- Главная
- Разное
- Бизнес и предпринимательство
- Образование
- Развлечения
- Государство
- Спорт
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Религиоведение
- Черчение
- Физкультура
- ИЗО
- Психология
- Социология
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Геометрия
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Что такое findslide.org?
FindSlide.org - это сайт презентаций, докладов, шаблонов в формате PowerPoint.
Обратная связь
Email: Нажмите что бы посмотреть
Презентация на тему Acute Cholecystitis
Содержание
- 2. Acute cholecystitis is the most common complication
- 3. Acute acalculous cholecystitisAcalculous cholecystitis is cholecystitis without
- 4. Symptoms and SignsMost patients have had prior
- 5. ComplicationsWithout treatment, 10% of patients develop localized
- 8. Скачать презентацию
- 9. Похожие презентации
Acute cholecystitis is the most common complication of cholelithiasis. Conversely, ≥ 95% of patients with acute cholecystitis have cholelithiasis. When a stone becomes impacted in the cystic duct and persistently obstructs it, acute inflammation results. Bile stasis triggers
Слайд 3
Acute acalculous cholecystitis
Acalculous cholecystitis is cholecystitis without stones.
It accounts for 5 to 10% of cholecystectomies done
for acute cholecystitis. Risk factors include the following:Critical illness (eg, major surgery, burns, sepsis, or trauma)
Prolonged fasting or TPN (both predispose to bile stasis)
Shock
Immune deficiency
Vasculitis (eg, SLE, polyarteritis nodosa)
The mechanism probably involves inflammatory mediators released because of ischemia, infection, or bile stasis. Sometimes an infecting organism can be identified (eg, Salmonella sp or cytomegalovirus in immunodeficient patients). In young children, acute acalculous cholecystitis tends to follow a febrile illness without an identifiable infecting organism.
Слайд 4
Symptoms and Signs
Most patients have had prior attacks
of biliary colic or acute cholecystitis. The pain of
cholecystitis is similar in quality and location to biliary colic but lasts longer (ie, > 6 h) and is more severe. Vomiting is common, as is right subcostal tenderness. Within a few hours, the Murphy sign (deep inspiration exacerbates the pain during palpation of the right upper quadrant and halts inspiration) develops along with involuntary guarding of upper abdominal muscles on the right side. Fever, usually low grade, is common.In the elderly, the first or only symptoms may be systemic and nonspecific (eg, anorexia, vomiting, malaise, weakness, fever). Sometimes fever does not develop.
Acute cholecystitis begins to subside in 2 to 3 days and resolves within 1 wk in 85% of patients even without treatment.
Слайд 5
Complications
Without treatment, 10% of patients develop localized perforation,
and 1% develop free perforation and peritonitis. Increasing abdominal
pain, high fever, and rigors with rebound tenderness or ileus suggest empyema (pus) in the gallbladder, gangrene, or perforation. When acute cholecystitis is accompanied by jaundice or cholestasis, partial common duct obstruction is likely, usually due to stones or inflammation.Other complications include the following:
Mirizzi syndrome: Rarely, a gallstone becomes impacted in the cystic duct and compresses and obstructs the common bile duct, causing cholestasis.
Gallstone pancreatitis: Gallstones pass from the gallbladder into the biliary tract and block the pancreatic duct.
Cholecystoenteric fistula: Infrequently, a large stone erodes the gallbladder wall, creating a fistula into the small bowel (or elsewhere in the abdominal cavity); the stone may pass freely or obstruct the small bowel (gallstone ileus).
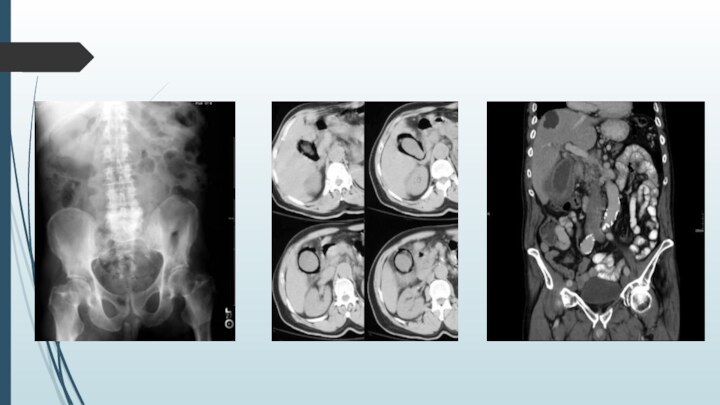
Слайд 7
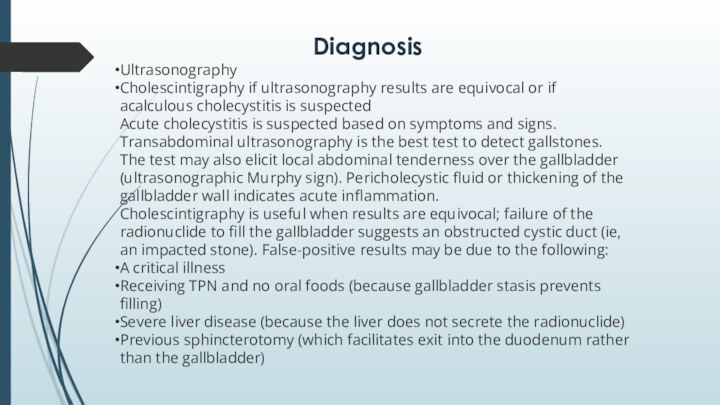
Diagnosis
Ultrasonography
Cholescintigraphy if ultrasonography results are equivocal or if acalculous cholecystitis is suspected
Acute cholecystitis is suspected based on symptoms and signs.
Transabdominal ultrasonography is the best test to detect gallstones. The test may also elicit local abdominal tenderness over the gallbladder (ultrasonographic Murphy sign). Pericholecystic fluid or thickening of the gallbladder wall indicates acute inflammation.
Cholescintigraphy is useful when results are equivocal; failure of the radionuclide to fill the gallbladder suggests an obstructed cystic duct (ie, an impacted stone). False-positive results may be due to the following:
A critical illness
Receiving TPN and no oral foods (because gallbladder stasis prevents filling)
Severe liver disease (because the liver does not secrete the radionuclide)
Previous sphincterotomy (which facilitates exit into the duodenum rather than the gallbladder)