluation of
health
communication programs
11-4. Quality of Internet health Web sites
11-5. Centers of Excellence in health
communication
11-6. Provider-patient communication
Слайд 39
Healthy People 2010 Health Literacy Objectives
11-2. Improve the
health literacy of persons
with inadequate or marginal literacy
skills.
11-6.
Increase the proportion of persons
who report that their healthcare
providers have satisfactory
communication skills.
Слайд 40
Funding
NIH program announcement: Understanding and Promoting Health Literacy
Three
annual submission dates 2004–2006
Thirteen sponsoring institutes and offices with
AHRQ
NIH spending in FY05 for these grants is close to
$3 million, and it will total more than $8 million during the life of the awarded grants.
HRSA provides funding to community-based organizations for health literacy activities and research.
Слайд 41
Health Literacy Coordination
Department health literacy workgroup
Agency health literacy
workgroups
HHS health literacy intranet site
Quick Guide to Health Literacy
for HHS employees
Health literacy action plan
Слайд 42
Strategies for Improving Health Literacy
Слайд 43
Four Strategies for Improving Health Literacy
Improve the usability
of health information.
Improve the usability of health services.
Build knowledge
to improve decisionmaking.
Advocate for health literacy improvement.
Слайд 44
1. Improve the Usability of Health
Information
Is the information appropriate for the users?
Is the
information easy to use?
Are you speaking clearly and listening carefully?
Слайд 45
Identify the Intended Users of the Health Information
and Services
Know the intended users of the health information
and services:
Demographics
Behavior
Culture
Attitude
Literacy skills
Language
Socioeconomic status
Access to services
Decide which channel(s) and format are most appropriate.
Слайд 46
Evaluation
Evaluate users’ understanding before (formative), during (process), and
after (outcome) the introduction of materials.
Test! Test!
Test!
Слайд 47
Acknowledge Cultural Differences and Practice Respect
Accepted roles of
men and women
Value of traditional vs. Western medicine
Favorite or
forbidden foods
Manner of dress
Body language, especially touching or proximity
Слайд 48
What Is Cultural Competency?
Cultural competency is the ability
of health organizations and practitioners to recognize the following
in diverse populations to produce a positive health outcome:
Cultural beliefs
Values
Attitudes
Traditions
Language preferences
Health practices
Слайд 49
Use Plain Language
Plain language is a strategy for
making written and oral information easier to understand.
Key elements
of plain language include:
Using simple language and defining technical terms
Using the active voice
Breaking down complex information into understandable pieces
Organizing information so the most important points come first
Слайд 50
Speak Clearly and Listen Carefully
Use a medically trained
interpreter if necessary:
For those who do not speak English
well, plain English will not help.
Ensure that all language access services, including translation, are in plain language.
Refer to CLAS standards.
Ask open-ended questions:
Elicit cultural beliefs and attitudes: “Tell me about the problem and what may have caused it.”
Check for understanding:
Use the “teach-back” method: Have the person restate the information in his or her own words.
Слайд 51
Improve the Usability of Health Information on the
Internet
People cannot find the information they seek on Web
sites 60% of the time.
Many elements that improve written and oral communication can be applied to information on the Web:
— Plain language
— Large font
— White space
— Simple graphics
Don’t forget
Refer to the Office of Management and Budget (OMB) Policies for Federal Public Websites for further guidance.
Слайд 52
Improve the Usability of Health Information on the
Internet
Health literacy has implications for Web-based communication beyond written
text. Consider the following strategies:
Apply user-centered design principles and conduct usability tests.
Include interactive features and personalized content.
Organize information to minimize scrolling.
Use uniform navigation.
Слайд 53
2. Improve the Usability of
Health
Services
Improve the usability of health forms and instructions.
Improve the
accessibility of the physical environment.
Establish a patient navigator program.
Слайд 54
Health Forms and Instructions
Healthcare and public health settings
rely heavily on forms and printed instructions:
Medical history forms
Insurance
forms
Informed consent forms
Child immunization records for school
Test results
Directions to the lab or pharmacy
Hospital discharge and home care instructions
Clinical research protocols and announcements
Слайд 55
Improve the Usability of Health Forms and Instructions
Revise
forms to ensure clarity and simplicity.
Test forms with intended
users and revise as needed.
Provide forms in multiple languages.
Offer assistance with completing forms and scheduling followup care.
Слайд 56
Improve the Physical Environment
Settings with lots of signs
and postings have a high literacy demand:
Include universal symbols
and clear signage in multiple languages.
Promote easy flow through healthcare facilities.
Create a respectful and shame-free environment.
Слайд 57
Establish a Patient Navigator Program
Patient navigators are health
professionals or community health workers who help patients:
Evaluate their
treatment options.
Obtain referrals.
Find clinical trials.
Apply for financial assistance.
Congress recently passed the Patient Navigator Outreach and Chronic Disease Prevention Act of 2005.
Слайд 58
3. Build Knowledge to Improve
Decisionmaking
Improve
access to accurate and appropriate health information.
Facilitate healthy decisionmaking.
Partner
with educators to improve health curricula.
Слайд 59
Improve Access to Accurate and Appropriate Health Information
Create
new mechanisms for sharing and distributing understandable health education
materials:
Create audience or language-specific databases.
Partner with adult educators.
Identify new methods for information dissemination:
Cell phones, palm pilots, personalized and interactive content, information kiosks, talking prescription bottles, etc.
Слайд 60
Improve Access to Accurate and Appropriate Health Information
Form
partnerships with civic and faith-based organizations trusted in the
community.
Work with the media to increase awareness of health literacy issues.
Work with providers to ensure that the health information they share is accurate, current, and reliable.
Слайд 61
Facilitate Healthy Decisionmaking
Use short documents that present “bottom-line”
information, step-by-step instructions, and visual cues that highlight the
most important information:
People process and use a limited amount of information when making a decision.
Align health information and recommendations with access to services, resources, and support!
Слайд 62
Partner With Educators
Co-develop adult basic education lessons on
health topics:
Adult learners want information that is relevant to
their lives; health content is likely to engage them.
Construct lessons in which students use health-related texts, forms, and content from the Internet.
Слайд 63
Partner With Educators
The K–12 education system is a
critical point of intervention to improve health literacy.
Incorporate health-related
tasks, materials, and examples into lesson plans.
Design and disseminate health information to support existing state standards.
Speak to students or help organize health-related field trips for local schools.
Слайд 64
4. Advocate for Health Literacy
Improvement
Make
the case for improving health literacy.
Incorporate health literacy in
mission and planning.
Establish accountability for health literacy activities.
Слайд 65
Make the Case for Improving
Health Literacy
Identify specific
programs and projects affected by limited health literacy.
Target key
opinion leaders with health literacy information:
Explain how health literacy improvement relates to your mission, goals, and strategic plan.
Circulate relevant research and reports on health literacy to colleagues.
Post and share health literacy resources.
Слайд 66
Incorporate Health Literacy in Mission and Planning
Include
goals and objectives specifically related to health literacy improvement
in:
Strategic plans
Program plans
Educational initiatives
Goals can be broad (e.g., Achieving Healthy People 2010 Objective 11-2) or specific to the mission of the office/program.
Слайд 67
Include Health Literacy in Grants, Contracts, and MOUs
Recommend
that all products, materials, and forms be written in
plain language and tested with the intended audiences.
Слайд 68
Establish Accountability
Include health literacy improvement criteria in program
evaluation.
Implement health literacy metrics.
Слайд 69
Establish Accountability
Sample metrics
Our office will:
Apply user-centered design principles
to 75% of new Web pages created after January
2006.
Ensure that all documents intended for the public are reviewed by a plain language expert.
Provide all new employees with training in cultural competency and health literacy within 6 months of their date of hire.
Слайд 70
Integrating Health Literacy Into Your Work at HHS
Слайд 71
Integrating Health Literacy Into Your Work at HHS
Communicate
with the public.
Work with grantees and contractors.
Conduct and promote
research.
Manage staff and programs.
Work with external stakeholders and partners.
Слайд 72
Communicating With the Public
HHS communication functions include:
Responding to
public inquiries
Developing public health messages/campaigns
Developing materials, publications, Web sites
Improving
public access to evidence-based health information
Promoting and disseminating messages, materials, recommendations, and guidelines
Working with the media/press
Acting as public liaisons
Developing and implementing communication plans
Providing health research results
Speechwriting
Contributing to professional and academic publications
Слайд 73
Communicating With the Public
Example: Working with the media
Write
press releases aimed at the general public; use plain
language.
Provide journalists with access to health literacy resources:
Create and post a health literacy “backgrounder” for journalists online (focus on data and news “hooks”).
Highlight health literacy angle embedded in routine stories.
Слайд 74
Working With Grantees and Contractors
Require health literacy expertise
as part of the skill set for the teams
awarded contracts.
Encourage grantees to address health literacy issues in their work plans and deliverables.
Include health literacy improvement as a topic in all technical assistance and materials development grants.
Слайд 75
Working With Grantees and Contractors
Example:
Ask Funding Opportunity Announcement
applicants to explain how their projects will contribute to
meeting the health literacy objectives in Healthy People 2010.
Слайд 76
Promoting Research
Integrating health literacy into research agendas:
Review research
portfolios.
Convene research agenda-setting meetings for your topics:
Include colleagues from
across HHS who share responsibility for these topics.
Identify health literacy research questions.
Communicate research findings to health professionals and the public (shared function with Communication staff).
Слайд 77
Promoting Research
Example:
Make presentations at scholarly meetings.
Organize symposia
and sessions on health literacy at annual professional association
meetings.
Publish in professional journals.
Слайд 78
Managing Staff and Programs
Incorporate health literacy improvement into
performance plans, GPRA, and PART.
Include health literacy activities in
budget requests.
Communicate the importance of health literacy improvement to staff.
Слайд 79
Managing Staff and Programs
Example:
Conduct a senior-level briefing
at your office or agency:
Include formal presentation and handouts.
Tie
health literacy improvement to your specific mission, goals, and objectives.
Make specific recommendations.
Слайд 80
Working With External Stakeholders and Partners
External stakeholders and
partners include:
Healthcare professional organizations
Patient advocacy and support organizations
Consumer advocacy
organizations
State, local, and tribal governments
Federal departments and agencies
Academic institutions
Industry trade organizations
Media vendors and associations
Слайд 81
Working With External Partners
Arrangements may be:
Formal (e.g.,
Collaborative Research and Development Agreements and signed letters of
agreement)
Informal collaboration
In both cases, agencies can encourage partners to:
Conduct user-centered research.
Evaluate the impact of enhanced understandability.
Слайд 82
Working With External Stakeholders
Include representatives from your target
population in planning, implementation, and evaluation.
Be sure to include
organizations that represent/serve populations with limited literacy skills.
Слайд 83
Working With External Stakeholders and Partners
Examples:
When you
are soliciting proposals for presentations at HHS-sponsored events, state
your interest in receiving presentations that address health literacy issues.
Слайд 84
Who Is Responsible for Improving Health Literacy?
A health
literate America is a society in which health systems
and institutions take responsibility for providing clear communication and adequate support to facilitate health-promoting actions based on understanding.
—Institute of Medicine, 2004
Слайд 85
Who Is Responsible for Improving Health Literacy?
Our job
as HHS employees is to protect the health of
all Americans.
Healthcare providers, public health professionals, health policy makers, and health administrators are all responsible for improving health literacy.
Слайд 86
Who Is Responsible for Improving Health Literacy?
We are!
Слайд 88
Resources
AHRQ Report—Literacy and Health Outcomes (2004): www.ahrq.gov/clinic/epcsums/litsum.htm
Healthy People
2010 (2000): www.healthypeople.gov
Healthy People 2010 Health Literacy Action Plan—Communicating
Health: Priorities and Strategies for Progress (2003): http://odphp.osophs.dhhs.gov/projects/healthcomm/
objective2.htm
IOM Report—Health Literacy: A Prescription To End Confusion (2004): www.iom.edu/report.asp?id=19723
Слайд 89
Resources
NIH Improving Health Literacy Web page:
www.nih.gov/icd/od/ocpl/resources/improvinghealthliteracy.htm
NIH/AHRQ program
announcements—Understanding and Promoting Health Literacy: http://grants.nih.gov/grants/guide/pa-files/PAR-04-116.html; http://grants.nih.gov/grants/guide/pa-files/PAR-04-117.html
Prevention: A Blueprint
for Action (2004): http://aspe.hhs.gov/health/blueprint/
Слайд 90
Resources
AHRQ Health Literacy and Cultural and Linguistic Competency
Web page: www.ahrq.gov/browse/hlitix.htm
NLM Bibliography—Understanding Health Literacy and Its Barriers
(2004): www.nlm.nih.gov/pubs/cbm/healthliteracybarriers.html
CDC—Scientific and Technical Information: Simply Put: www.cdc.gov/communication/resources/simpput.pdf
CDCynergy (CD-ROM): www.cdc.gov/communication/cdcynergy.htm
NCI—Making Health Communication Programs Work (the “Pink Book”): www.cancer.gov/pinkbook