- Главная
- Разное
- Бизнес и предпринимательство
- Образование
- Развлечения
- Государство
- Спорт
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Религиоведение
- Черчение
- Физкультура
- ИЗО
- Психология
- Социология
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Геометрия
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Что такое findslide.org?
FindSlide.org - это сайт презентаций, докладов, шаблонов в формате PowerPoint.
Обратная связь
Email: Нажмите что бы посмотреть
Презентация на тему Prophylaxis of tuberculosis. (Lecture 4)
Содержание
- 2. Prophylaxis of tuberculosis: Social, Infectious control, Sanitary, BCG vaccination,Preventive Chemotherapy
- 3. Social prophylaxisPrinciples of prophylactic orientation, state character,
- 4. A social prophylaxis is directed on:making healthy
- 5. BCG VACCINEattenuated (virulence-reduced) live bovine tuberculosis bacillus,
- 6. Because the living bacilli evolve to make
- 7. Microscopic image of the Calmette-Guérin bacillus, Ziehl–Neelsen stain, magnification:1,000
- 8. The bacille Calmette-Guérin (BCG) vaccine has existed
- 9. The biological interaction between MTB and the
- 10. RECOMBINANT BCG VACCINE
- 11. is used for active specific prophylaxis of
- 12. BCG-M vaccine is manufactured in a half
- 13. BCG-STRAINSThere have been many (WHO estimated 40
- 14. when the vaccine had been administered in
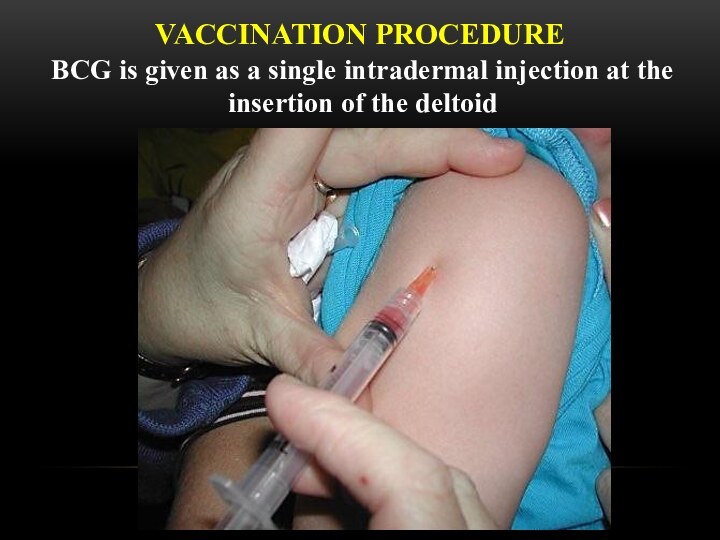
- 15. VACCINATION PROCEDUREBCG is given as a single intradermal injection at the insertion of the deltoid
- 16. THE RULES OF TRANSFUSION
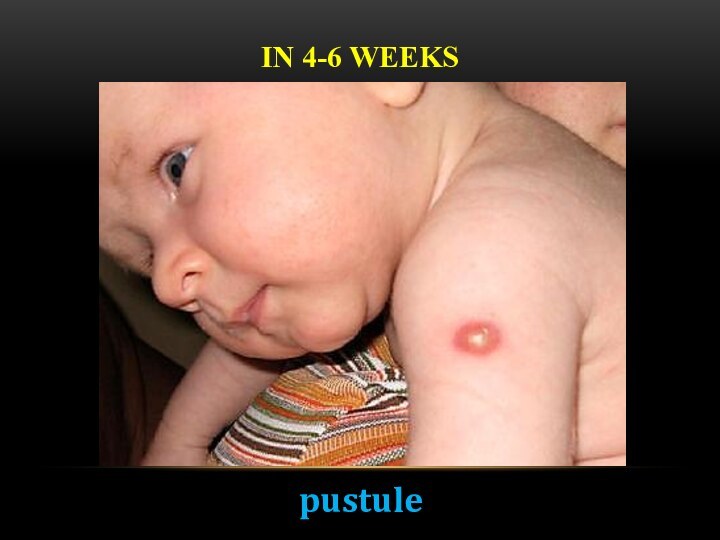
- 17. IN 4-6 WEEKSpustule
- 18. IN 6-8 WEEKScrust
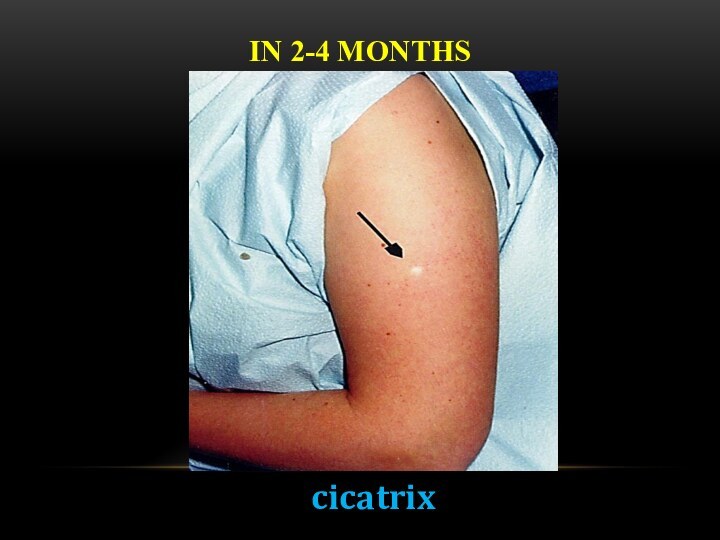
- 19. IN 2-4 MONTHScicatrix
- 20. BCG IN ADOLESCENTS AND ADULTSThere is no
- 21. BCG IN HIV-INFECTED NEWBORNSIn children who are
- 22. COMPLICATIONS (BCG-RELATED DISEASES) CLASSIFICATION (WHO, 1984) Local
- 23. The term "BCG lymphadenitis" is usually coined
- 24. There are two forms of BCG lymphadenitis.The
- 25. Overlying skin changes is universal, with erythema,
- 26. BCG LYMPHADENITISThree treatment options have been described
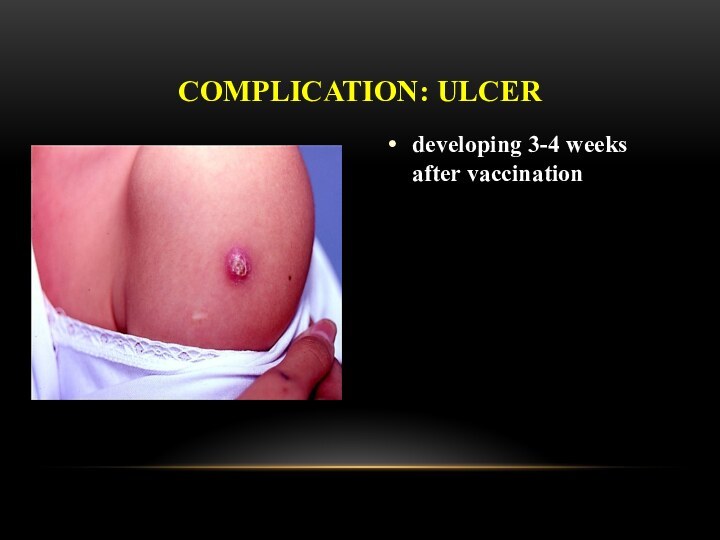
- 27. developing 3-4 weeks after vaccinationCOMPLICATION: ULCER
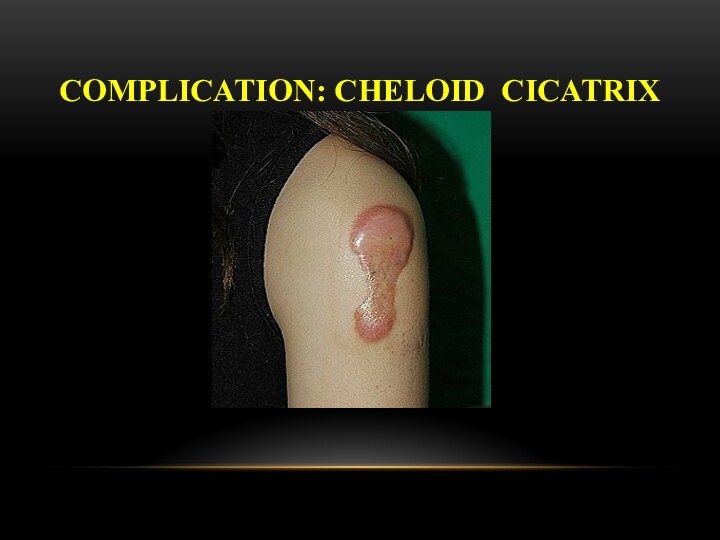
- 28. COMPLICATION: CHELOID CICATRIX
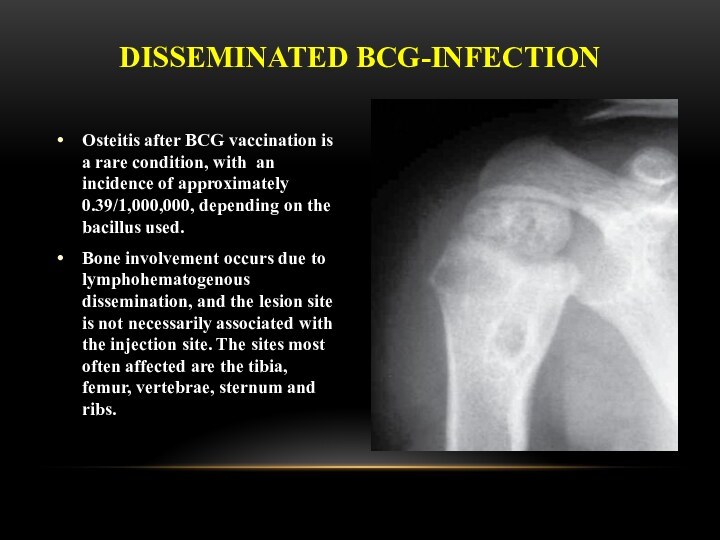
- 29. Osteitis after BCG vaccination is a rare
- 30. Clinical manifestations usually occur 18 months
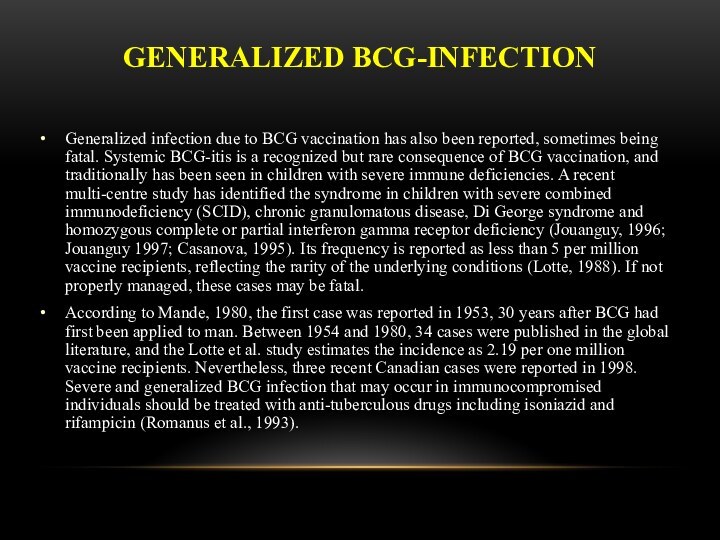
- 31. GENERALIZED BCG-INFECTIONGeneralized infection due to BCG vaccination
- 32. LATENT TB INFECTIONLatent tuberculosis infection (LTBI) is
- 33. PREVENTIVE CHEMOTHERAPYGuidelines on the management of latent
- 34. PREVENTIVE CHEMOTHERAPYSystematic testing and treatment of LTBI
- 35. PREVENTIVE CHEMOTHERAPYSystematic testing and treatment of LTBI
- 36. PREVENTIVE CHEMOTHERAPYSystematic testing for LTBI is not
- 37. PREVENTIVE CHEMOTHERAPYIndividuals should be asked about symptoms
- 38. PREVENTIVE CHEMOTHERAPYEither TST or IGRA can be
- 39. FOR RESOURCE-LIMITED COUNTRIES AND OTHER MIDDLE-INCOME COUNTRIES
- 40. PREVENTIVE CHEMOTHERAPYTreatment options recommended for LTBI include:
- 41. MDR-TB CASESStrict clinical observation and close monitoring
- 42. RISK OF DRUG RESISTANCE FOLLOWING LTBI TREATMENTA
- 43. INFECTION CONTROL OF TUBERCULOSIS
- 44. EMPHASISE THAT TRANSMISSION IS NOT ONE-WAY AND
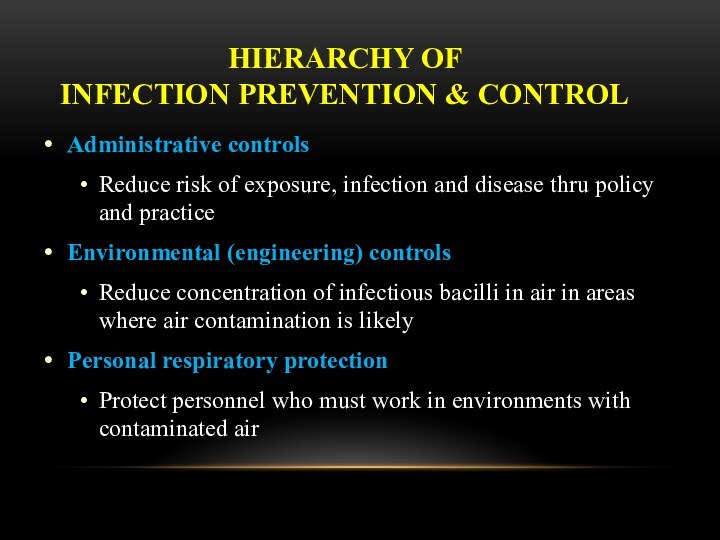
- 45. HIERARCHY OF INFECTION PREVENTION & CONTROLAdministrative
- 46. ADMINISTRATIVE CONTROLSDevelop and implement written policies and
- 47. ENVIRONMENTAL CONTROLS: VENTILATION AND AIR FLOWVentilation
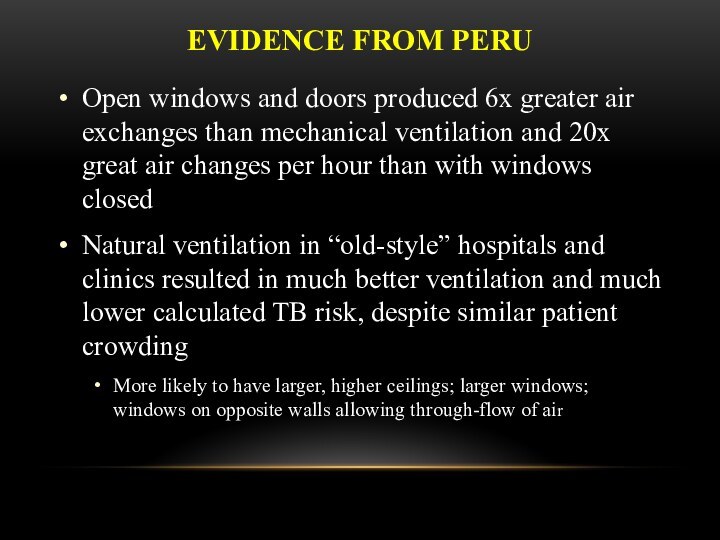
- 48. EVIDENCE FROM PERUOpen windows and doors produced
- 49. ESTIMATED RISK OF AIRBORNE TB INFECTIONNaturally
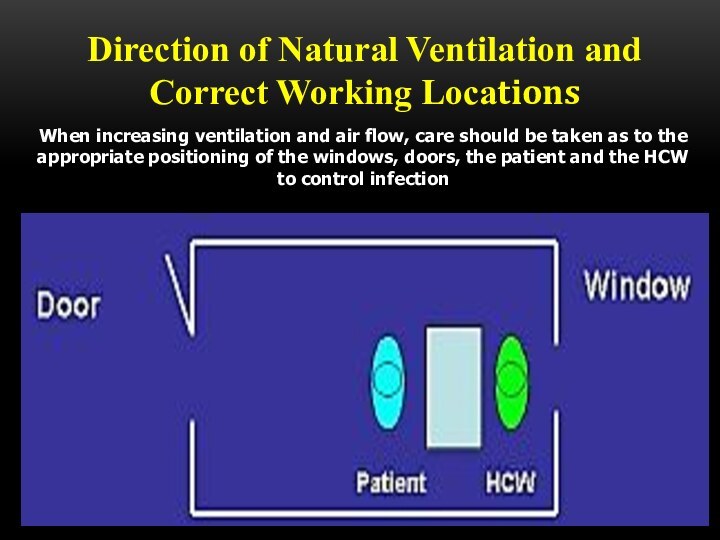
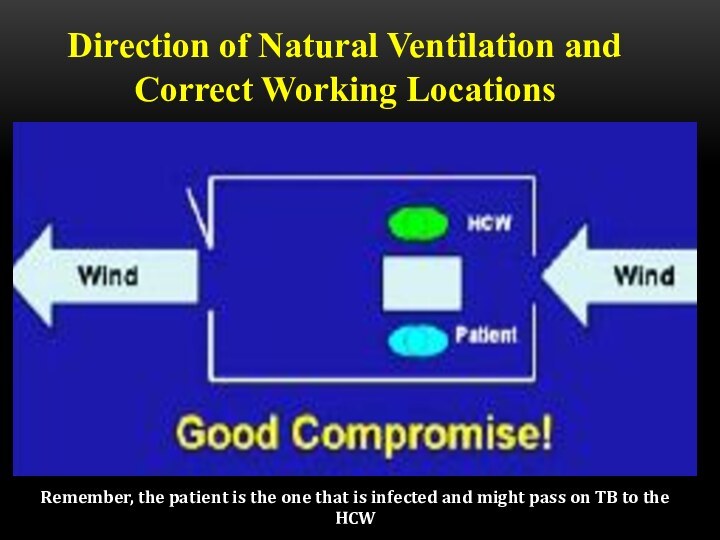
- 50. Direction of Natural Ventilation and Correct Working
- 51. Direction of Natural Ventilation and Correct Working Locations
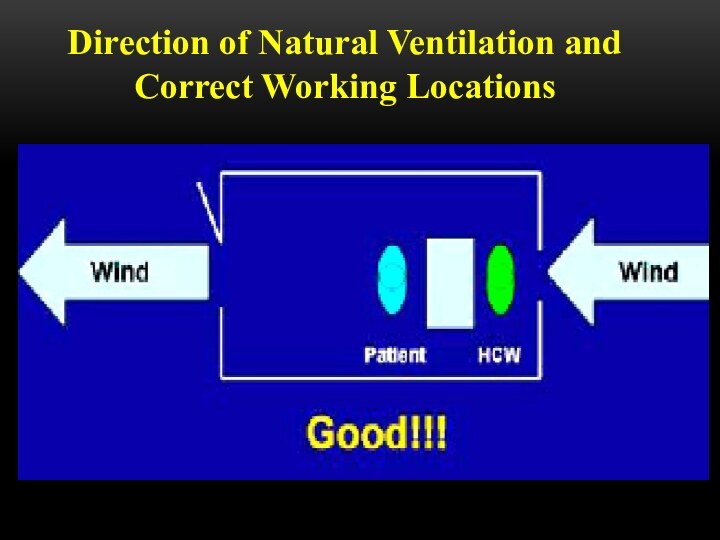
- 52. Direction of Natural Ventilation and Correct Working Locations
- 53. Direction of Natural Ventilation and Correct Working
- 55. ENVIRONMENTAL CONTROLSUltraviolet Light HEPA (high efficiency particulate air)
- 56. PERSONAL RESPIRATORY PROTECTIONRespirators:Can protect HCWsShould be encouraged
- 57. N95 RESPIRATOR DOS AND DON’TS
- 58. Be sure your respirator is properly fitted! It should fit snugly at nose and chin
- 59. Note poor fit at the bridge of
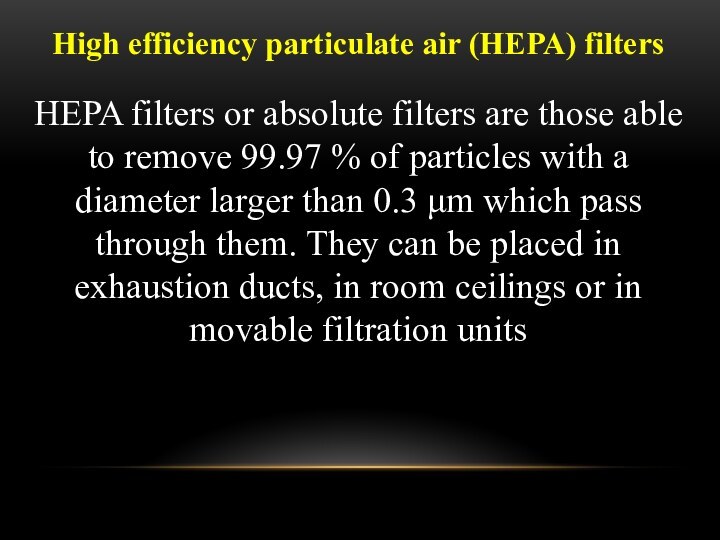
- 60. High efficiency particulate air (HEPA) filters HEPA
- 61. The use of HEPA filters and/or UV
- 62. HEPA filters are used:• To purify the
- 63. DON’T FORGET TO WEAR IT! Remember, respirators
- 64. Скачать презентацию
- 65. Похожие презентации





















Слайд 3
Social prophylaxis
Principles of prophylactic orientation, state character, toll-free
medi-care are fixed in basis of social prophylaxis.
It
is carried out due to the measures of socio-economic character of state scale.
Слайд 4
A social prophylaxis is directed on:
making healthy of
environment;
it is an increase of financial welfare of
population; it is strengthening of health of population;
it is an improvement of feed and vitally domestic terms;
it is development of physical education and sport;
are measures on a fight against alcoholism, drug addiction, smoking, other harmful habits.
Слайд 5
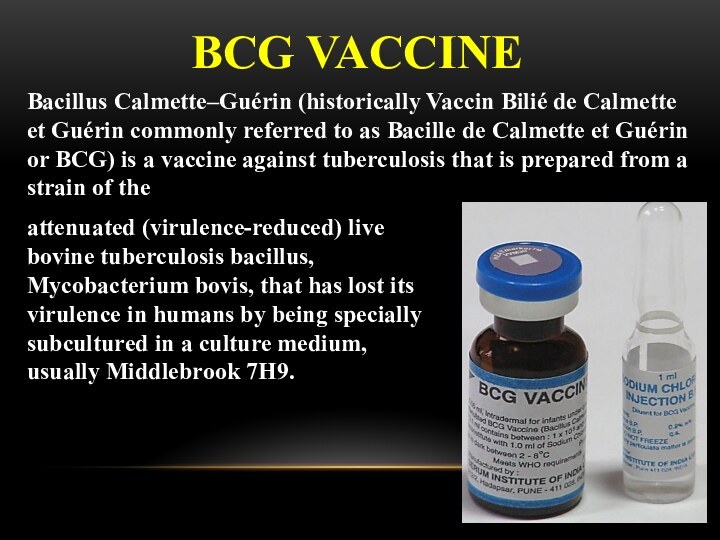
BCG VACCINE
attenuated (virulence-reduced) live bovine tuberculosis bacillus, Mycobacterium
bovis, that has lost its virulence in humans by
being specially subcultured in a culture medium, usually Middlebrook 7H9.Bacillus Calmette–Guérin (historically Vaccin Bilié de Calmette et Guérin commonly referred to as Bacille de Calmette et Guérin or BCG) is a vaccine against tuberculosis that is prepared from a strain of the
Слайд 6 Because the living bacilli evolve to make the
best use of available nutrients, they become less well-adapted
to human blood and can no longer induce disease when introduced into a human host. Still, they are similar enough to their wild ancestors to provide some degree of immunity against human tuberculosis.The BCG vaccine can be anywhere from 0 to 80% effective in preventing tuberculosis for a duration of 15 years.
Слайд 8 The bacille Calmette-Guérin (BCG) vaccine has existed for
80 years and is one of the most widely
used of all current vaccines, reading >80%of neonates and infants in countries where it is part of the national childhood immunization programme. BCG vaccine has a documented protective effect against meningitis and disseminated TB in children. It does not prevent primary infection and, more importantly, does not prevent reactivation of latent pulmonary infection, the principal source of bacillary spread in the community. The impact of BCG vaccination on transmission of MTB is therefore limited.Слайд 9 The biological interaction between MTB and the human
host is complex and only partially understood. Recent advances
in areas such as mycobacterial immunology and genomics have stimulated research on numerous new experimental vaccines, but it is unlikely that any of these urgently need vaccines will be available for routine use within the next few years. In the meantime, optimal utilization of BCG is encouraged.Слайд 11 is used for active specific prophylaxis of tuberculosis
– dry for intracutaneoud transfusion.
These are live mycobacteria of vaccine strain, lyophilicly dried in 1,5 % solution of sodium glutaminate. It looks like a white dried mass. It is manufactured in ampullas of 1 mg of vaccine, which contains 20 doses, each of 0,05 mg of the preparation. BCG vaccine is used intracutaneously in a dose of 0,05 mg in the volume of 0,1 ml.
The primary vaccination is done to healthy, delivered at the right time newly borns on the 3-5th day of their life.
Tuberculosis vaccine (BCG)
Слайд 12
BCG-M vaccine
is manufactured in a half
dose (0,5 mg in an ampulla, which contains 20
doses, each of 0.025 mg of the preparation)is meant for vaccinating prematurely newly borns and children who were not immunised at birth in connection with contraindications, as well as for vaccination and revaccination of children, who live in the territories (areas) contaminated with radionuclides (III-IV zone).
Слайд 13
BCG-STRAINS
There have been many (WHO estimated 40 or
more in 1999) manufacturers of BCG around the world.
The most widely-used strains in international immunization programmes include: “Danish 1331” strain; “Moscow” strain, and “Tokyo 172” strain. The use of other strains is largely limited to their country of origin, e.g. “Moreau” strain (Brazil) or “Tice” strain (USA).Слайд 14 when the vaccine had been administered in infancy,
as is recommended by WHO and widely practiced, use
of presence or absence of BCG scar years later was not a highly sensitive and reliable indicator of prior vaccination status. There is also no evidence of a correlation between increased BCG scar size and protection against either tuberculosis.
Слайд 15
VACCINATION PROCEDURE
BCG is given as a single intradermal
injection at the insertion of the deltoid
Слайд 16
THE RULES OF TRANSFUSION
The dry vaccine (1 ampulla ) is dissolved in
2 ml of isotonic solution and the cultivation is the result, i.e. 1 dose in 0,1 ml of the solution.The vaccine is used during 2-3 hours, the remnant is destroyed by boiling.
0,2 ml of the dissolved vaccine is taken into 1-gram syringe after mixing, the air and part of the preparation up to 0,1 ml mark is evacuated through the needle.
The vaccine is injected strictly intracutaneously on the limit between the upper and the middle third part of the shoulder, having previously rubbed the skin with 70° spirit.
At the proper technique a whitish papule of 5-6 mm in diameter is formed, which resolves in 15-20 minutes.
Слайд 20
BCG IN ADOLESCENTS AND ADULTS
There is no evidence
that revaccination with BCG affords any additional protection, and
general revaccination is therefore not recommended.However, given the serious consequences of developing multidrug-resistant disease and the low reactogenicity of the vaccine, BCG vaccination may be considered for all HIV-negative, unvaccinated, tuberculin-negative persons who are in an unavoidable close exposure to multidrug-resistant tuberculosis (MTB) (e.g. health care workers in facilities still lacking of proper TB infection control measures in place).
Слайд 21
BCG IN HIV-INFECTED NEWBORNS
In children who are known
to be HIV-infected, BCG vaccine should not be given.
In infants whose HIV status is unknown and who are born to HIV-positive mothers and who lack symptoms suggestive of HIV, BCG vaccine should be given after considering local factors. Such factors are likely to be important determinants of the risk-benefit balance of such an approach and include: coverage and success of the prevention of mother to child transmission of HIV programme; possibility of deferring BCG vaccination in HIV-exposed infants until HIV infection status has been established; availability of early diagnosis of HIV infection in infants; and, provision of early ART to HIV-positive infants.
Слайд 22
COMPLICATIONS (BCG-RELATED DISEASES) CLASSIFICATION (WHO, 1984)
Local (the
most frequent) – cold abscess, ulcer, regional lymphadenitis.
Disseminated BCG-infection
(osteitis, lupus). Generalized BCG-infection with lethal outcomes.
Post-BCG syndrome (cheloid cicatrix, nodular erythema, allergic rash).
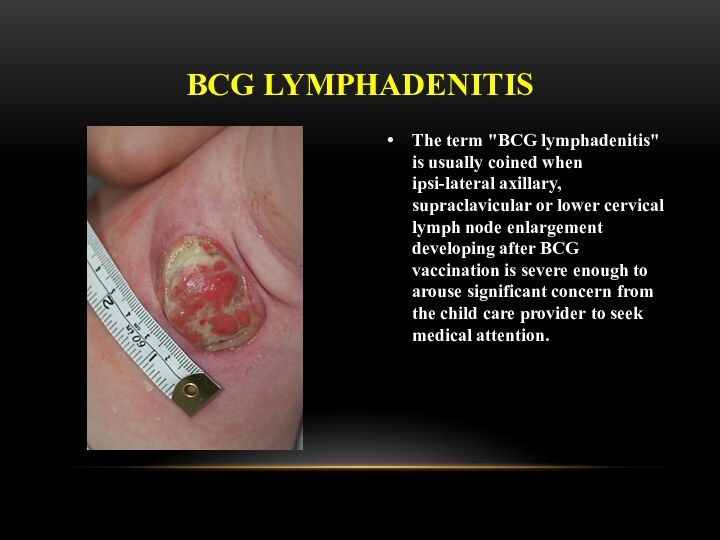
Слайд 23 The term "BCG lymphadenitis" is usually coined when
ipsi-lateral axillary, supraclavicular or lower cervical lymph node enlargement
developing after BCG vaccination is severe enough to arouse significant concern from the child care provider to seek medical attention.BCG LYMPHADENITIS
Слайд 24
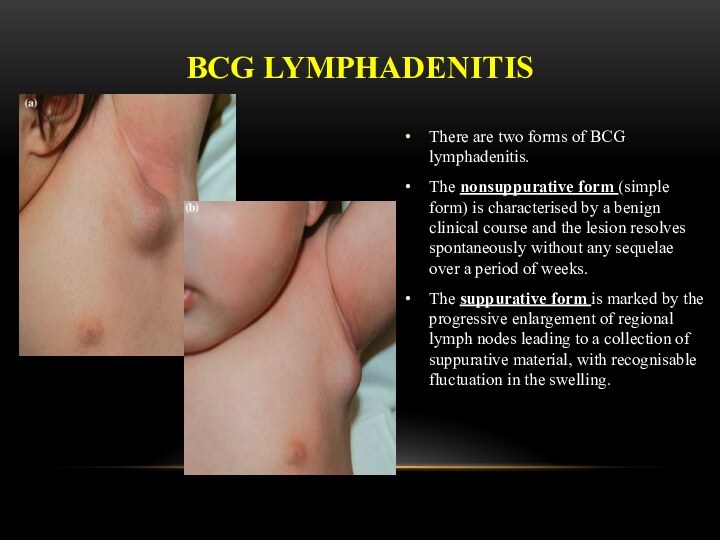
There are two forms of BCG lymphadenitis.
The nonsuppurative
form (simple form) is characterised by a benign clinical
course and the lesion resolves spontaneously without any sequelae over a period of weeks.The suppurative form is marked by the progressive enlargement of regional lymph nodes leading to a collection of suppurative material, with recognisable fluctuation in the swelling.
BCG LYMPHADENITIS
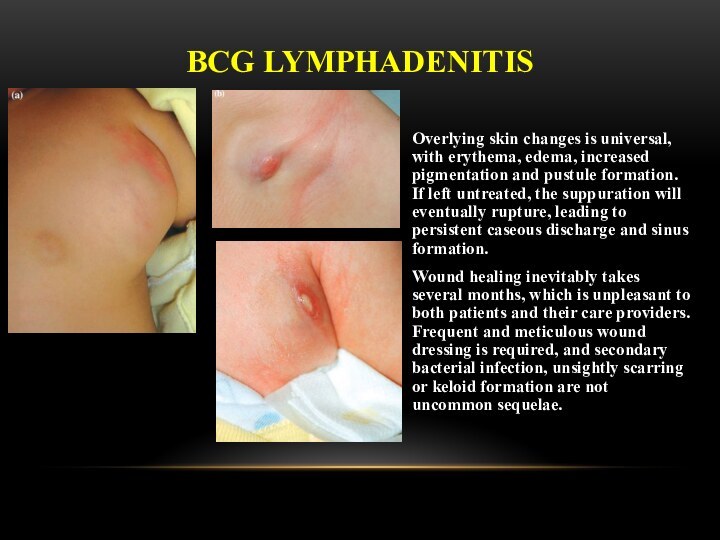
Слайд 25 Overlying skin changes is universal, with erythema, edema,
increased pigmentation and pustule formation. If left untreated, the
suppuration will eventually rupture, leading to persistent caseous discharge and sinus formation.Wound healing inevitably takes several months, which is unpleasant to both patients and their care providers. Frequent and meticulous wound dressing is required, and secondary bacterial infection, unsightly scarring or keloid formation are not uncommon sequelae.
BCG LYMPHADENITIS
Слайд 26
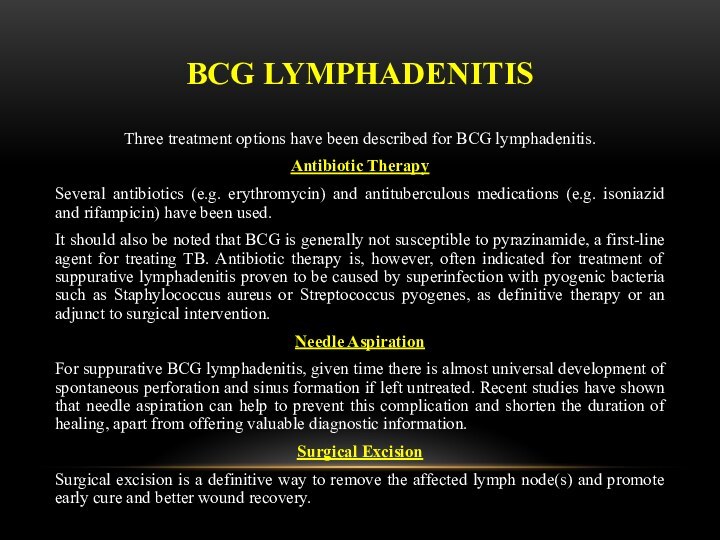
BCG LYMPHADENITIS
Three treatment options have been described for
BCG lymphadenitis.
Antibiotic Therapy
Several antibiotics (e.g. erythromycin) and antituberculous medications
(e.g. isoniazid and rifampicin) have been used.It should also be noted that BCG is generally not susceptible to pyrazinamide, a first-line agent for treating TB. Antibiotic therapy is, however, often indicated for treatment of suppurative lymphadenitis proven to be caused by superinfection with pyogenic bacteria such as Staphylococcus aureus or Streptococcus pyogenes, as definitive therapy or an adjunct to surgical intervention.
Needle Aspiration
For suppurative BCG lymphadenitis, given time there is almost universal development of spontaneous perforation and sinus formation if left untreated. Recent studies have shown that needle aspiration can help to prevent this complication and shorten the duration of healing, apart from offering valuable diagnostic information.
Surgical Excision
Surgical excision is a definitive way to remove the affected lymph node(s) and promote early cure and better wound recovery.
Слайд 29 Osteitis after BCG vaccination is a rare condition,
with an incidence of approximately 0.39/1,000,000, depending on the
bacillus used.Bone involvement occurs due to lymphohematogenous dissemination, and the lesion site is not necessarily associated with the injection site. The sites most often affected are the tibia, femur, vertebrae, sternum and ribs.
DISSEMINATED BCG-INFECTION
Слайд 30 Clinical manifestations usually occur 18 months after
vaccination, this interval can range from a few months
to 5 years.The initial symptoms are sensitivity, pain and limited movement of the affected region. When present, fever is low and does not affect the general status of the individual.
On X-rays, lytic lesions with a sclerotic halo can be seen, as can periosteal reaction and periarticular osteoporosis.
Histopathological studies show granulomatous inflammation with epithelioid cells, with or without caseous necrosis. Acid-fast bacilli are detected in approximately half of all cases, and most present strongly positive PPD reactions.
It recommends treatment with isoniazid and rifampin for 12 months.
In most cases, long-term antituberculosis therapy and surgical drainage are necessary for remission. Fortunately, the prognosis is good, with a low frequency of complications. Therefore, the use of BCG vaccine should be maintained in countries with a high incidence of TB.
DISSEMINATED BCG-INFECTION
Слайд 31
GENERALIZED BCG-INFECTION
Generalized infection due to BCG vaccination has
also been reported, sometimes being fatal. Systemic BCG-itis is
a recognized but rare consequence of BCG vaccination, and traditionally has been seen in children with severe immune deficiencies. A recent multi-centre study has identified the syndrome in children with severe combined immunodeficiency (SCID), chronic granulomatous disease, Di George syndrome and homozygous complete or partial interferon gamma receptor deficiency (Jouanguy, 1996; Jouanguy 1997; Casanova, 1995). Its frequency is reported as less than 5 per million vaccine recipients, reflecting the rarity of the underlying conditions (Lotte, 1988). If not properly managed, these cases may be fatal.According to Mande, 1980, the first case was reported in 1953, 30 years after BCG had first been applied to man. Between 1954 and 1980, 34 cases were published in the global literature, and the Lotte et al. study estimates the incidence as 2.19 per one million vaccine recipients. Nevertheless, three recent Canadian cases were reported in 1998. Severe and generalized BCG infection that may occur in immunocompromised individuals should be treated with anti-tuberculous drugs including isoniazid and rifampicin (Romanus et al., 1993).
Слайд 32
LATENT TB INFECTION
Latent tuberculosis infection (LTBI) is defined
as a state of persistent immune response to stimulation
by Mycobacterium tuberculosis antigens without evidence of clinically manifested active TB .One third of the world’s population is estimated to be infected with M. tuberculosis. The vast majority of infected persons have no signs or symptoms of TB disease and are not infectious, but they are at risk for developing active TB disease and becoming infectious. The lifetime risk of reactivation TB for a person with documented LTBI is estimated to be 5–10 %, with the majority developing TB disease within the first five years after initial infection.
However, the risk of developing TB disease following infection depends on several factors, the most important one being the immunological status of the host.
Слайд 33
PREVENTIVE CHEMOTHERAPY
Guidelines on the management of latent tuberculosis
infection were developed in accordance to the requirements and
recommended process of the WHO Guideline Review Committee, and provide public health approach guidance on evidence-based practices for testing, treating and managing LTBI in infected individuals with the highest likelihood of progression to active Disease.The guidelines are also intended to provide the basis and rationale for the development of national guidelines. The guidelines are primarily targeted at high-income or upper middle-income countries with an estimated TB incidence rate of less than 100 per 100 000 population.
Resource-limited and other middle-income countries that do not belong to the above category should implement the existing WHO guidelines on people living with HIV and child contacts below 5 years of age.
Слайд 34
PREVENTIVE CHEMOTHERAPY
Systematic testing and treatment of LTBI should
be performed in people living with HIV, adult and
child contacts of pulmonary TB cases, patients initiating anti-tumour necrosis factor (TNF) treatment, patients receiving dialysis, patients preparing for organ or haematologic transplantation, and patients with silicosis. Either interferon-gamma release assays (IGRA) or Mantoux tuberculin skin test (TST) should be used to test for LTBI.(Strong recommendation, low to very low quality of evidence)
Слайд 35
PREVENTIVE CHEMOTHERAPY
Systematic testing and treatment of LTBI should
be considered for prisoners, health-care workers, immigrants from high
TB burden countries, homeless persons and illicit drug users. Either IGRA or TST should be used to test for LTBI.(Conditional recommendation, low to very low quality of evidence)
Слайд 36
PREVENTIVE CHEMOTHERAPY
Systematic testing for LTBI is not recommended
in people with diabetes, people with harmful alcohol use,
tobacco smokers, and underweight people provided they are not already included in the above recommendations.(Conditional recommendation, very low quality of evidence)
Слайд 37
PREVENTIVE CHEMOTHERAPY
Individuals should be asked about symptoms of
TB before being tested for LTBI. Chest radiography can
be done if efforts are intended also for active TB case finding. Individuals with TB symptoms or any radiological abnormality should be investigated further for active TB and other conditions.(Strong recommendation, low quality of evidence)
Слайд 38
PREVENTIVE CHEMOTHERAPY
Either TST or IGRA can be used
to test for LTBI in high-income and upper middle-income
countries with estimated TB incidence less than 100 per 100 000(Strong recommendation, low quality of evidence).
IGRA should not replace TST in low-income and other middle-income countries.
(Strong recommendation, very low quality of evidence)
Слайд 39 FOR RESOURCE-LIMITED COUNTRIES AND OTHER MIDDLE-INCOME COUNTRIES THAT
DO NOT BELONG TO THE ABOVE CATEGORY
People living with
HIV and children below 5 years of age who are household or close contacts of people with TB and who, after an appropriate clinical evaluation, are found not to have active TB but have LTBI should be treated. (Strong recommendation, high quality of evidence)
Слайд 40
PREVENTIVE CHEMOTHERAPY
Treatment options recommended for LTBI include:
6-month
isoniazid, or
9-month isoniazid,
or 3-month regimen of weekly
rifapentine plus isoniazid, or 3–4 months isoniazid plus rifampicin, or 3–4 months rifampicin alone.
(Strong recommendation, moderate to high quality of evidence).
Слайд 41
MDR-TB CASES
Strict clinical observation and close monitoring for
the development of active TB disease among contacts of
multidrug-resistant TB (MDR-TB) cases preferably for at least two years over the provision of preventive treatment.Clinicians can consider individually tailored treatment regimens based on the drug susceptibility profile of the index case, particularly for child contacts below 5 years of age, when benefits can outweigh harms with reasonable confidence.
Слайд 42
RISK OF DRUG RESISTANCE FOLLOWING LTBI TREATMENT
A systematic
review was conducted to determine whether LTBI treatment leads
to significant development of resistance. The systematic review considered the following treatment regimens:Isoniazid for 6- to 12-month duration: Thirteen studies comparing 6- to 12-month isoniazid preventive therapy versus no treatment or placebo were included in the systematic review (seven involving HIV uninfected populations); no difference in the risk of resistance among incident TB cases was found (risk ratio = 1.45 (95% CI: 0.85–2.47)). There was little evidence of heterogeneity (p=0.923) and the risk ratio for HIV-uninfected and HIV-infected populations was comparable. The quality of the evidence was moderate.
Isoniazid for 36 months in HIV-infected individuals:Three studies comparing 36- and 6-month isoniazid were reviewed but only one study provided resistance rates, and no significant Difference in drug resistance was found (risk ratio = 5.96 (95% CI: 0.24–146) (24). The two other studies reported that the observed proportion of resistant cases were similar to the expected rate in the background population, but did not provide a direct comparison of resistance rates between those receiving 36 months compared to those receiving 6 months treatment (25,26). Therefore, it was concluded that there is no evidence to indicate whether or not continuous use of isoniazid increases the risk of isoniazid resistance.
Слайд 44 EMPHASISE THAT TRANSMISSION IS NOT ONE-WAY AND DOES
NOT DISCRIMINATE! PATIENTS CAN TRANSMIT TO WORKERS, VISITORS AND OTHER
PATIENTS AND VICE VERSA. ANY INFECTIOUS PERSON PUTS EVERYONE IN HIS/HER IMMEDIATE SURROUNDINGS AT RISK! INFECTION PREVENTION AND CONTROL IS THE PREVENTION OF TRANSMISSION FROM INDIVIDUAL TO INDIVIDUAL (AS ABOVE) THROUGH ADMINISTRATIVE, ENVIRONMENTAL, AND PERSONAL PROTECTION EQUIPMENTPatient to:
Worker
Visitor
Patient
Worker to:
Worker
Visitor
Patient
Visitor to:
Worker
Visitor
Patient
Слайд 45
HIERARCHY OF
INFECTION PREVENTION & CONTROL
Administrative controls
Reduce risk
of exposure, infection and disease thru policy and practice
Environmental
(engineering) controlsReduce concentration of infectious bacilli in air in areas where air contamination is likely
Personal respiratory protection
Protect personnel who must work in environments with contaminated air
Слайд 46
ADMINISTRATIVE CONTROLS
Develop and implement written policies and protocols
to ensure:
Rapid identification of TB cases (e.g., improving the
turn-around time for obtaining sputum results)Isolation of patients with PTB
Rapid diagnostic evaluation
Rapid initiation treatment
Educate, train, and counsel HCWs about TB
To the extent possible, avoid mixing TB patients and HIV patients in the hospital or clinic setting
Слайд 47
ENVIRONMENTAL CONTROLS:
VENTILATION AND AIR FLOW
Ventilation is the
movement of air
Should be done in a controlled manner
Types
Natural
Local
General
Simple
measures can be effective
Слайд 48
EVIDENCE FROM PERU
Open windows and doors produced 6x
greater air exchanges than mechanical ventilation and 20x great
air changes per hour than with windows closedNatural ventilation in “old-style” hospitals and clinics resulted in much better ventilation and much lower calculated TB risk, despite similar patient crowding
More likely to have larger, higher ceilings; larger windows; windows on opposite walls allowing through-flow of air
Слайд 49
ESTIMATED RISK OF
AIRBORNE TB INFECTION
Naturally ventilated, windows
closed - 97%
Mechanically ventilated with neg pressure (ACH 12)
- 39%Naturally ventilation, windows and doors fully open:
Modern (1970-1990) - 33%
Old-fashioned (pre-1950) - 11%
Слайд 50 Direction of Natural Ventilation and Correct Working Locations
When increasing ventilation and air flow, care should be
taken as to the appropriate positioning of the windows, doors, the patient and the HCW to control infection
Слайд 53
Direction of Natural Ventilation and Correct Working Locations
Remember,
the patient is the one that is infected and
might pass on TB to the HCW
Слайд 55
ENVIRONMENTAL CONTROLS
Ultraviolet Light
HEPA (high efficiency particulate air) filters
Both
indirect ultraviolet irradiation of air and HEPA filters have
been used in some high-risk settings to reduce the concentration of infectious TB particles in the ambient air
Слайд 56
PERSONAL RESPIRATORY PROTECTION
Respirators:
Can protect HCWs
Should be encouraged in
high-risk settings
May be unavailable in low-resource settings
Face/surgical masks:
Act as
a barrier to prevent infectious patients from expelling dropletsDo not protect against inhalation of microscopic TB particles
Слайд 59
Note poor fit at the bridge of nose
Note
poor fit at the chin
Respirator should cover chin and
create a seal
Слайд 60
High efficiency particulate air (HEPA) filters
HEPA filters
or absolute filters are those able to remove 99.97
% of particles with a diameter larger than 0.3 μm which pass through them. They can be placed in exhaustion ducts, in room ceilings or in movable filtration unitsСлайд 61 The use of HEPA filters and/or UV light
is strongly recommended for rooms where the following procedures
take place:bronchoscopy,
induced sputum,
pentamidine nebulization,
necropsy,
isolation.
The combination of an adequate number of air changes with negative pressure and a HEPA filter or UV light minimizes the risk of transmission in the environment in which the TB patient is assisted and in the area where the air is exhausted. The germicidal efficiency of the UV light is limited to its area of direct incidence and decreases with time
Слайд 62
HEPA filters are used:
• To purify the exhaustion
of air of contaminated environments
• To recirculate the air
inside the room or to other rooms facilitating thenumber of air changes per hour.