- Главная
- Разное
- Бизнес и предпринимательство
- Образование
- Развлечения
- Государство
- Спорт
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Религиоведение
- Черчение
- Физкультура
- ИЗО
- Психология
- Социология
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Геометрия
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Что такое findslide.org?
FindSlide.org - это сайт презентаций, докладов, шаблонов в формате PowerPoint.
Обратная связь
Email: Нажмите что бы посмотреть
Презентация на тему Takayasu’s arteritis
Содержание
- 7. EpidemiologyMore case reports from Japan ,India, South-east
- 8. AgeMc-2nd & 3rd decadeMay range from
- 10. HistopathologyIdiopathic inflammatory arteritis of elastic arteries resulting
- 11. Pathogenesis Antigen-driven disease, with the site of
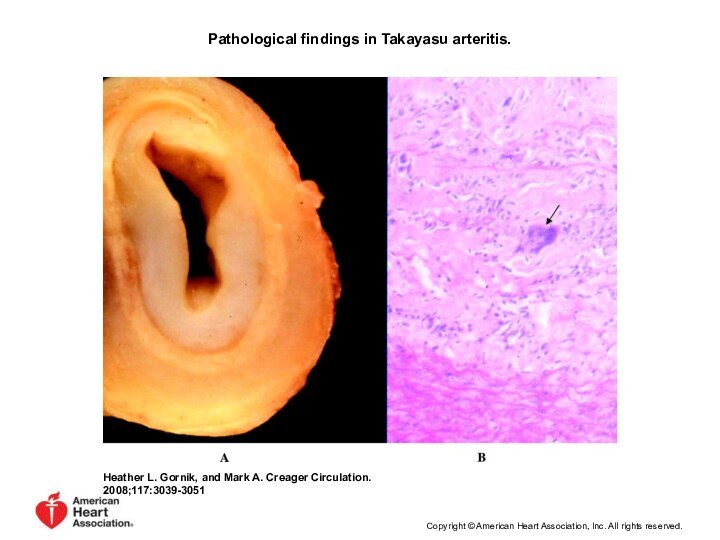
- 12. Pathological findings in Takayasu arteritis. Heather L.
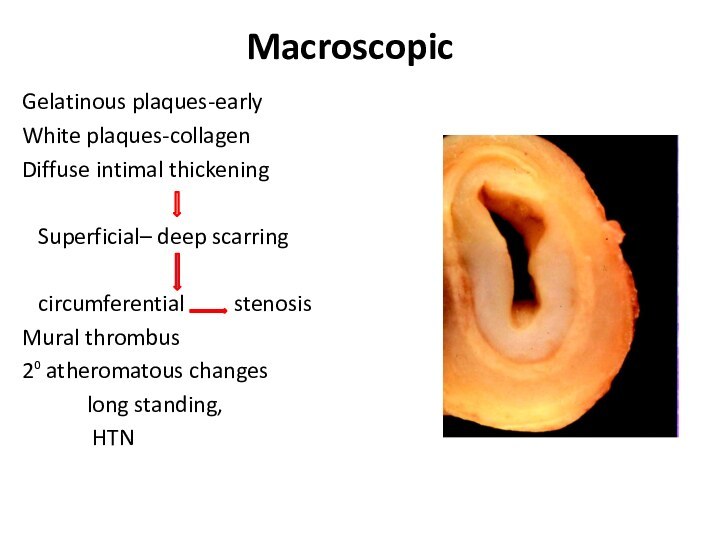
- 13. MacroscopicGelatinous plaques-earlyWhite plaques-collagenDiffuse intimal thickening Superficial–
- 14. MacroscopicWall thickening, fibrosis, stenosis, thrombus formation →end
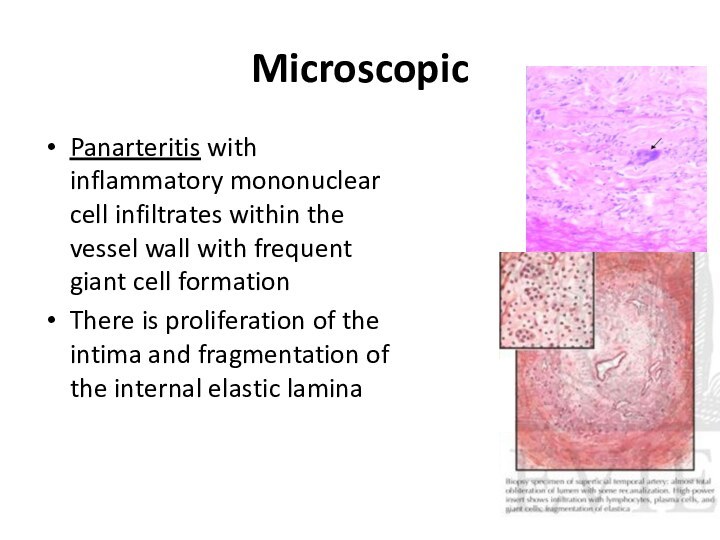
- 15. MicroscopicPanarteritis with inflammatory mononuclear cell infiltrates within
- 17. Clinical featuresEarly pre-pulseless/gen manifestationsFever, weight loss,headache, fatigue,malaise,night
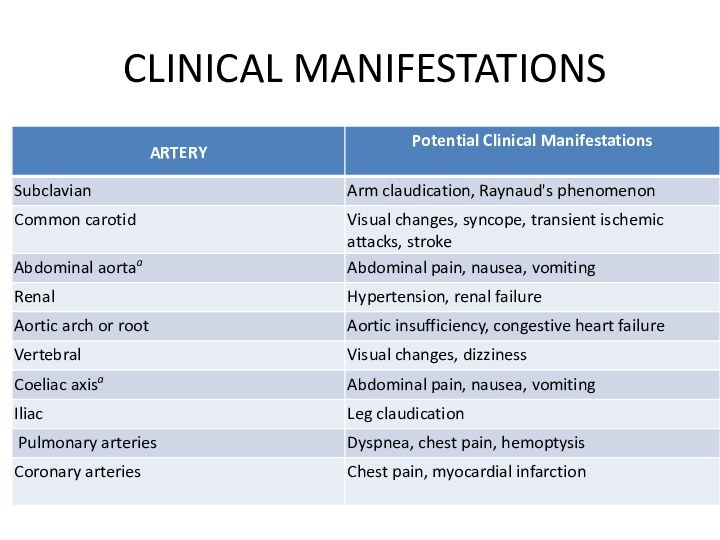
- 18. CLINICAL MANIFESTATIONS
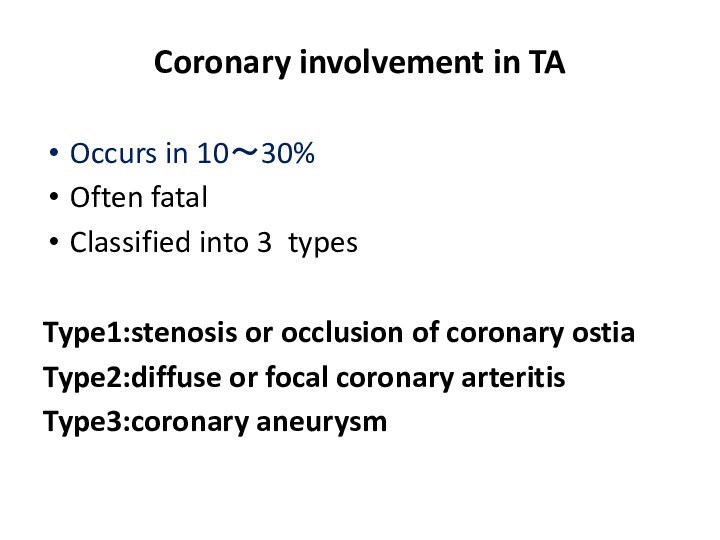
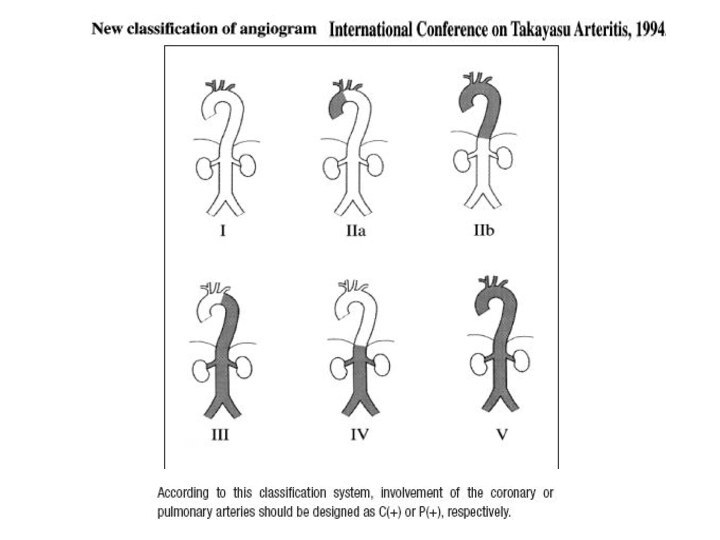
- 20. Coronary involvement in TAOccurs in 10~30%Often fatalClassified
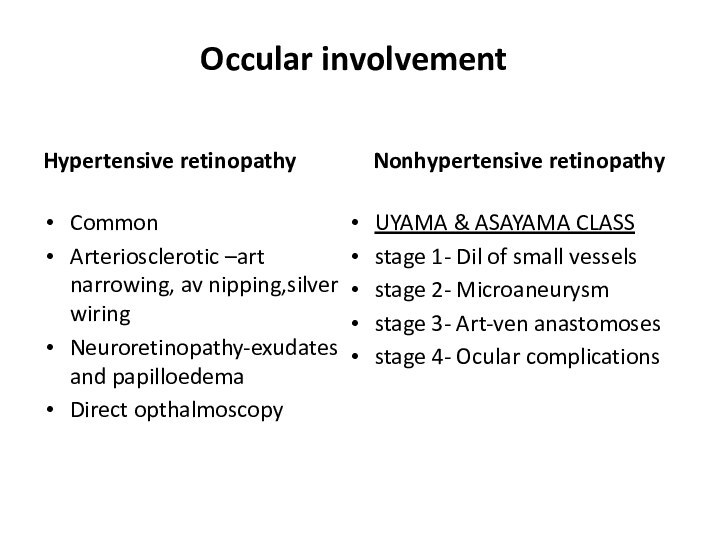
- 21. Occular involvementHypertensive retinopathyCommonArteriosclerotic –art narrowing, av nipping,silver
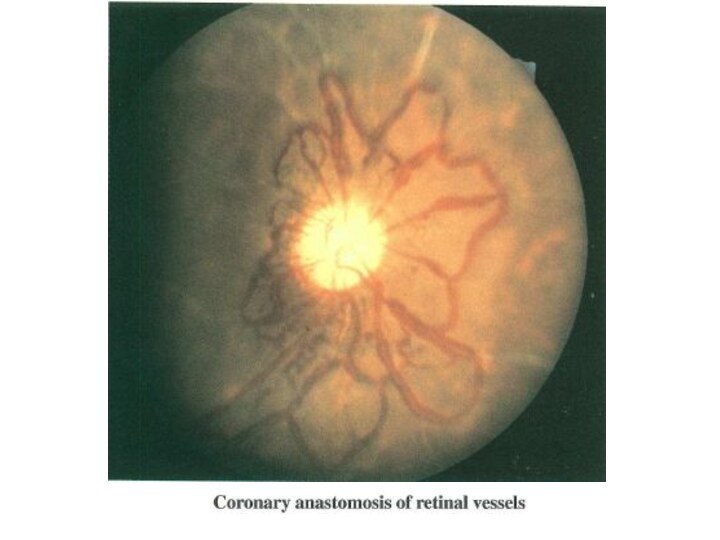
- 23. nee
- 24. Severe arteritis with complete occlusion of left
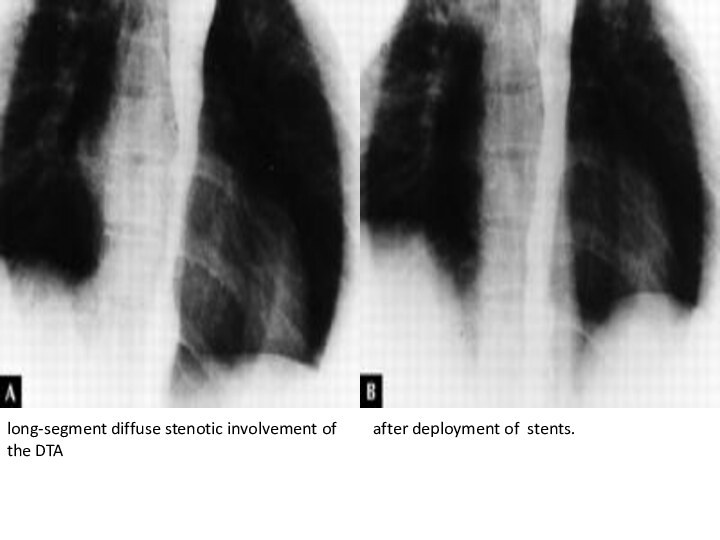
- 25. long-segment diffuse stenotic involvement of the DTAafter deployment of stents.
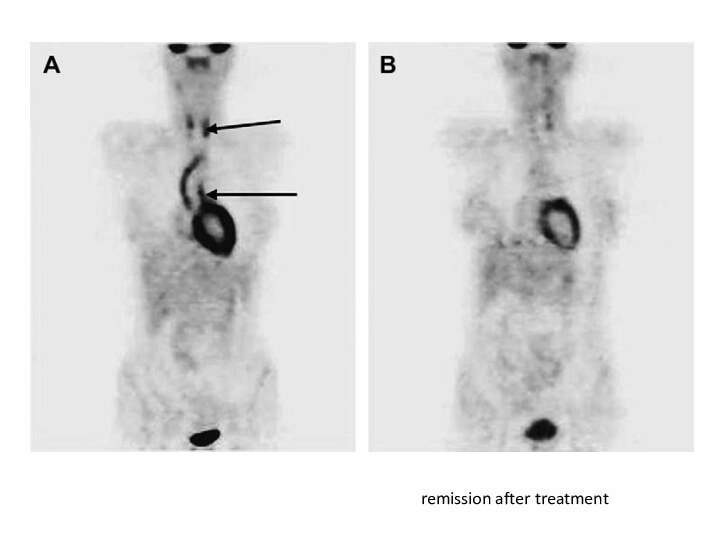
- 26. remission after treatment
- 27. Figure 4. Takayasu arteritis involving the coronary
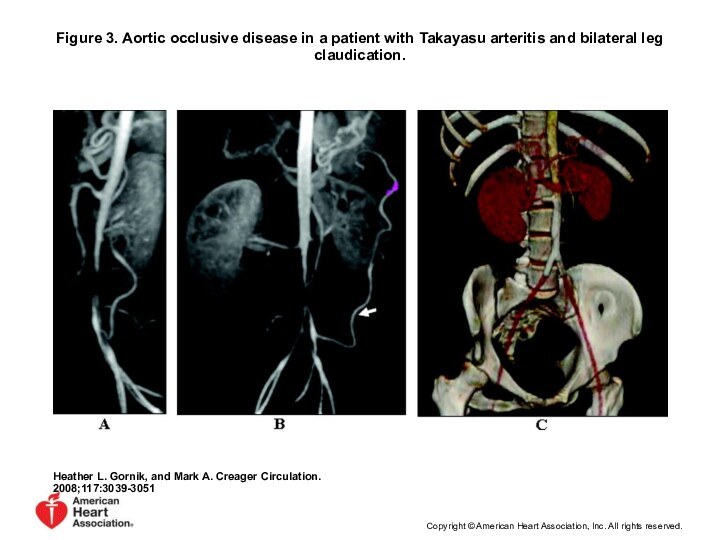
- 28. Figure 3. Aortic occlusive disease in a
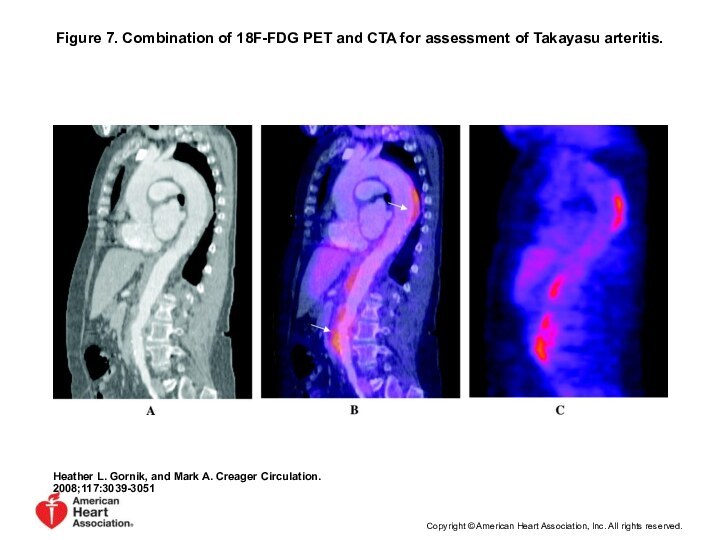
- 29. Figure 7. Combination of 18F-FDG PET and
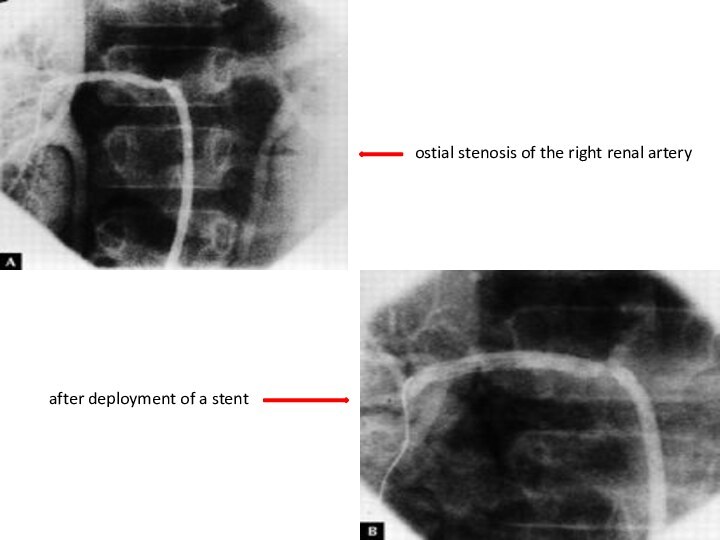
- 30. ostial stenosis of the right renal arteryafter deployment of a stent
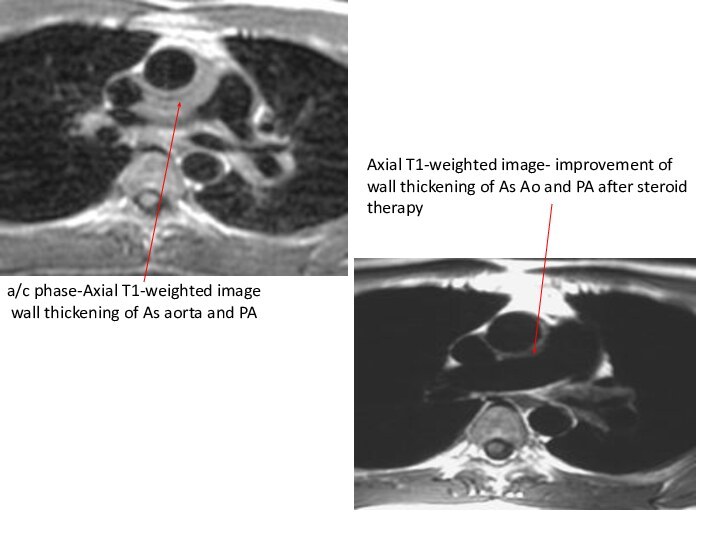
- 31. a/c phase-Axial T1-weighted image wall thickening
- 33. Diagnosis The diagnosis of Takayasu's arteritis should
- 34. Treatment Disease-related mortality most often occurs from
- 35. Treatment of TA ・ Steroidsimmunosuppressants:Cyclosporine,Cyclophosphamide,Mtx,Mycophenolate mofetilAnti-platelet therapy(low-dose Aspirin)angioplasty/surgeryIf uncontrolledControl of vasculitisSymptomatic occlusionthrombosis
- 36. Pharmacological treatment 0.7-1 mg/kg/day –prednisone for 1-3
- 37. Steroids → 50% responseMethotrexate →further 50% respond25%
- 38. Critical issue is in trying to determine
- 39. Скачать презентацию
- 40. Похожие презентации
EpidemiologyMore case reports from Japan ,India, South-east Asia, MexicoNo geographic restrictionNo race – immuneIncidence-2.6/million/year-N.America/EuropeThe incidence in Asia is 1 case/1000-5000 women.
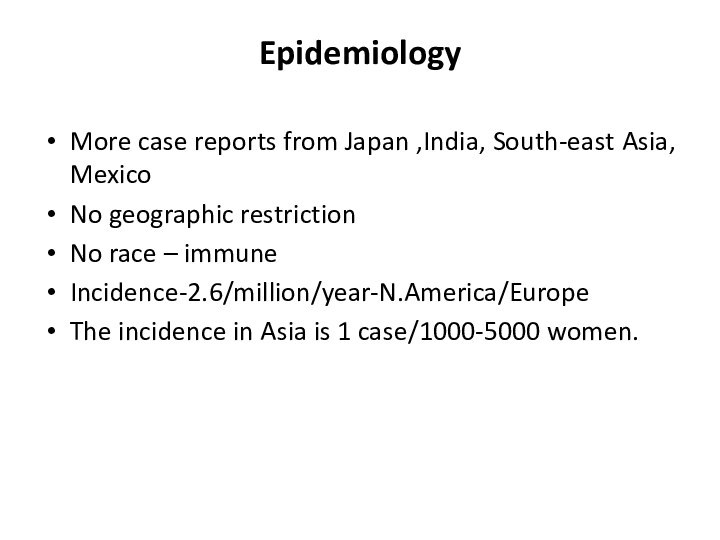
Слайд 7
Epidemiology
More case reports from Japan ,India, South-east Asia,
Mexico
is 1 case/1000-5000 women.
Слайд 8
Age
Mc-2nd & 3rd decade
May range from infancy
to middle age
Indian studies-age 3- 50 y
Gender diff
Japan-F:M=8-9:1
India-F:M ratio varies from -1:1 - 3:1
Epidemiology
Слайд 9
Genetics
Japan - HLA-B52 and B39
Mexican and Colombian patients - HLA-DRB1*1301 and HLA-DRB1*1602
India- HLA- B 5, -B 21
Слайд 10
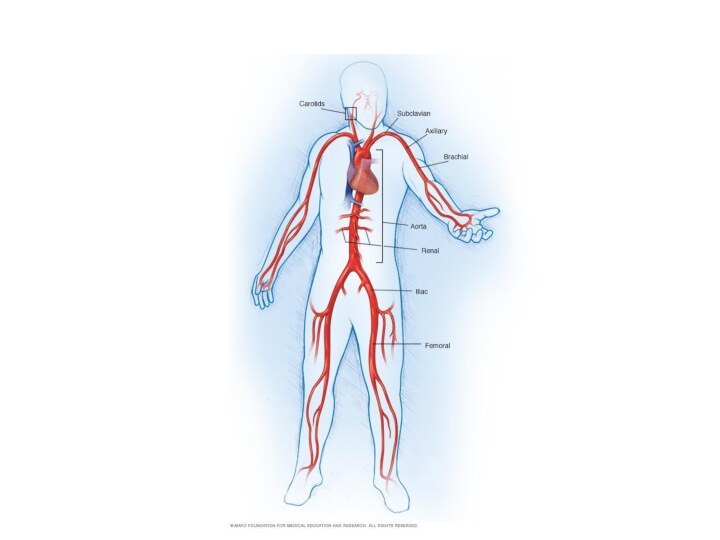
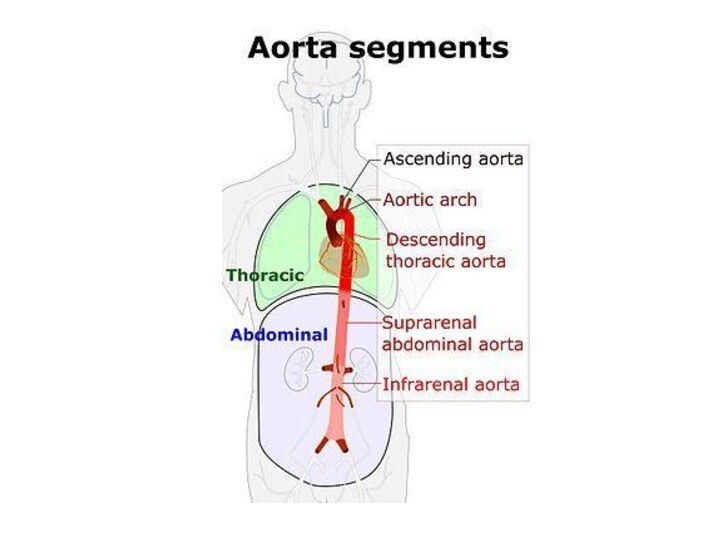
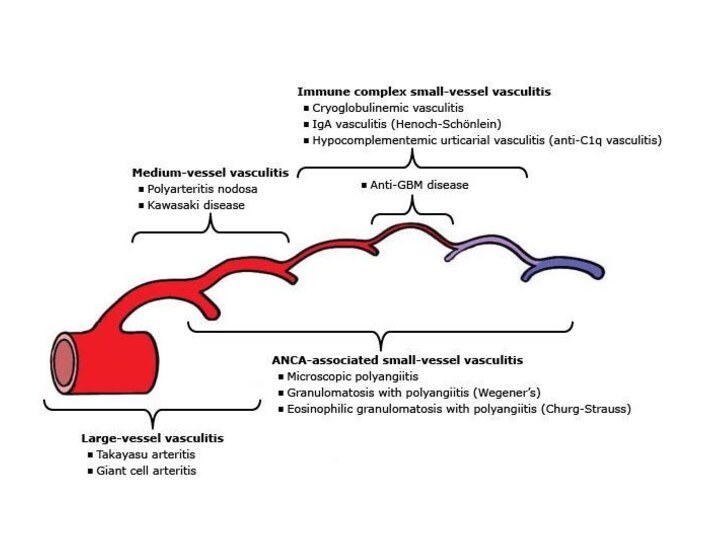
Histopathology
Idiopathic inflammatory arteritis of elastic arteries resulting in
occlusive/ ectatic changes
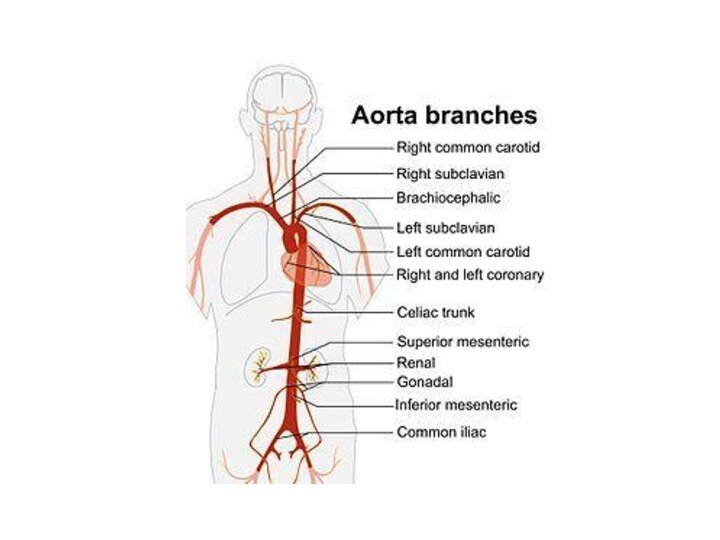
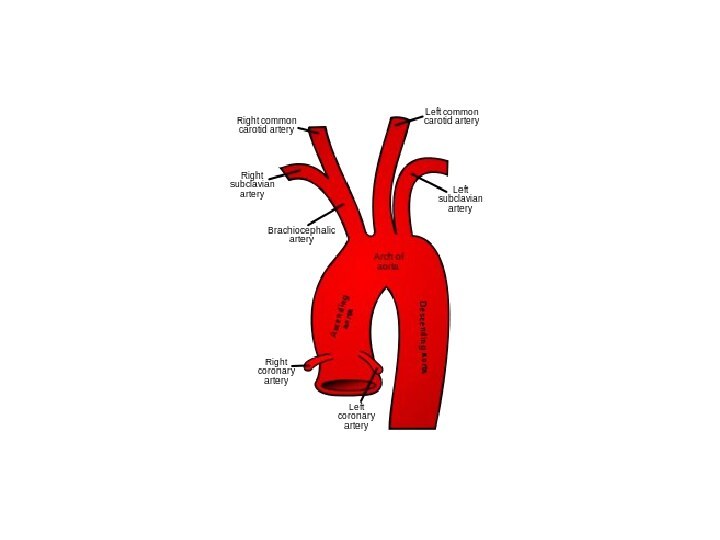
Large vessels – Aorta and its main
branches (brachiocephalic, carotid, SCL, vertebral, RA) Coronary and PA involvement
Aorta - usually not beyond IMA
Multiple segments with skipped areas
or diffuse involvement
Слайд 11
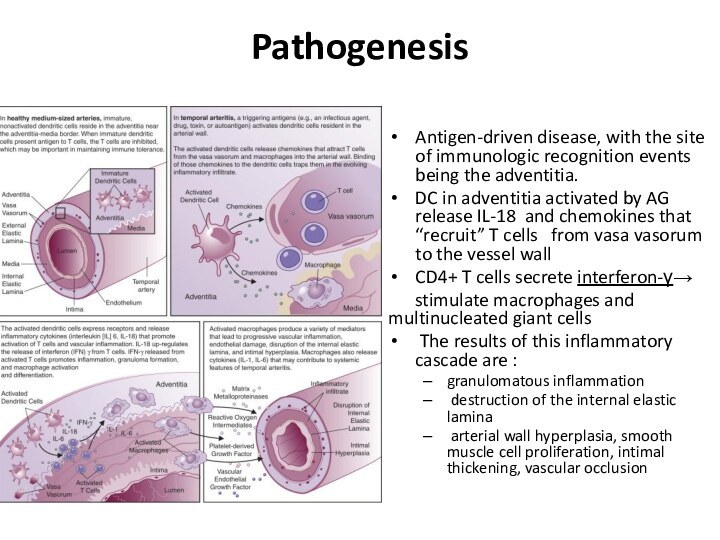
Pathogenesis
Antigen-driven disease, with the site of immunologic
recognition events being the adventitia.
DC in adventitia activated by
AG release IL-18 and chemokines that “recruit” T cells from vasa vasorum to the vessel wallCD4+ T cells secrete interferon-γ→
stimulate macrophages and multinucleated giant cells
The results of this inflammatory cascade are :
granulomatous inflammation
destruction of the internal elastic lamina
arterial wall hyperplasia, smooth muscle cell proliferation, intimal thickening, vascular occlusion
Слайд 12
Pathological findings in Takayasu arteritis.
Heather L. Gornik,
and Mark A. Creager Circulation. 2008;117:3039-3051
Copyright © American Heart
Association, Inc. All rights reserved.
Слайд 13
Macroscopic
Gelatinous plaques-early
White plaques-collagen
Diffuse intimal thickening
Superficial– deep
scarring
circumferential stenosis
Mural thrombus
2⁰
atheromatous changeslong standing,
HTN
Слайд 14
Macroscopic
Wall thickening, fibrosis, stenosis, thrombus formation →end organ
ischemia
More inflammation → destroys arterial media → Aneurysm (fibrosis
inadequate)Most patients with aneurysms also have stenosis
Слайд 15
Microscopic
Panarteritis with inflammatory mononuclear cell infiltrates within the
vessel wall with frequent giant cell formation
There is proliferation
of the intima and fragmentation of the internal elastic lamina
Слайд 17
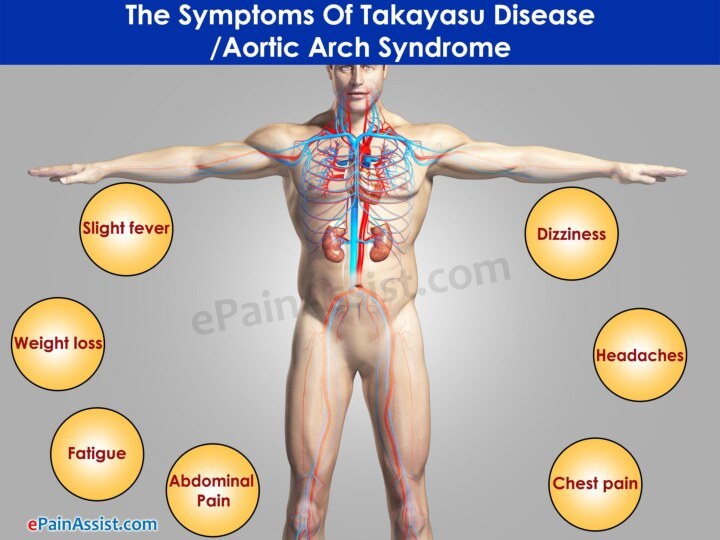
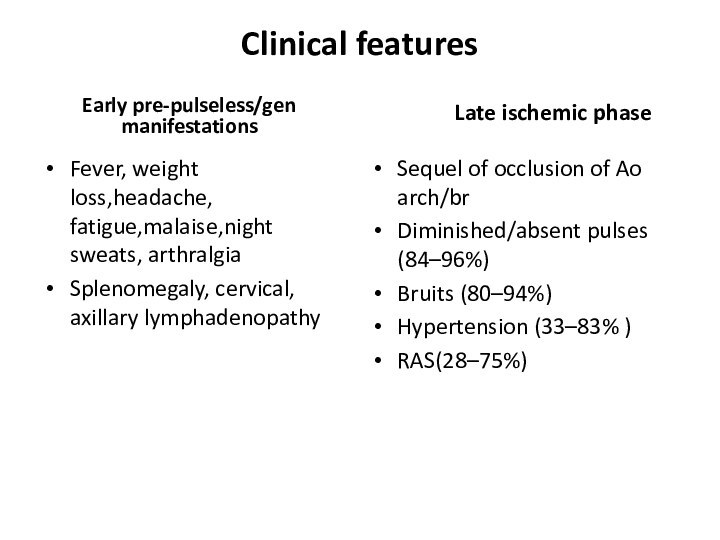
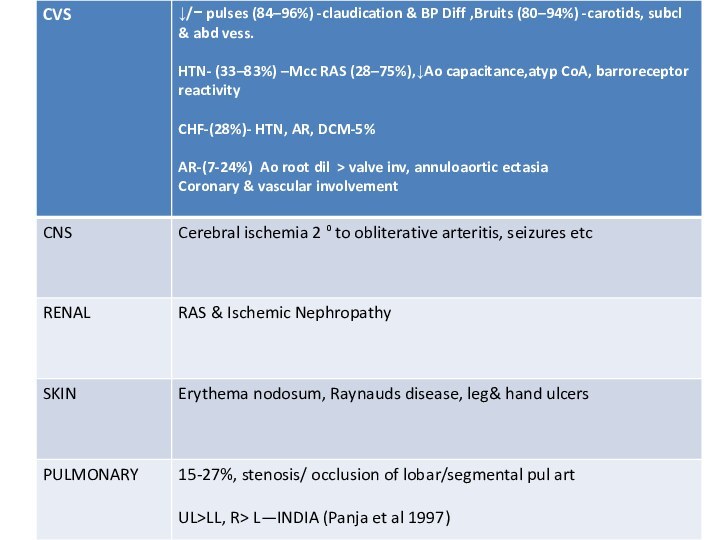
Clinical features
Early pre-pulseless/gen manifestations
Fever, weight loss,headache, fatigue,malaise,night sweats,
arthralgia
Splenomegaly, cervical, axillary lymphadenopathy
Late ischemic phase
Sequel
of occlusion of Ao arch/brDiminished/absent pulses (84–96%)
Bruits (80–94%)
Hypertension (33–83% )
RAS(28–75%)
Слайд 20
Coronary involvement in TA
Occurs in 10~30%
Often fatal
Classified into
3 types
Type1:stenosis or occlusion of coronary ostia
Type2:diffuse or focal
coronary arteritisType3:coronary aneurysm
Слайд 21
Occular involvement
Hypertensive retinopathy
Common
Arteriosclerotic –art narrowing, av nipping,silver wiring
Neuroretinopathy-exudates
and papilloedema
Direct opthalmoscopy
Nonhypertensive retinopathy
UYAMA & ASAYAMA CLASS
stage 1- Dil
of small vesselsstage 2- Microaneurysm
stage 3- Art-ven anastomoses
stage 4- Ocular complications
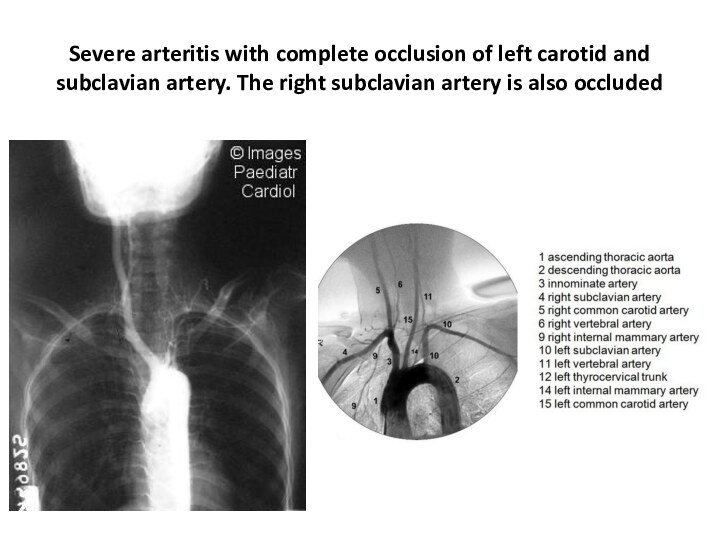
Слайд 24 Severe arteritis with complete occlusion of left carotid
and subclavian artery. The right subclavian artery is also
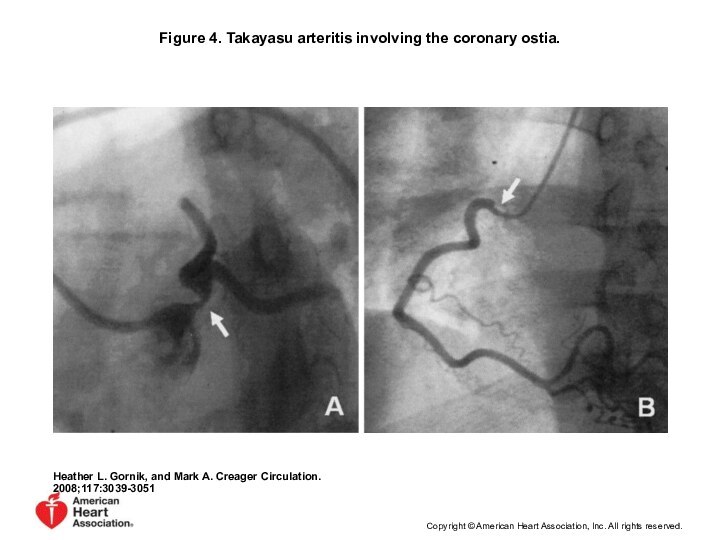
occludedСлайд 27 Figure 4. Takayasu arteritis involving the coronary ostia.
Heather L. Gornik, and Mark A. Creager Circulation. 2008;117:3039-3051
Copyright
© American Heart Association, Inc. All rights reserved.Слайд 28 Figure 3. Aortic occlusive disease in a patient
with Takayasu arteritis and bilateral leg claudication.
Heather L.
Gornik, and Mark A. Creager Circulation. 2008;117:3039-3051Copyright © American Heart Association, Inc. All rights reserved.
Слайд 29 Figure 7. Combination of 18F-FDG PET and CTA
for assessment of Takayasu arteritis.
Heather L. Gornik, and
Mark A. Creager Circulation. 2008;117:3039-3051Copyright © American Heart Association, Inc. All rights reserved.
Слайд 31
a/c phase-Axial T1-weighted image
wall thickening of
As aorta and PA
Axial T1-weighted image- improvement of wall
thickening of As Ao and PA after steroid therapy
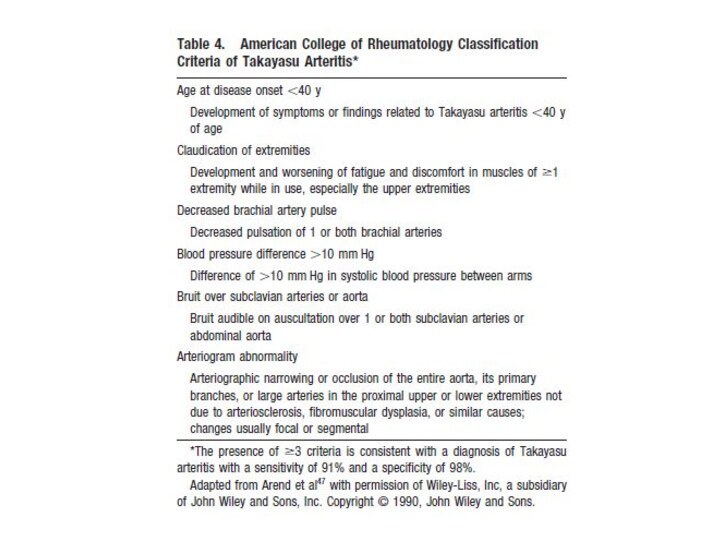
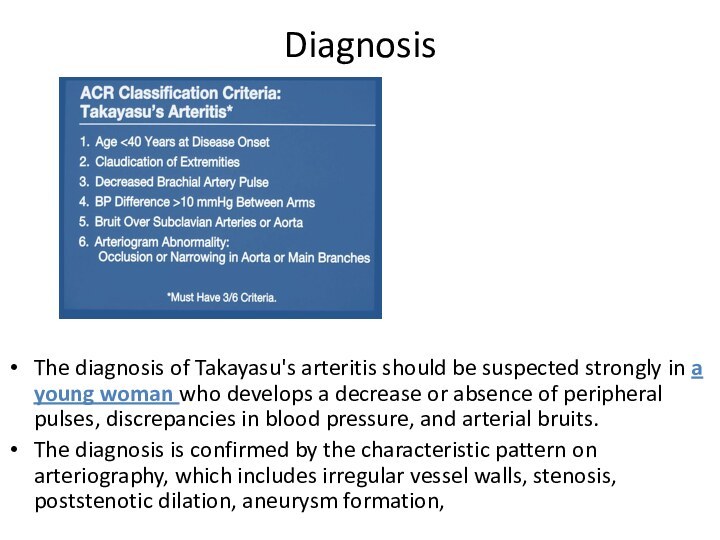
Слайд 33
Diagnosis
The diagnosis of Takayasu's arteritis should be suspected
strongly in a young woman who develops a decrease
or absence of peripheral pulses, discrepancies in blood pressure, and arterial bruits.The diagnosis is confirmed by the characteristic pattern on arteriography, which includes irregular vessel walls, stenosis, poststenotic dilation, aneurysm formation,
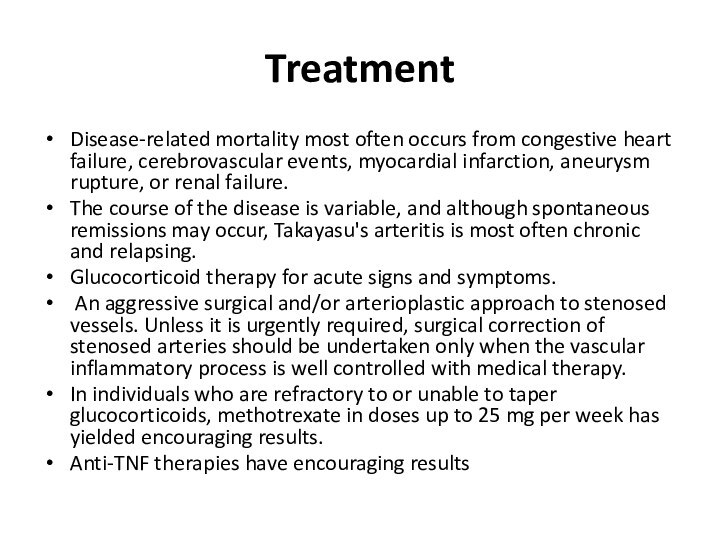
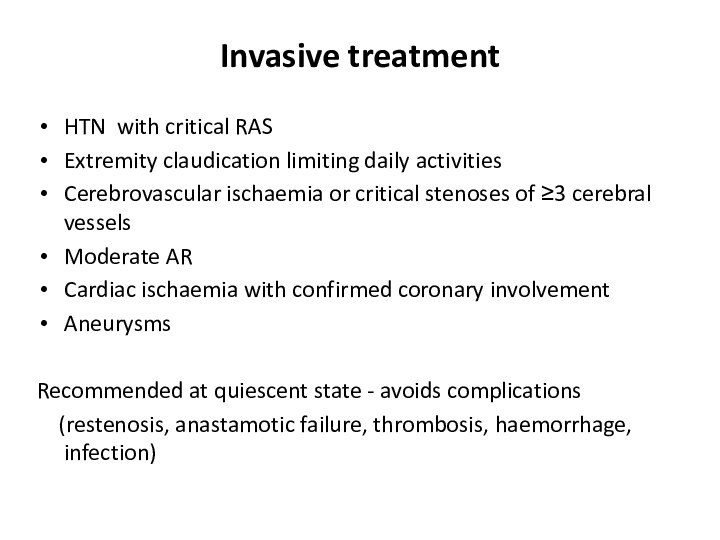
Слайд 34
Treatment
Disease-related mortality most often occurs from congestive
heart failure, cerebrovascular events, myocardial infarction, aneurysm rupture, or
renal failure.The course of the disease is variable, and although spontaneous remissions may occur, Takayasu's arteritis is most often chronic and relapsing.
Glucocorticoid therapy for acute signs and symptoms.
An aggressive surgical and/or arterioplastic approach to stenosed vessels. Unless it is urgently required, surgical correction of stenosed arteries should be undertaken only when the vascular inflammatory process is well controlled with medical therapy.
In individuals who are refractory to or unable to taper glucocorticoids, methotrexate in doses up to 25 mg per week has yielded encouraging results.
Anti-TNF therapies have encouraging results
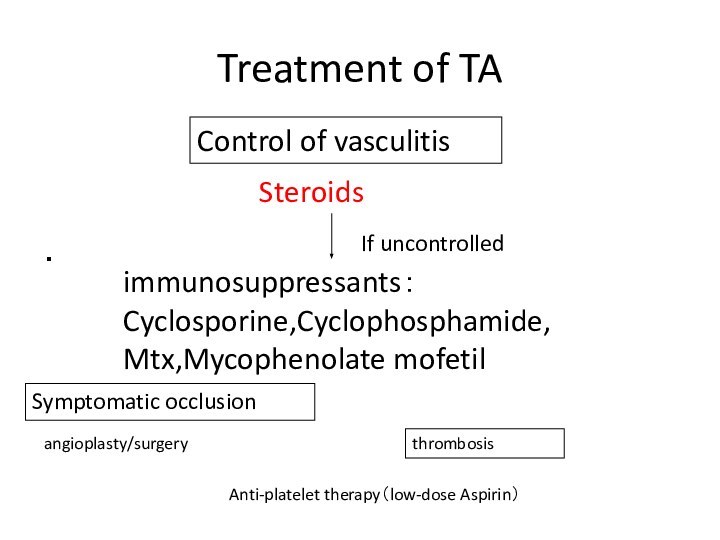
Слайд 35
Treatment of TA
・
Steroids
immunosuppressants:
Cyclosporine,Cyclophosphamide,
Mtx,Mycophenolate mofetil
Anti-platelet therapy(low-dose Aspirin)
angioplasty/surgery
If uncontrolled
Control of
vasculitis
Symptomatic occlusion
thrombosis
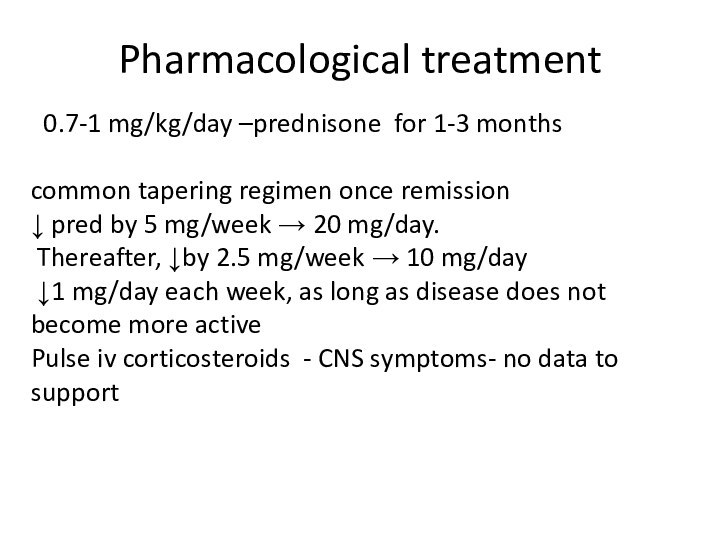
Слайд 36
Pharmacological treatment
0.7-1 mg/kg/day –prednisone for 1-3 months
common
tapering regimen once remission
↓ pred by 5 mg/week →
20 mg/day.Thereafter, ↓by 2.5 mg/week → 10 mg/day
↓1 mg/day each week, as long as disease does not become more active
Pulse iv corticosteroids - CNS symptoms- no data to support
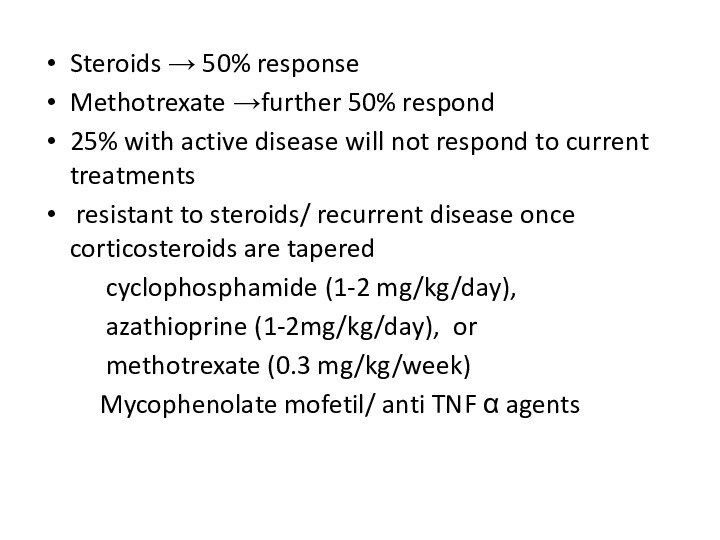
Слайд 37
Steroids → 50% response
Methotrexate →further 50% respond
25% with
active disease will not respond to current treatments
resistant
to steroids/ recurrent disease once corticosteroids are taperedcyclophosphamide (1-2 mg/kg/day),
azathioprine (1-2mg/kg/day), or
methotrexate (0.3 mg/kg/week)
Mycophenolate mofetil/ anti TNF α agents
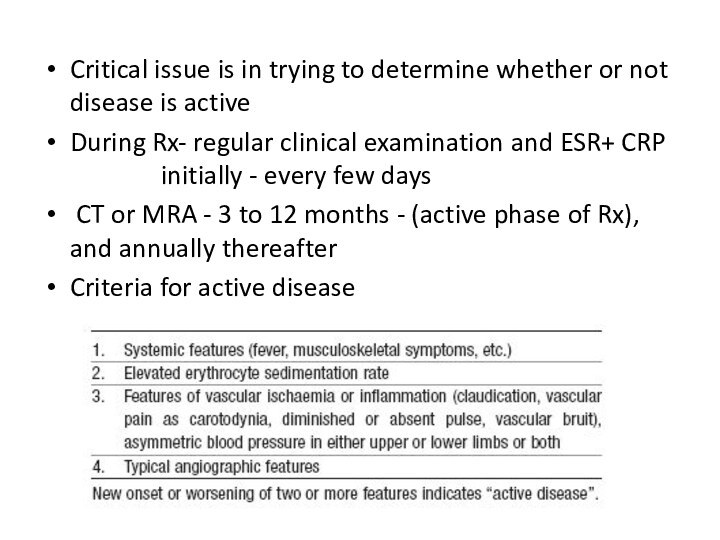
Слайд 38
Critical issue is in trying to determine whether
or not disease is active
During Rx- regular clinical examination
and ESR+ CRP initially - every few daysCT or MRA - 3 to 12 months - (active phase of Rx), and annually thereafter
Criteria for active disease