- Главная
- Разное
- Бизнес и предпринимательство
- Образование
- Развлечения
- Государство
- Спорт
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Религиоведение
- Черчение
- Физкультура
- ИЗО
- Психология
- Социология
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Геометрия
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Что такое findslide.org?
FindSlide.org - это сайт презентаций, докладов, шаблонов в формате PowerPoint.
Обратная связь
Email: Нажмите что бы посмотреть
Презентация на тему Management of cin
Содержание
- 2. Since the introduction of Colposcopy in 1924
- 3. Cervical cancer has become curable and detectable disease
- 4. This is mainly due to the fact
- 5. early detection and treatment of pre-invasive
- 6. Classification ProgressionRegression
- 7. We have no dilemma of how to
- 8. There is no dispute about the need
- 9. This two grades of CIN (CIN2 -
- 10. L-SILWhile near consensus exists regarding the evaluation
- 11. Most of low grade lesions reflects
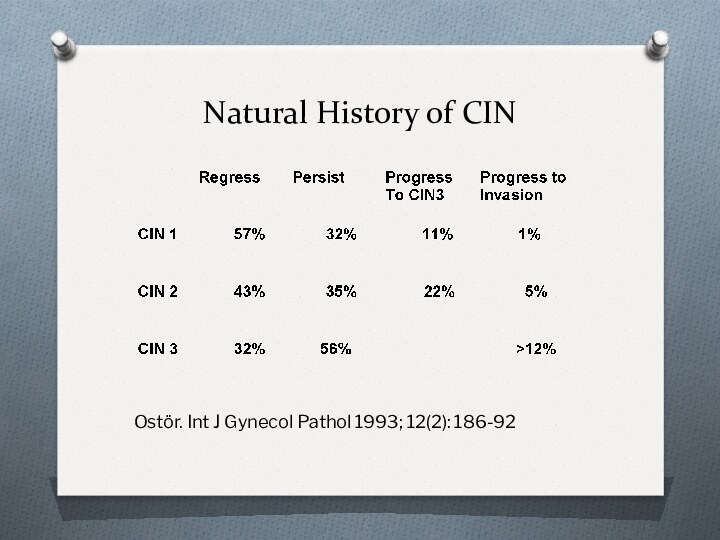
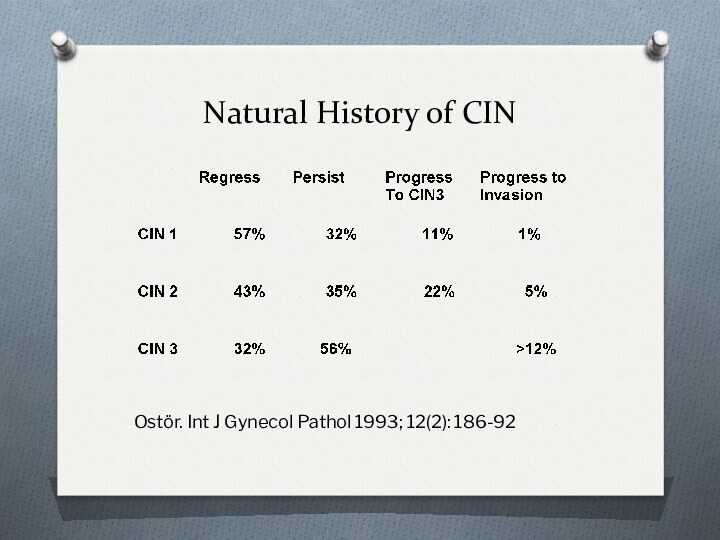
- 12. Natural History of CIN Ostör. Int J Gynecol Pathol 1993; 12(2): 186-92
- 13. after 10 years of follow-up …87.8% showing
- 14. Study enrolled more than 1000 of patients
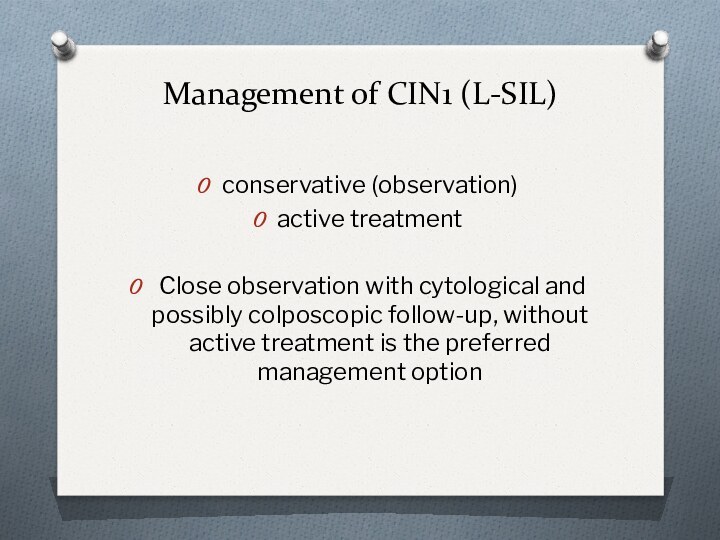
- 15. Management of CIN1 (L-SIL) conservative
- 17. Expectant management of CIN1 is not totally
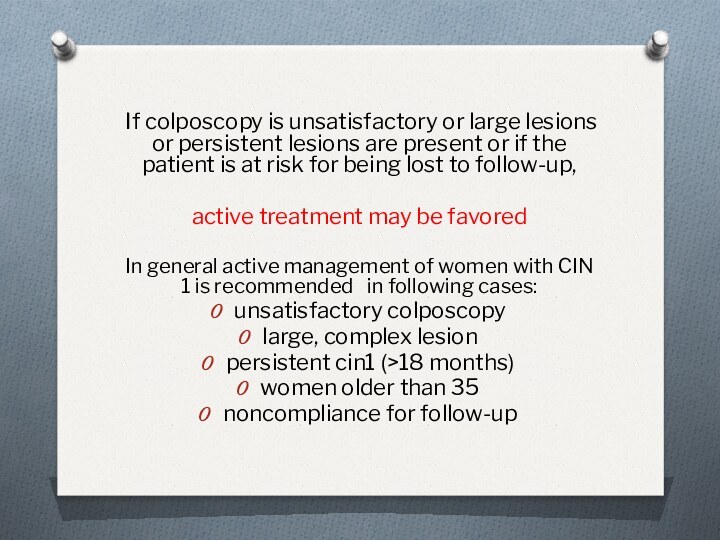
- 18. If colposcopy is unsatisfactory or large lesions
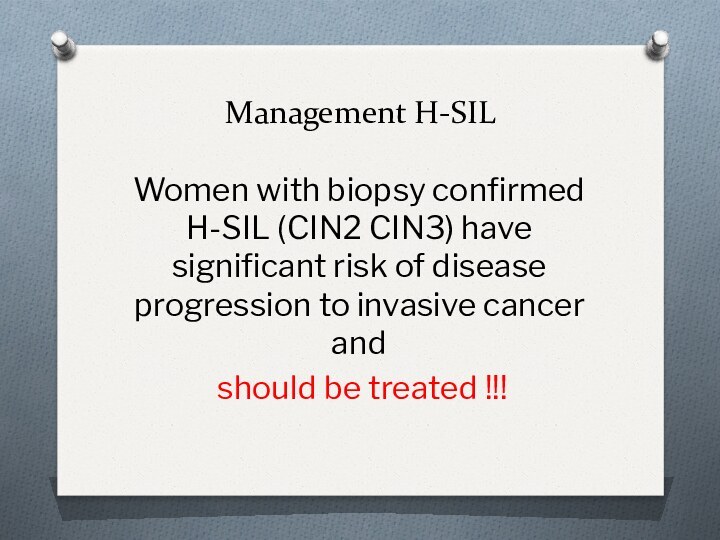
- 20. Management H-SIL Women with biopsy confirmed H-SIL
- 22. Natural History of CIN Ostör. Int J Gynecol Pathol 1993; 12(2): 186-92
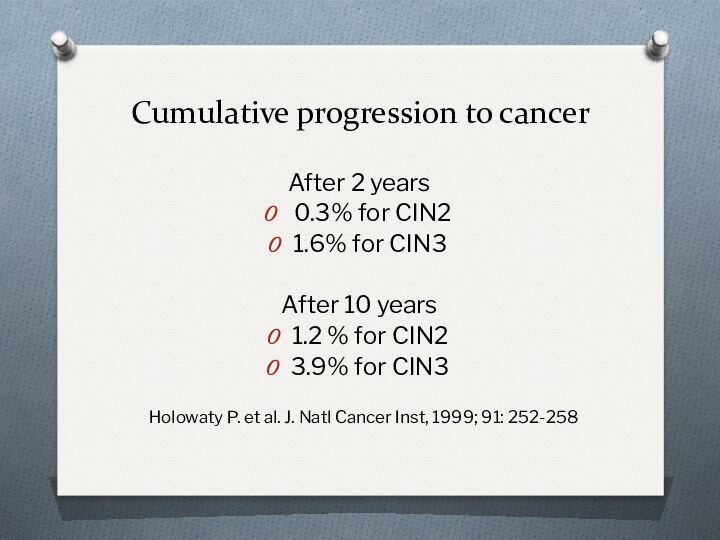
- 23. Cumulative progression to cancer After 2 years
- 24. The expectant management of CIN2 and 3with
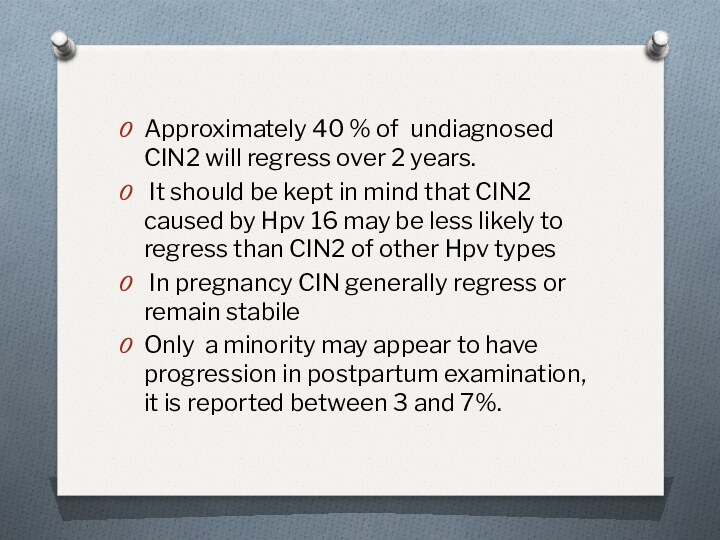
- 25. Approximately 40 % of undiagnosed CIN2 will
- 26. For high grade lesions in pregnancy the
- 27. What is an effective treatment for CIN?
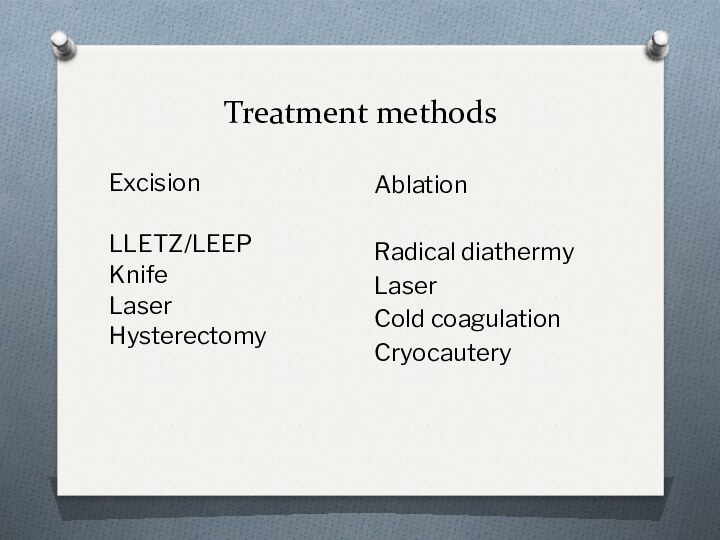
- 28. Treatment methods ExcisionLLETZ/LEEPKnifeLaserHysterectomyAblationRadical diathermyLaserCold coagulationCryocautery
- 29. Ablative techniques are only suitable when:the entire
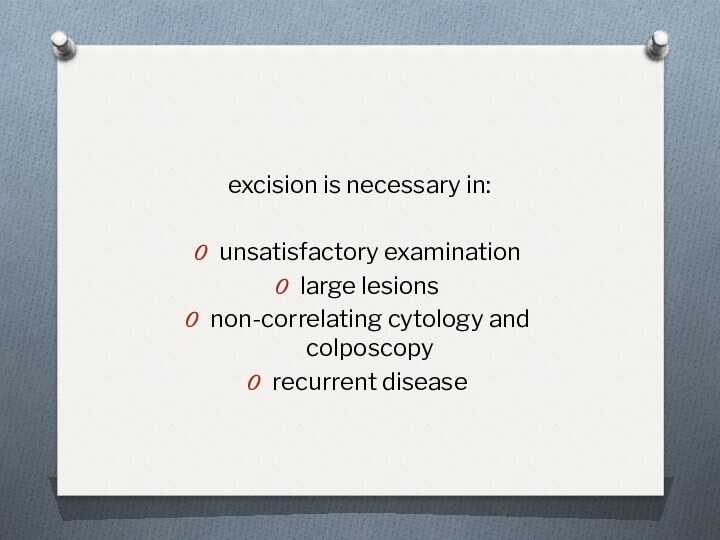
- 31. excision is necessary in:unsatisfactory examination large lesionsnon-correlating cytology and colposcopyrecurrent disease
- 34. The histology report should record:the dimension of
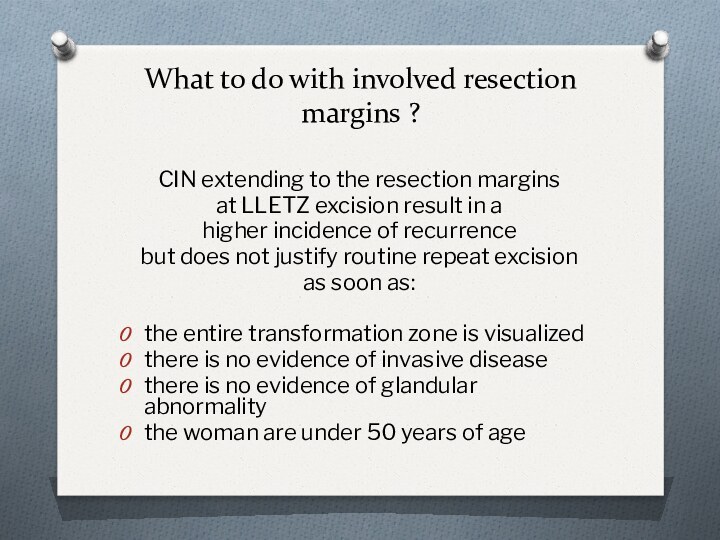
- 35. What to do with involved resection margins
- 36. Recurrence rate in relation to the margin
- 37. Unless there are other compelling reasons for
- 38. The primary goal in management of pre-invasive
- 39. Скачать презентацию
- 40. Похожие презентации
Since the introduction of Colposcopy in 1924 by Hans Hinselmann Cytology by George Papanicolau in 1946




















Слайд 4 This is mainly due to the fact that
cervical cancer has:
Long asymptomatic pre-invasive period
Effective screening methods
Successful
modalities for treatment of pre-invasive lesions Слайд 5 early detection and treatment of pre-invasive cervical
lesions have lead to significant decrease of both the
incidence and mortality of invasive cervical cancer
Слайд 7
We have no dilemma of how to diagnose
CIN
Significant controversy, however, has arisen over several aspects
of the management of cervical intraepithelial neoplasia The main questions we need to answer are:
Do all patients with CIN need therapy?
What is most appropriate therapy for CIN?
Слайд 8 There is no dispute about the need to
treat CIN 3, and few would argue that CIN
2 should be managed conservativelyToday it’s clear that in the spectrum of cervical pathology the line between premalignant and benign changes may be drawn between
CIN 1
CIN 2
CIN 3
Слайд 9 This two grades of CIN (CIN2 - 3)
are referred to as High-grade Squamous Intra-epithelial Lesions to
differentiate them from the Low-grade Lesions (CIN 1 and Hpv changes)This division now widely used in pathology originates from Bethesda system of cytological classification that was introduced in 1988 which contains SIL terms and is divided to:
Low grade - Sil (L-SIL): Hpv changes/CIN1
High grade - Sil (H-SIL): CIN 2 and 3
Слайд 10
L-SIL
While near consensus exists regarding the evaluation and
management of patients with high grade lesions the appropriate
management of patients with low grade abnormalities continues to be controversialhigh proportion of women affected
low risk of progression
significant regression may occur
Слайд 11 Most of low grade lesions reflects the
expression of Hpv infection rather than true neoplasia
Treatment
is unnecessary in many patients with L-SIL because their lesion will regress spontaneously Bansai N et al. Anticancer Res, 2008: 28:1763-6
Слайд 13
after 10 years of follow-up …
87.8% showing mild
dysplasia became normal
2.8% progressed in cin3 and
0.4% progressed to
invasive cancer Holowaty P. et al. J. Natl Cancer Inst, 1999; 91: 252-258
Слайд 14 Study enrolled more than 1000 of patients with
CIN 1 has showed that at 12 months approximately
80%
regressed to normal16% has persistent low grade
while 4% progressed to high grade lesions
Bansai N et al. Anticancer Res, 2008: 28:1763-6
Слайд 15
Management of CIN1 (L-SIL)
conservative (observation)
active treatment
Close observation with cytological and possibly colposcopic follow-up,
without active treatment is the preferred management option Слайд 17 Expectant management of CIN1 is not totally without
some risk
potential for a high-grade lesion to develop
during follow-upalready existing high-grade lesion that was not correctly diagnosed
loss to follow-up
Слайд 18 If colposcopy is unsatisfactory or large lesions or
persistent lesions are present or if the patient is
at risk for being lost to follow-up,active treatment may be favored
In general active management of women with CIN 1 is recommended in following cases:
unsatisfactory colposcopy
large, complex lesion
persistent cin1 (>18 months)
women older than 35
noncompliance for follow-up
Слайд 20
Management H-SIL
Women with biopsy confirmed H-SIL (CIN2
CIN3) have significant risk of disease progression to invasive
cancer andshould be treated !!!
Слайд 23
Cumulative progression to cancer
After 2 years
0.3%
for CIN2
1.6% for CIN3
After 10 years
1.2 % for CIN2
3.9%
for CIN3Holowaty P. et al. J. Natl Cancer Inst, 1999; 91: 252-258
Слайд 24
The expectant management of CIN2 and 3
with repeat
cytology and colposcopy
is not acceptable except for:
very young
patients with CIN2pregnant patients
Слайд 25 Approximately 40 % of undiagnosed CIN2 will regress
over 2 years.
It should be kept in mind
that CIN2 caused by Hpv 16 may be less likely to regress than CIN2 of other Hpv types In pregnancy CIN generally regress or remain stabile
Only a minority may appear to have progression in postpartum examination, it is reported between 3 and 7%.
Слайд 26 For high grade lesions in pregnancy the risk
of progression of CIN 2 and 3 in invasive
disease is relatively small but they should be reexamined every 6-8 weeks with cytology and colposcopyFor very big lesions in pregnancy large biopsy or even cone should not be delayed
Слайд 27
What is an effective treatment for CIN?
There
is no obviously superior conservative surgical technique for treating
and eradicating cervical intra-epithelial neoplasiaExcision is preferred because of better histological assessment
Слайд 28
Treatment methods
Excision
LLETZ/LEEP
Knife
Laser
Hysterectomy
Ablation
Radical diathermy
Laser
Cold coagulation
Cryocautery
Слайд 29
Ablative techniques are only suitable when:
the entire transformation
zone is visualized
there is no evidence of glandular
abnormality there is no evidence of invasive disease
there is no discrepancy between cytology and colposcopy
no previous treatment
Слайд 31
excision is necessary in:
unsatisfactory examination
large lesions
non-correlating cytology
and colposcopy
recurrent disease
Слайд 34
The histology report should record:
the dimension of specimen
the status of resection margins
with regard to intraepithelial
or invasive disease for ectocervical lesions treatment techniques should remove tissue to a depth of at least 7 mm
Слайд 35 What to do with involved resection margins ?
CIN extending to the resection margins
at LLETZ excision result
in ahigher incidence of recurrence
but does not justify routine repeat excision
as soon as:
the entire transformation zone is visualized
there is no evidence of invasive disease
there is no evidence of glandular abnormality
the woman are under 50 years of age