- Главная
- Разное
- Бизнес и предпринимательство
- Образование
- Развлечения
- Государство
- Спорт
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Религиоведение
- Черчение
- Физкультура
- ИЗО
- Психология
- Социология
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Геометрия
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Что такое findslide.org?
FindSlide.org - это сайт презентаций, докладов, шаблонов в формате PowerPoint.
Обратная связь
Email: Нажмите что бы посмотреть
Презентация на тему Introduction to Psychotic Disorders and Secondary=Organic Psychotic Disorders
Содержание
- 2. מבנה ההרצאהWhat is Psychosis?SymptomsDDX
- 3. PsychosisInability to distinguish between the reality and
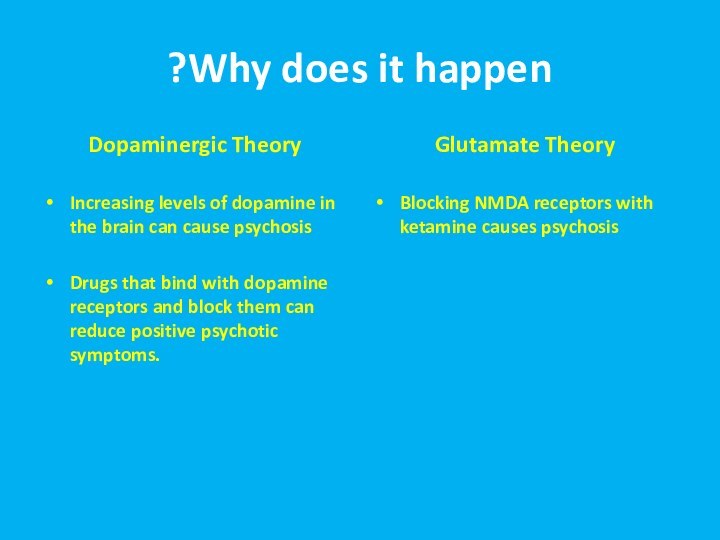
- 5. Why does it happen?Dopaminergic TheoryIncreasing levels of
- 6. סימפטומיםSigns of psychosisHallucinationsDelusionsBizarre or disorganized behaviorImpaired thought processImpaired speech outputAbnormal movements
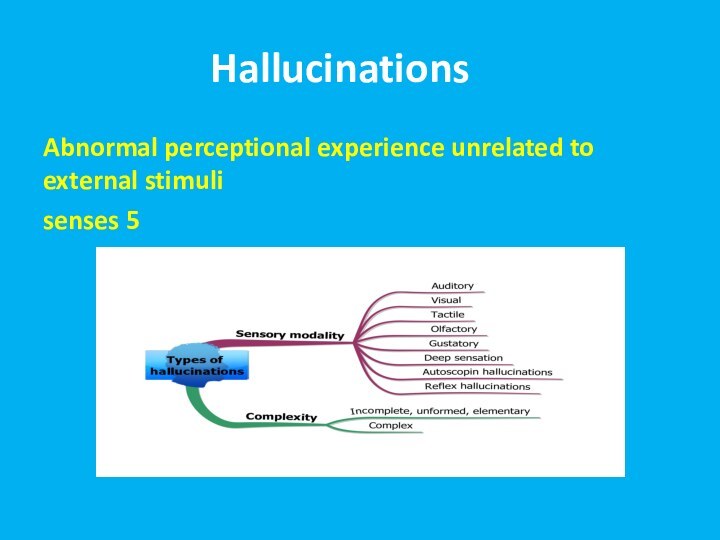
- 7. הזיוHallucinationsתAbnormal perceptional experience unrelated to external stimuli5 senses
- 8. Reasons for HallucinationsPrimary psychiatric disordersBrain pathologySubstancesDisorders of cranial nervesDeliriumDementia
- 9. Auditory HallucinationsPrimary psychotic disorders- human voices, noises,
- 10. Taste HallucinationsUsually epilepsy and brain pathologyVery rare
- 11. Smell HallucinationsUsually epilepsy and brain pathologyRare in
- 12. Somatic and Tactile HallucinationsUsually epilepsy and brain
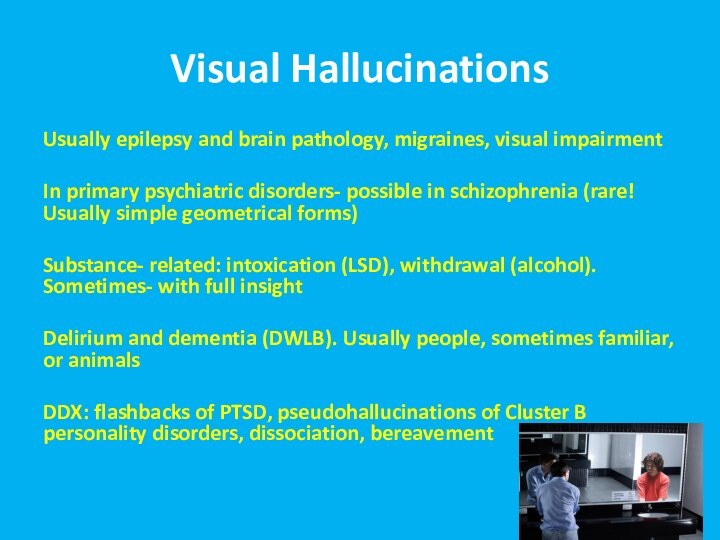
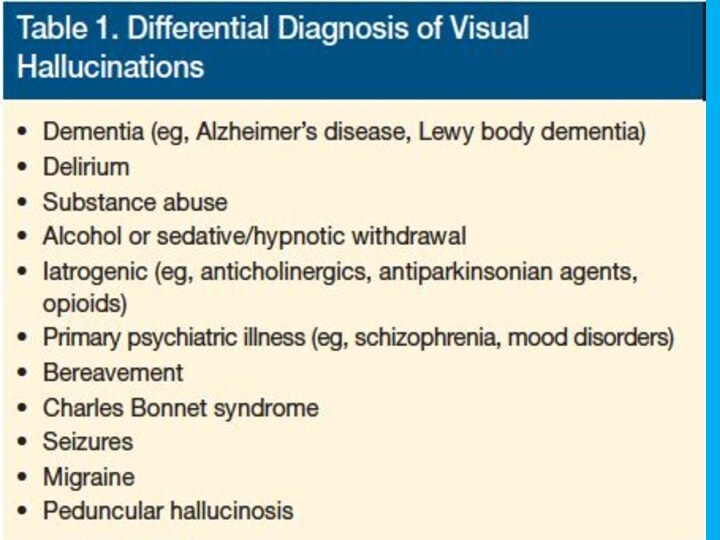
- 13. Visual HallucinationsUsually epilepsy and brain pathology, migraines,
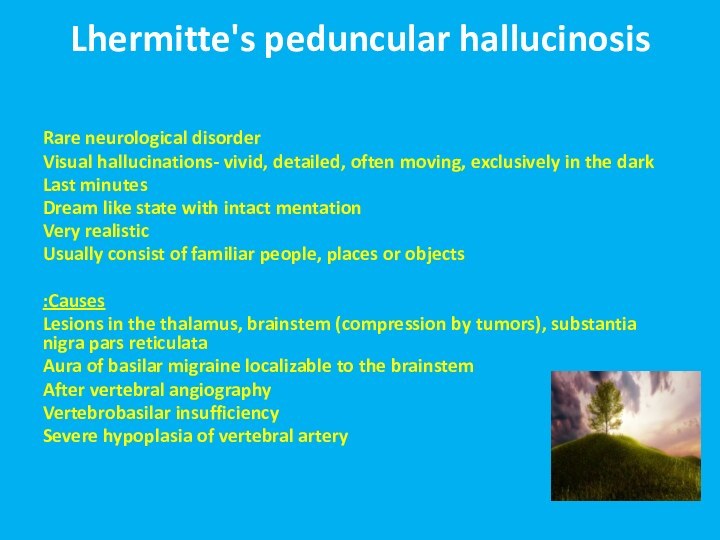
- 15. Lhermitte's peduncular hallucinosisRare neurological disorderVisual hallucinations- vivid,
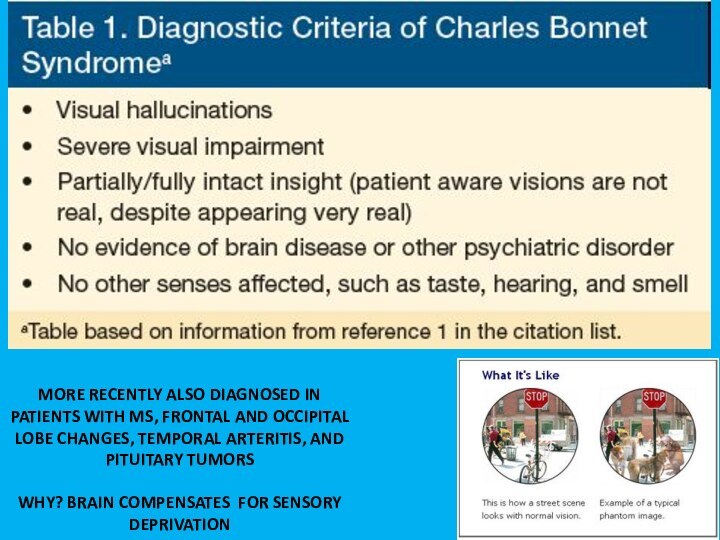
- 16. MORE RECENTLY ALSO DIAGNOSED IN PATIENTS WITH
- 17. Release HallucinationsANY MODALITY BUT VISUAL MOST COMMON:
- 18. Out of Body ExperiencesSleepSubstancesGeneral anesthesiaNeurological disorders
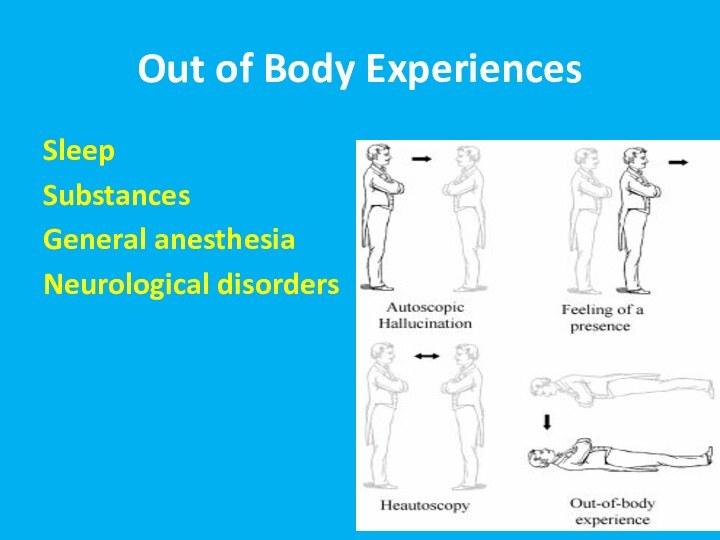
- 19. Autoscopic psychosisThe experience in which an individual
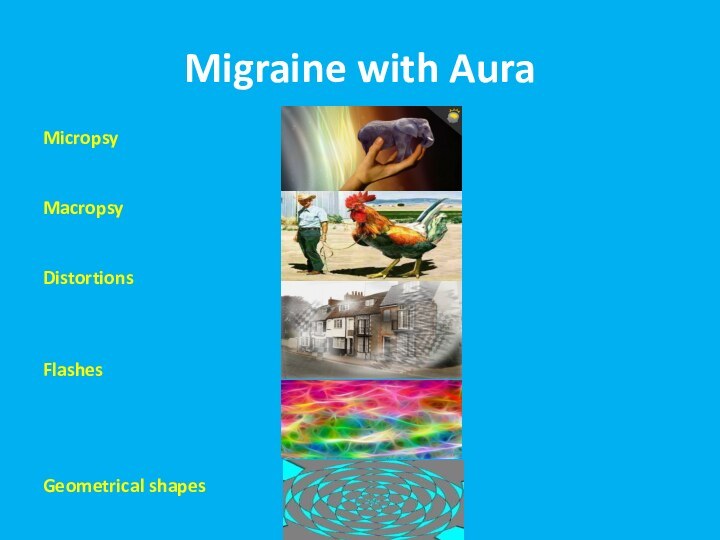
- 20. Migraine with AuraMicropsyMacropsyDistortionsFlashesGeometrical shapes
- 21. Hypnagogic/ Hypnapompic HallucinationsOnly upon falling asleep/ waking upVery commonNormal phenomenon!Seconds to minutesUsually eith full insightNarcolepsyChildren
- 22. Illusions Unrealistic interpretation of realistic stimulusNormal!Common in the dark
- 23. הזיות Substance- Induced Visual ExperiencesHallucinogensIntoxication- stimulants, cocaine, alcoholWithdrawal- alcohol, BZ
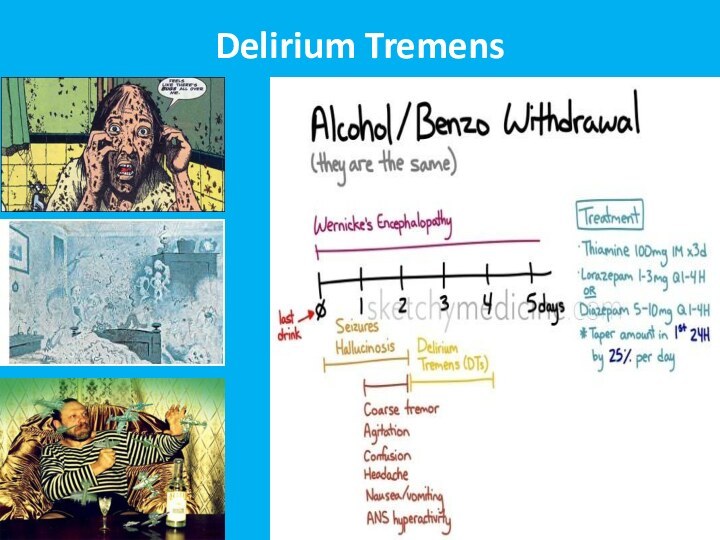
- 24. Delirium Tremens
- 25. Treatment OptionsORGANICALLY BASED HALLUCINATIONS ARE USUALLY SELF-LIMITING.
- 26. DelusionsFalse belief, based on the incorrect interpretation
- 27. Types of DelusionsParanoid/persecutoryIdeas of reference External locus of controlThought broadcastingThought insertion, withdrawalJealousy GuiltGrandiosityReligious delusionsSomatic delusions
- 28. Disorders of ThoughtAlogia (also poverty of speech) – A poverty
- 29. Disorders of ThoughtEcholalia – Echoing of another's speech
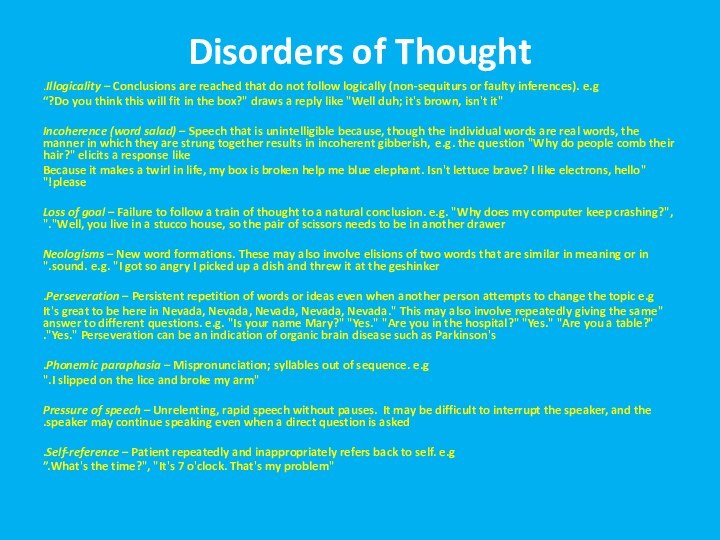
- 30. Disorders of ThoughtIllogicality – Conclusions are reached that
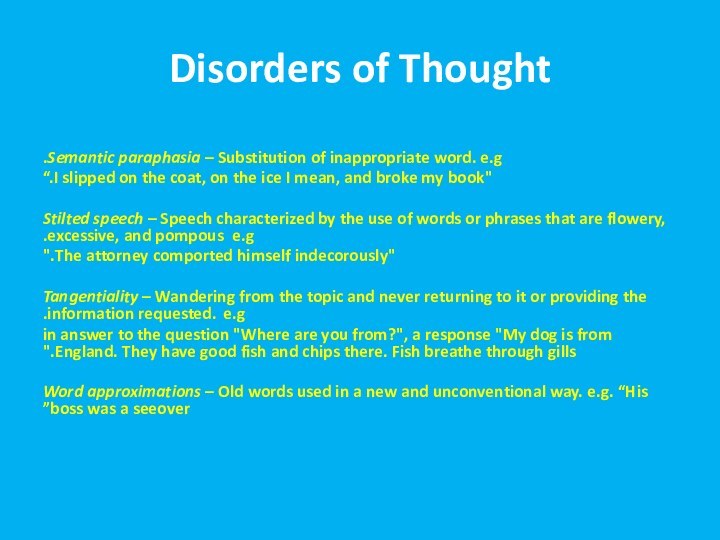
- 31. Disorders of ThoughtSemantic paraphasia – Substitution of inappropriate
- 32. BehaviorBizarre dress and appearanceCatatoniaLoss of impulse controlAggression and extreme irritabilityStereotypic speech and behaviorMannerisms
- 33. CatatoniaStupor (i.e., no psychomotor activity; not actively relating
- 34. Mood and AffectInappropriate affectBlunting of affect/mood
- 35. מצב פסיכוטי פרנואידי- הדגמהMovie
- 36. DDXBasis- primary versus secondary psychosis!
- 37. DDX- Primary PsychosisSchizophrenia, schizophreniformSchizoaffectiveBrief Psychotic disorderDelusional disorderAffective psychosis (depression, mania)
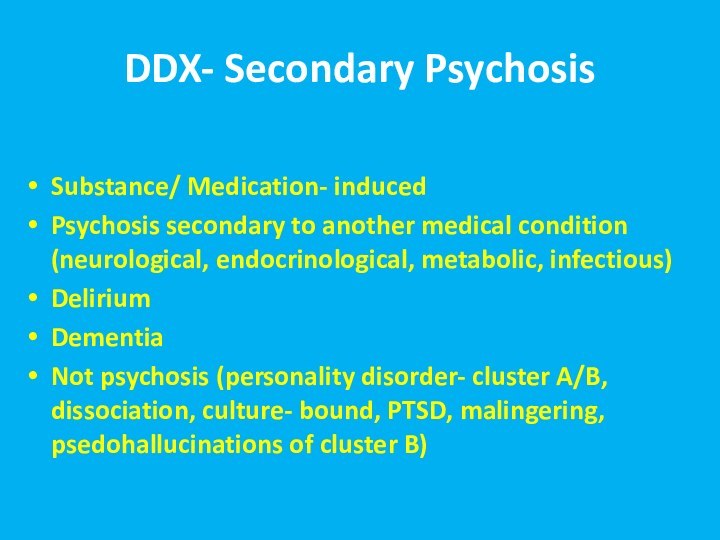
- 38. DDX- Secondary PsychosisSubstance/ Medication- inducedPsychosis secondary to
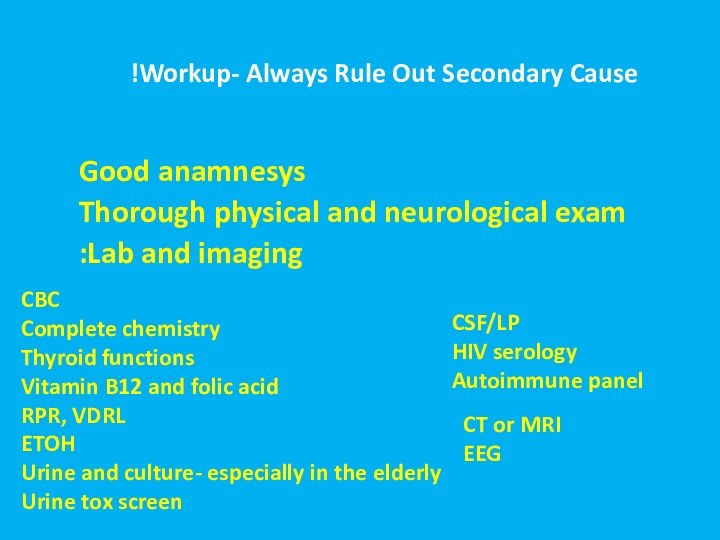
- 39. Workup- Always Rule Out Secondary Cause!"אורגנית"
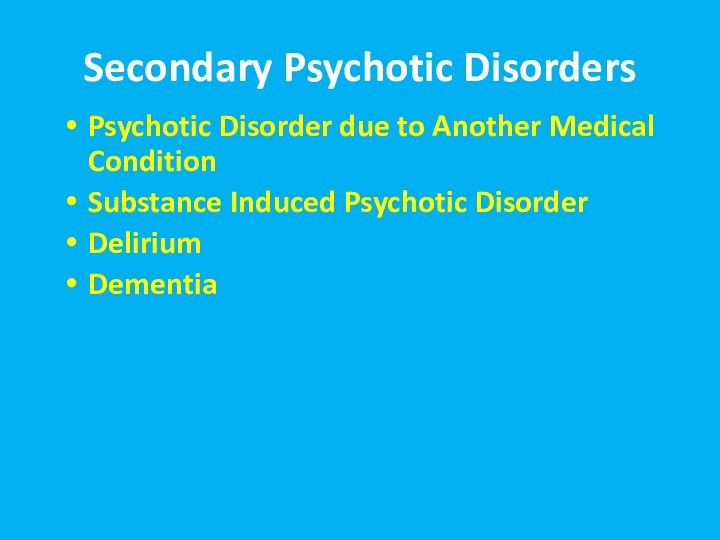
- 40. Secondary Psychotic DisordersPsychotic Disorder due to Another Medical ConditionSubstance Induced Psychotic DisorderDeliriumDementia
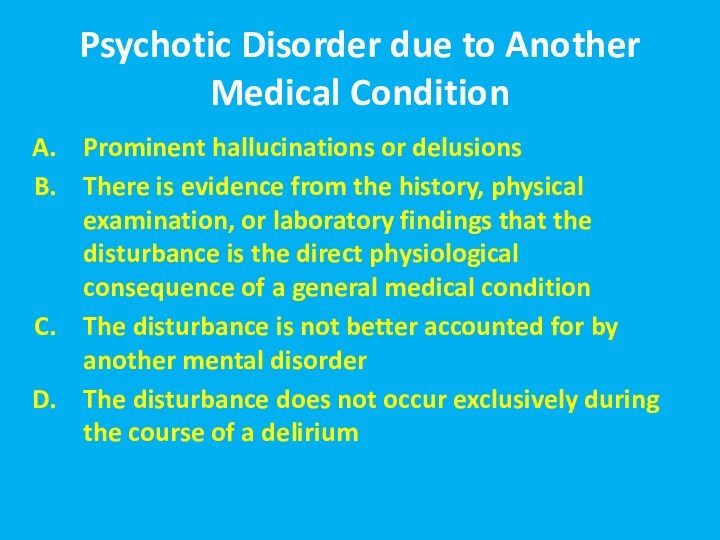
- 41. Psychotic Disorder due to Another Medical ConditionProminent
- 42. Psychotic Disorder due to Another Medical Condition
- 45. Over the counter: Dextromethorphan, cold medicationsOther: Steroids, Bupropion, Dostinex, antibiotics, antivirals, antimalarials
- 47. Delirium15-25% of patients on general medical wards,
- 48. Delirium Perceptual disturbances are common; however, hallucinations
- 49. EtiologiesIn general- delirium etiology =secondary psychosis etiology!Intracranial
- 50. Etiologies cont’dExtracranial causes:
- 51. Etiologies cont’dSystemic InfectionsElectrolyte abnormalitiesPostoperative statesTrauma
- 52. Treatment of DeliriumHigh Potency Antipsychotic+ antihistamineSupportive CareFind and Resolve Causative Factor(s)
- 53. Dementia as the Cause of Psychosis
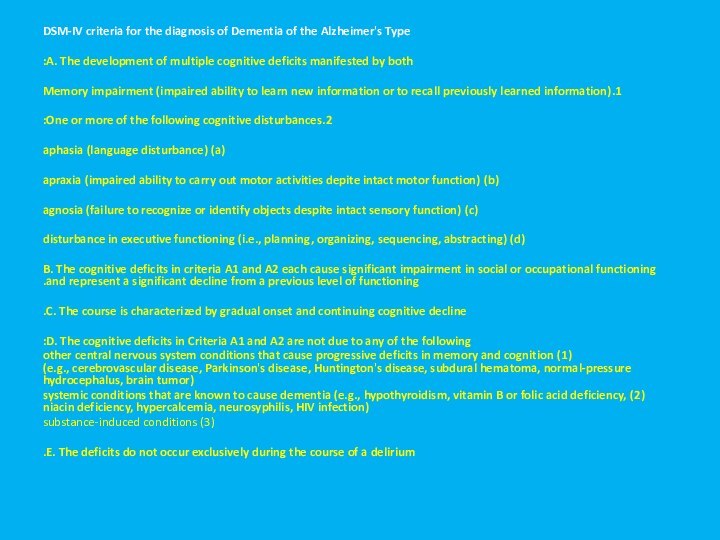
- 54. DSM-IV criteria for the diagnosis of Dementia
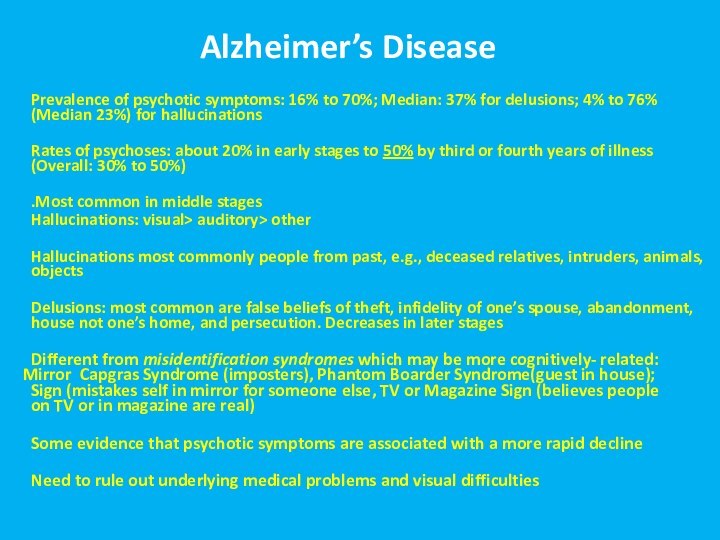
- 55. Alzheimer’s Disease Prevalence of psychotic symptoms: 16% to
- 56. Vascular Dementia Cache County study found
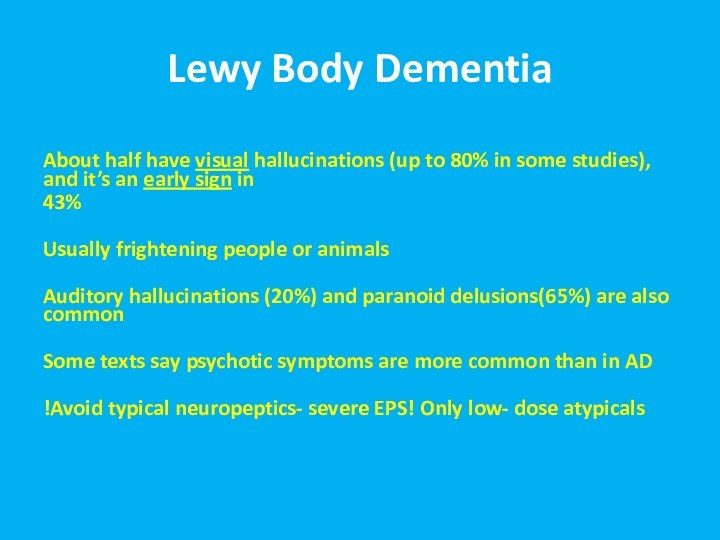
- 57. Lewy Body DementiaAbout half have visual hallucinations
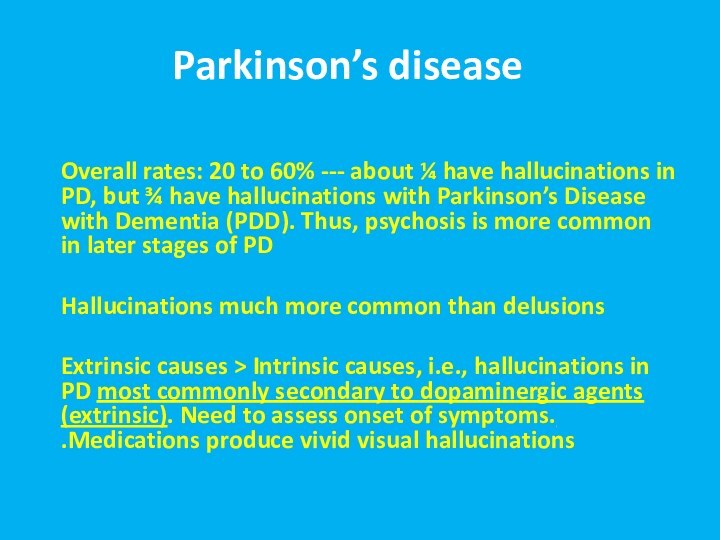
- 58. Parkinson’s disease Overall rates: 20 to 60%
- 59. Test Yourself
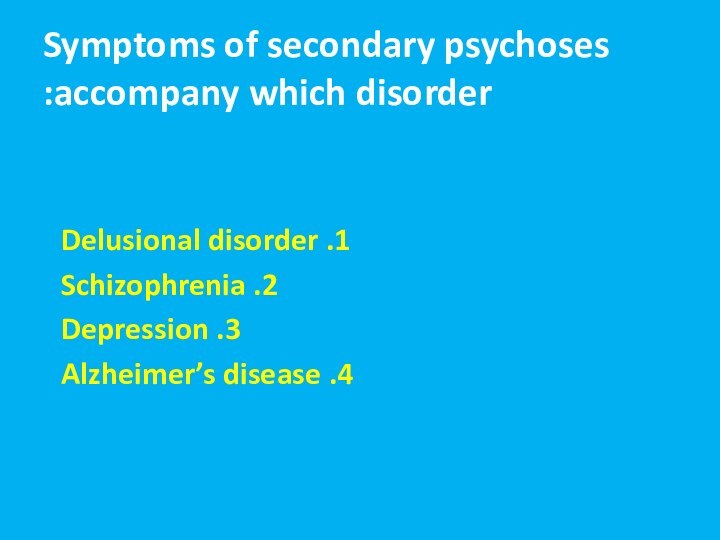
- 60. Symptoms of secondary psychoses accompany which disorder: 1. Delusional disorder2. Schizophrenia3. Depression4. Alzheimer’s disease
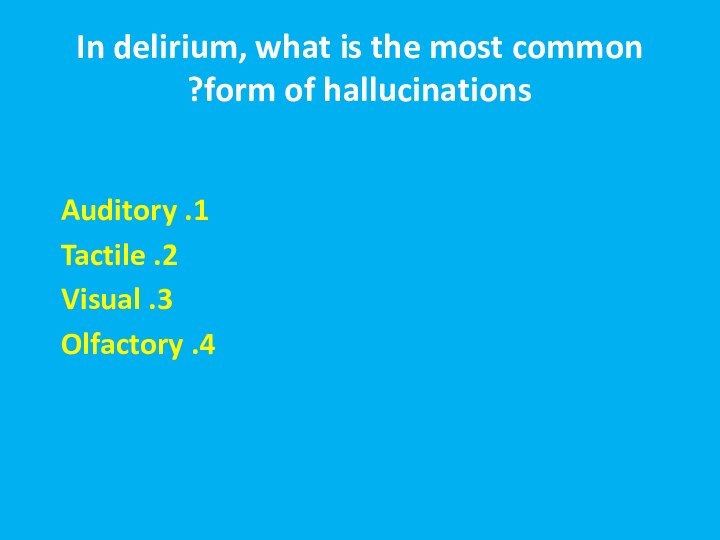
- 61. In delirium, what is the most common form of hallucinations?1. Auditory2. Tactile3. Visual4. Olfactory
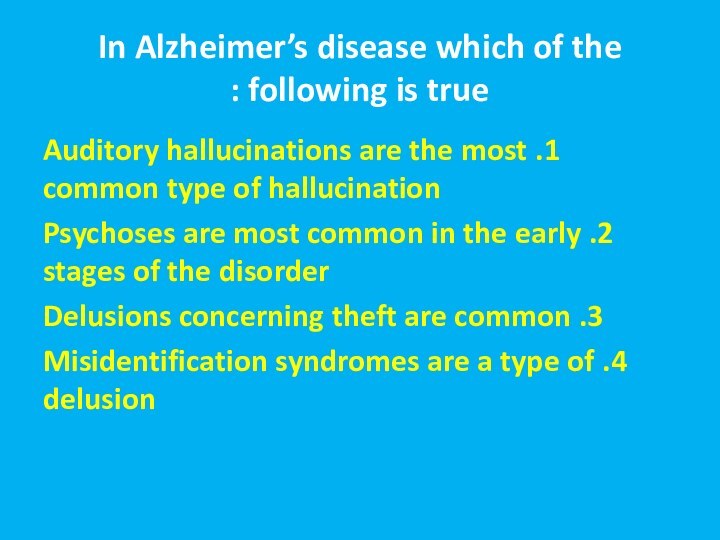
- 62. In Alzheimer’s disease which of the following
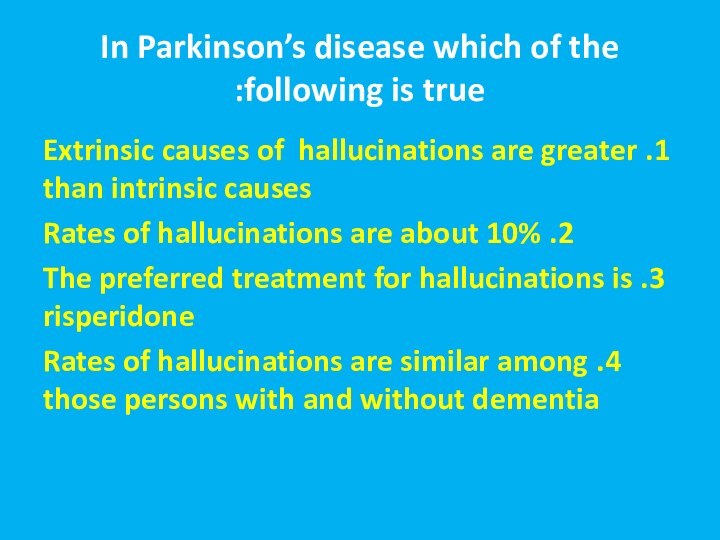
- 63. In Parkinson’s disease which of the following
- 64. Скачать презентацию
- 65. Похожие презентации
מבנה ההרצאהWhat is Psychosis?SymptomsDDX


Слайд 3
Psychosis
Inability to distinguish between the reality and the
inner world and stimuli
testing and behavior, accompanied by hallucinations and/or delusions
Слайд 5
Why does it happen?
Dopaminergic Theory
Increasing levels of dopamine
in the brain can cause psychosis
Drugs that bind with
dopamine receptors and block them can reduce positive psychotic symptoms.Glutamate Theory
Blocking NMDA receptors with ketamine causes psychosis
Слайд 6
סימפטומים
Signs of psychosis
Hallucinations
Delusions
Bizarre or disorganized behavior
Impaired thought process
Impaired
speech output
Abnormal movements
Слайд 8
Reasons for Hallucinations
Primary psychiatric disorders
Brain pathology
Substances
Disorders of cranial
nerves
Delirium
Dementia
Слайд 9
Auditory Hallucinations
Primary psychotic disorders- human voices, noises, command
hallucinations. Usually perceived as coming from outside!
Substances- both intoxication
and withdrawal. All types of voices and noisesCN7 tumors- tinnitus, music, vague noises. Usually perceived as coming from within!
Epilepsy and brain neoplasms- All types of voices and noises
Delirium and dementia- usually unclear voices and unformed phrases
Слайд 10
Taste Hallucinations
Usually epilepsy and brain pathology
Very rare in
primary psychiatric disorders
Do not perceive taste or perceive he
“wrong” taste
Слайд 11
Smell Hallucinations
Usually epilepsy and brain pathology
Rare in primary
psychiatric disorders- possible in psychotic depression and in delusional
disorder (halithosis)Usually- unpleasant smells (decay, burned rubber)
Usually- patients perceive themselves as the source of the smell
Слайд 12
Somatic and Tactile Hallucinations
Usually epilepsy and brain pathology
In
primary psychiatric disorders- possible in delusional disorder (parasitosis)
Substance- related:
intoxication (cocain), withdrawal (alcohol)DDX: peripheral neuropathy
Sense of “electricity”, “bugs crawling”, “worms”, “touch”, change in body shape
Слайд 13
Visual Hallucinations
Usually epilepsy and brain pathology, migraines, visual
impairment
In primary psychiatric disorders- possible in schizophrenia (rare! Usually
simple geometrical forms)Substance- related: intoxication (LSD), withdrawal (alcohol). Sometimes- with full insight
Delirium and dementia (DWLB). Usually people, sometimes familiar, or animals
DDX: flashbacks of PTSD, pseudohallucinations of Cluster B personality disorders, dissociation, bereavement
Слайд 15
Lhermitte's peduncular hallucinosis
Rare neurological disorder
Visual hallucinations- vivid, detailed,
often moving, exclusively in the dark
Last minutes
Dream like state
with intact mentationVery realistic
Usually consist of familiar people, places or objects
Causes:
Lesions in the thalamus, brainstem (compression by tumors), substantia nigra pars reticulata
Aura of basilar migraine localizable to the brainstem
After vertebral angiography
Vertebrobasilar insufficiency
Severe hypoplasia of vertebral artery
Слайд 16
MORE RECENTLY ALSO DIAGNOSED IN PATIENTS WITH MS,
FRONTAL AND OCCIPITAL LOBE CHANGES, TEMPORAL ARTERITIS, AND PITUITARY
TUMORSWHY? BRAIN COMPENSATES FOR SENSORY DEPRIVATION
Слайд 17
Release Hallucinations
ANY MODALITY BUT VISUAL MOST COMMON: DEPENDS
ON END ORGAN AFFECTED
LESIONS ANYWHERE FROM THE EYE TO
THE OCCIPITAL CORTEXUSUALLY REPETITIOUS AND NONTHREATENING BUT IRRITATING
AWARENESS THAT THEY ARE NOT REAL
MODIFIED BY CHANGING VISUAL INPUT
THESE ARE MUCH MORE COMMON THAN THOUGHT AND UNDERREPORTED BECAUSE PEOPLE DO NOT WANT TO BE CONSIDERED “CRAZY.”
Слайд 19
Autoscopic psychosis
The experience in which an individual perceives
the surrounding environment from a different perspective, from a
position outside of his or her own bodyAutoscopic experiences are hallucinations
Experiences - are characterized by the presence of the following three factors:
Disembodiment,
impression of seeing the world from an elevated and distanced visuo-spatial perspective or extracorporeal, but egocentric visuo-spatial perspective;
impression of seeing one's own body from this perspective (autoscopy).
Heautoscopy - reduplicative hallucination of "seeing one's own body at a distance”. It can occur as a symptom in schizophrenia and epilepsy
Polyopic heutoscopy - more than one double is perceived. Can result from a tumor in the insular region of left temporal lobe
Negative autoscopy (or negative heautoscopy) - the sufferer does not see his or her reflection when looking in a mirror
Слайд 21
Hypnagogic/ Hypnapompic Hallucinations
Only upon falling asleep/ waking up
Very
common
Normal phenomenon!
Seconds to minutes
Usually eith full insight
Narcolepsy
Children
Слайд 23
הזיות Substance- Induced Visual Experiences
Hallucinogens
Intoxication- stimulants, cocaine, alcohol
Withdrawal-
alcohol, BZ
Слайд 25
Treatment Options
ORGANICALLY BASED HALLUCINATIONS ARE USUALLY SELF-LIMITING. With
either end organ or central nervous system changes, they
disappear after a few days, months, or years. THE FIRST STEP IS TO REASSURE THE PATIENT.INTERVENTIONS:
CHANGE PATIENT’S ENVIRONMENT
HASTEN END ORGAN CHANGE, E.G., CATARACT REMOVAL
GOOD MEDICAL MANAGEMENT OF CNS RISK FACTORS, E.G., HTN, DM, ET AL.
MEDICATIONS: DO NOT ROUTINELY USE CLASSIC NEUROLEPTICS
PEDUNCULAR HALLUCINOSIS: CLOZAPINE
RELEASE HALLUCINATIONS: CARBAMAZEPINE, GABAPENTIN, MELPERONE, VALPROATE, CISAPRIDE
Слайд 26
Delusions
False belief, based on the incorrect interpretation of
the external reality, not in cultural context, not challengeable
by rational explanations, affects the persons behavior and actions
Слайд 27
Types of Delusions
Paranoid/persecutory
Ideas of reference
External locus of
control
Thought broadcasting
Thought insertion, withdrawal
Jealousy
Guilt
Grandiosity
Religious delusions
Somatic delusions
Слайд 28
Disorders of Thought
Alogia (also poverty of speech) – A poverty of
speech, either in amount or content; it can occur
as a negative symptom of schizophreniaBlocking – An abrupt stop in the middle of a train of thought; the individual may or may not be able to continue theidea. This is a type of formal thought disorder that can be seen in schizophrenia
Circumstantiality (also circumstantial thinking, or circumstantial speech) – An inability to answer a question without giving excessive, unnecessary detail. This differs from tangential thinking, in that the person does eventually return to the original point
Clanging or Clang association – Ideas that are related only by similar or rhyming sounds rather than actual meaning. This may be heard as excessive rhyming and/or alliteration. e.g.
"Many moldy mushrooms merge out of the mildewy mud on Mondays." "I heard the bell. Well, hell, then I fell.“
Derailment (also loose association and knight's move thinking) – Ideas slip off the topic's track on to another which is obliquely related or unrelated .
"The next day when I'd be going out you know, I took control, like uh, I put bleach on my hair in California."
Distractible speech – During mid speech, the subject is changed in response to a stimulus. e.g.
"Then I left San Francisco and moved to... where did you get that tie?"
Слайд 29
Disorders of Thought
Echolalia – Echoing of another's speech that
may only be committed once, or may be continuous
in repetition. This may involve repeating only the last few words or last word of the examiner's sentences. This can be a symptom of Tourette's Syndrome. e.g."What would you like for dinner?", "That's a good question. That's a good question. That's a good question. That's a good question."
Evasive interaction – Attempts to express ideas and/or feelings about another individual come out as evasive or in a diluted form, e.g.:
"I... er ah... you are uh... I think you have... uh-- acceptable erm... uh... hair.“
Flight of ideas – Excessive speech at a rapid rate that involves fragmented or unrelated ideas. It is common in mania. "His boss was a wheelchair"
Слайд 30
Disorders of Thought
Illogicality – Conclusions are reached that do
not follow logically (non-sequiturs or faulty inferences). e.g.
"Do you
think this will fit in the box?" draws a reply like "Well duh; it's brown, isn't it?“Incoherence (word salad) – Speech that is unintelligible because, though the individual words are real words, the manner in which they are strung together results in incoherent gibberish, e.g. the question "Why do people comb their hair?" elicits a response like
"Because it makes a twirl in life, my box is broken help me blue elephant. Isn't lettuce brave? I like electrons, hello please!"
Loss of goal – Failure to follow a train of thought to a natural conclusion. e.g. "Why does my computer keep crashing?", "Well, you live in a stucco house, so the pair of scissors needs to be in another drawer."
Neologisms – New word formations. These may also involve elisions of two words that are similar in meaning or in sound. e.g. "I got so angry I picked up a dish and threw it at the geshinker."
Perseveration – Persistent repetition of words or ideas even when another person attempts to change the topic e.g.
"It's great to be here in Nevada, Nevada, Nevada, Nevada, Nevada." This may also involve repeatedly giving the same answer to different questions. e.g. "Is your name Mary?" "Yes." "Are you in the hospital?" "Yes." "Are you a table?" "Yes." Perseveration can be an indication of organic brain disease such as Parkinson's.
Phonemic paraphasia – Mispronunciation; syllables out of sequence. e.g.
"I slipped on the lice and broke my arm."
Pressure of speech – Unrelenting, rapid speech without pauses. It may be difficult to interrupt the speaker, and the speaker may continue speaking even when a direct question is asked.
Self-reference – Patient repeatedly and inappropriately refers back to self. e.g.
"What's the time?", "It's 7 o'clock. That's my problem.”
Слайд 31
Disorders of Thought
Semantic paraphasia – Substitution of inappropriate word.
e.g.
"I slipped on the coat, on the ice I
mean, and broke my book.“Stilted speech – Speech characterized by the use of words or phrases that are flowery, excessive, and pompous e.g.
"The attorney comported himself indecorously."
Tangentiality – Wandering from the topic and never returning to it or providing the information requested. e.g.
in answer to the question "Where are you from?", a response "My dog is from England. They have good fish and chips there. Fish breathe through gills."
Word approximations – Old words used in a new and unconventional way. e.g. “His boss was a seeover”
Слайд 32
Behavior
Bizarre dress and appearance
Catatonia
Loss of impulse control
Aggression and
extreme irritability
Stereotypic speech and behavior
Mannerisms
Слайд 33
Catatonia
Stupor (i.e., no psychomotor activity; not actively relating to
environment)
Catalepsy (i.e., passive induction of a posture held against gravity)
Waxy
flexibility (i.e., slight, even resistance to positioning by examiner)Mutism (i.e., no, or very little, verbal response [exclude if known aphasia])
Negativism (i.e., opposition or no response to instructions or external stimuli)
Posturing (i.e., spontaneous and active maintenance of a posture against gravity)
Mannerism (i.e., odd, circumstantial caricature of normal actions)
Stereotypy (i.e., repetitive, abnormally frequent, non-goal-directed movements)
Agitation, not influenced by external stimuli
Grimacing
Echolalia (i.e., mimicking another's speech)
Echopraxia (i.e., mimicking another's movements)
Слайд 37
DDX- Primary Psychosis
Schizophrenia, schizophreniform
Schizoaffective
Brief Psychotic disorder
Delusional disorder
Affective psychosis
(depression, mania)
Слайд 38
DDX- Secondary Psychosis
Substance/ Medication- induced
Psychosis secondary to another
medical condition (neurological, endocrinological, metabolic, infectious)
Delirium
Dementia
Not psychosis (personality disorder-
cluster A/B, dissociation, culture- bound, PTSD, malingering, psedohallucinations of cluster B)
Слайд 39
Workup- Always Rule Out Secondary Cause!"אורגנית"
Good
anamnesys
Thorough physical and neurological exam
Lab and imaging:
CBC
Complete chemistry
Thyroid functions
Vitamin
B12 and folic acidRPR, VDRL
ETOH
Urine and culture- especially in the elderly
Urine tox screen
CSF/LP
HIV serology
Autoimmune panel
CT or MRI
EEG
Слайд 40
Secondary Psychotic Disorders
Psychotic Disorder due to Another Medical
Condition
Substance Induced Psychotic Disorder
Delirium
Dementia
Слайд 41
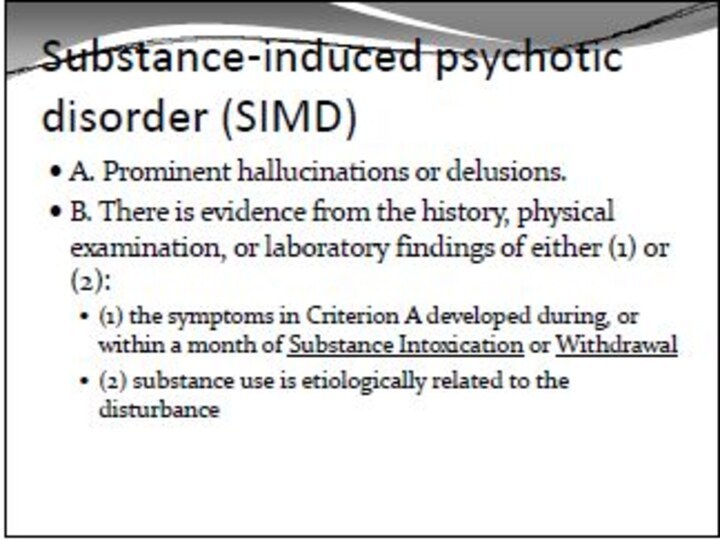
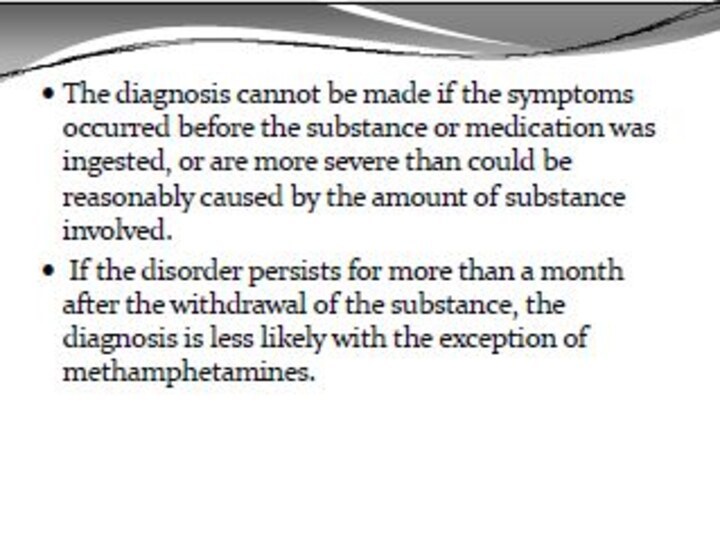
Psychotic Disorder due to Another Medical Condition
Prominent hallucinations
or delusions
There is evidence from the history, physical examination,
or laboratory findings that the disturbance is the direct physiological consequence of a general medical conditionThe disturbance is not better accounted for by another mental disorder
The disturbance does not occur exclusively during the course of a delirium
Слайд 42
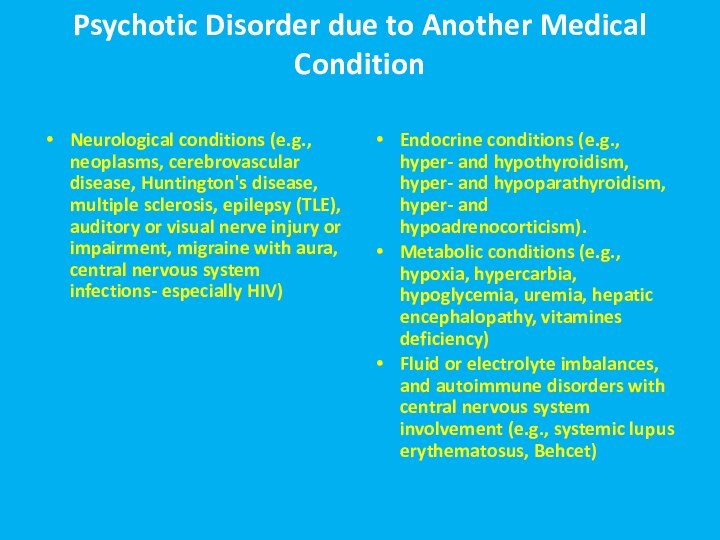
Psychotic Disorder due to Another Medical Condition
Neurological conditions
(e.g., neoplasms, cerebrovascular disease, Huntington's disease, multiple sclerosis, epilepsy
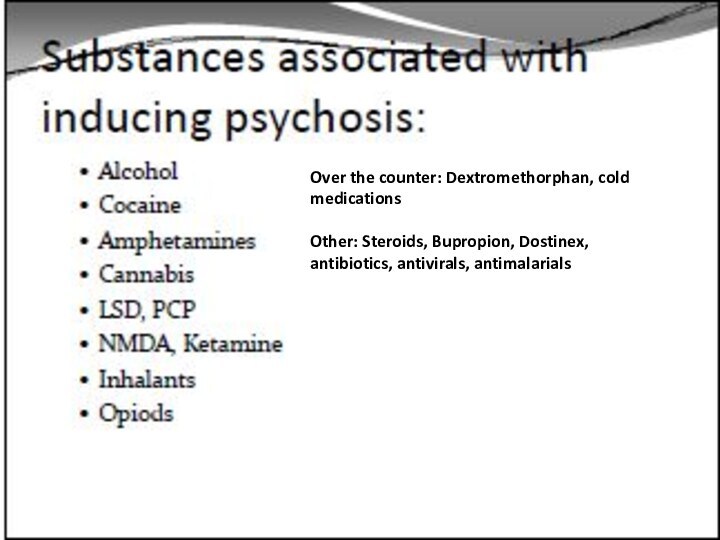
(TLE), auditory or visual nerve injury or impairment, migraine with aura, central nervous system infections- especially HIV)Endocrine conditions (e.g., hyper- and hypothyroidism, hyper- and hypoparathyroidism, hyper- and hypoadrenocorticism).
Metabolic conditions (e.g., hypoxia, hypercarbia, hypoglycemia, uremia, hepatic encephalopathy, vitamines deficiency)
Fluid or electrolyte imbalances, and autoimmune disorders with central nervous system involvement (e.g., systemic lupus erythematosus, Behcet)
Слайд 45
Over the counter: Dextromethorphan, cold medications
Other: Steroids, Bupropion,
Dostinex, antibiotics, antivirals, antimalarials
Слайд 47
Delirium
15-25% of patients on general medical wards, S/P
surgery- even higher percentages
Advanced age, any brain disorder and
underlying dementia are risk 1 yr mortality rate for those w/ episode of delirium= up to 50%!
Recognizing and treating delirium is a medical urgency
Слайд 48
Delirium
Perceptual disturbances are common; however, hallucinations also
are frequent:
Hallucinations: 40% to 67%
Delusions: 25% to 50%
Psychotic
symptoms are more commonly seen with hyperactive rather than hypoactive deliriumVisual > > auditory> other hallucinations
Paranoid delusions are the most common delusions
Clinical evaluation should help identify; dementia and delirium are often related
Слайд 49
Etiologies
In general- delirium etiology =secondary psychosis etiology!
Intracranial Causes:
Seizures and Postictal states Brain Trauma Neoplasms Infections Vascular Disorders (Vasculitis, CVA’s etc.)
Слайд 50
Etiologies cont’d
Extracranial causes:
Drugs/Medications- toxicity, intoxication, and w/d.
Poisons (Carbon Monoxide, Heavy metals) Endocrine dysfunction
Liver dz, Kidney failure, Cardiac failure, Arrhythmias, Hypotension, Hypoxia Deficiency dz’s
Слайд 52
Treatment of Delirium
High Potency Antipsychotic+ antihistamine
Supportive Care
Find and
Resolve Causative Factor(s)
Слайд 54 DSM-IV criteria for the diagnosis of Dementia of
the Alzheimer's Type
A. The development of multiple cognitive deficits
manifested by both:1.Memory impairment (impaired ability to learn new information or to recall previously learned information)
2.One or more of the following cognitive disturbances:
(a) aphasia (language disturbance)
(b) apraxia (impaired ability to carry out motor activities depite intact motor function)
(c) agnosia (failure to recognize or identify objects despite intact sensory function)
(d) disturbance in executive functioning (i.e., planning, organizing, sequencing, abstracting)
B. The cognitive deficits in criteria A1 and A2 each cause significant impairment in social or occupational functioning and represent a significant decline from a previous level of functioning.
C. The course is characterized by gradual onset and continuing cognitive decline.
D. The cognitive deficits in Criteria A1 and A2 are not due to any of the following:
(1) other central nervous system conditions that cause progressive deficits in memory and cognition (e.g., cerebrovascular disease, Parkinson's disease, Huntington's disease, subdural hematoma, normal-pressure hydrocephalus, brain tumor)
(2) systemic conditions that are known to cause dementia (e.g., hypothyroidism, vitamin B or folic acid deficiency, niacin deficiency, hypercalcemia, neurosyphilis, HIV infection)
(3) substance-induced conditions
E. The deficits do not occur exclusively during the course of a delirium.
Слайд 55
Alzheimer’s Disease
Prevalence of psychotic symptoms: 16% to 70%;
Median: 37% for delusions; 4% to 76% (Median 23%)
for hallucinationsRates of psychoses: about 20% in early stages to 50% by third or fourth years of illness (Overall: 30% to 50%)
Most common in middle stages.
Hallucinations: visual> auditory> other
Hallucinations most commonly people from past, e.g., deceased relatives, intruders, animals, objects
Delusions: most common are false beliefs of theft, infidelity of one’s spouse, abandonment, house not one’s home, and persecution. Decreases in later stages
Different from misidentification syndromes which may be more cognitively- related: Capgras Syndrome (imposters), Phantom Boarder Syndrome(guest in house); Mirror Sign (mistakes self in mirror for someone else, TV or Magazine Sign (believes people on TV or in magazine are real)
Some evidence that psychotic symptoms are associated with a more rapid decline
Need to rule out underlying medical problems and visual difficulties
Слайд 56
Vascular Dementia
Cache County study found prevalence
of hallucinations similar between AD and VaD, but delusions
were higher in AD (23% vs 8%)
Слайд 57
Lewy Body Dementia
About half have visual hallucinations (up
to 80% in some studies), and it’s an early
sign in43%
Usually frightening people or animals
Auditory hallucinations (20%) and paranoid delusions(65%) are also common
Some texts say psychotic symptoms are more common than in AD
Avoid typical neuropeptics- severe EPS! Only low- dose atypicals!
Слайд 58
Parkinson’s disease
Overall rates: 20 to 60% ---
about ¼ have hallucinations in PD, but ¾ have
hallucinations with Parkinson’s Disease with Dementia (PDD). Thus, psychosis is more common in later stages of PDHallucinations much more common than delusions
Extrinsic causes > Intrinsic causes, i.e., hallucinations in PD most commonly secondary to dopaminergic agents (extrinsic). Need to assess onset of symptoms. Medications produce vivid visual hallucinations.
Слайд 60
Symptoms of secondary psychoses accompany which disorder:
1.
Delusional disorder
2. Schizophrenia
3. Depression
4. Alzheimer’s disease
Слайд 61 In delirium, what is the most common form
of hallucinations?
1. Auditory
2. Tactile
3. Visual
4. Olfactory
Слайд 62 In Alzheimer’s disease which of the following is
true :
1. Auditory hallucinations are the most common type
of hallucination2. Psychoses are most common in the early stages of the disorder
3. Delusions concerning theft are common
4. Misidentification syndromes are a type of delusion
Слайд 63 In Parkinson’s disease which of the following is
true:
1. Extrinsic causes of hallucinations are greater than intrinsic
causes2. Rates of hallucinations are about 10%
3. The preferred treatment for hallucinations is risperidone
4. Rates of hallucinations are similar among those persons with and without dementia