- Главная
- Разное
- Бизнес и предпринимательство
- Образование
- Развлечения
- Государство
- Спорт
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Религиоведение
- Черчение
- Физкультура
- ИЗО
- Психология
- Социология
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Геометрия
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Что такое findslide.org?
FindSlide.org - это сайт презентаций, докладов, шаблонов в формате PowerPoint.
Обратная связь
Email: Нажмите что бы посмотреть
Презентация на тему Chest pain
Содержание
- 2. CHEST PAIN5% of all ED visits per yearDifferential diagnosis is difficult
- 3. CHEST PAINANATOMYDIFFERENTIAL DIAGNOSISBRIEF OVERVIEW OF DISEASE PROCESSES CAUSING CHEST PAINAPPROACH TO CHEST PAIN
- 4. ANATOMYIn devising a differential diagnosis for chest
- 5. ANATOMY SKIN
- 6. ANATOMY BONES
- 7. ANATOMYPULMONARY SYSTEM
- 8. ANATOMY HEART
- 9. ANATOMY VASCULAR AND GI SYSTEMAORTA AND ESOPHAGUS
- 10. DIFFERENTIAL DIAGNOSIS OF CHEST PAINCHEST WALL PAINPULMONARY CAUSESCARDIAC CAUSESVASCULAR CAUSESGI CAUSESOTHER (PSYCHOGENIC CAUSES)
- 11. DD: CHEST PAINCHEST WALL PAIN
- 12. DD: CHEST PAINPULMONARY CAUSES1 - Pulmonary Embolism
- 13. DD: CHEST PAINCARDIAC CAUSES -
- 14. DD: CHEST PAINVascular Causes: -Aortic Dissection
- 15. DD: CHEST PAINGI CAUSES -ESOPHAGEAL
- 16. DD: CHEST PAINPSYCHIATRIC - PANIC DISORDER
- 17. CHEST PAINBRIEF OVERVIEW OF DISEASE PROCESSES CAUSING CHEST PAIN
- 18. CHEST WALL PAIN .
- 19. CHEST WALL PAINHERPES ZOSTER -Reactivation of
- 20. HERPES ZOSTERClusters of vesicles (with clear or
- 21. HERPES ZOSTERTREATMENT: * Antivirals: reduce duration
- 22. CHEST WALL PAINMusculoskeletal Pain - Usually localized,
- 23. MUSCULOSKELETAL PAINDIAGNOSISCOSTOCHONDRITISTIETZE SYNDROMEXIPHODYNIAPRECORDIAL CATCH SYNDROMERIB FRACTURECLINICAL FEATURESInflammation
- 24. MUSCULOSKELETAL PAINTreatment: Analgesia (NSAIDs)
- 25. PULMONARY CAUSES OF CHEST PAIN.
- 26. PULMONARY EMBOLISMRISK FACTORS: VIRCHOW’S TRIAD -
- 27. PULMONARY EMBOLISM (PE)CLINICAL FEATURES - Shortness
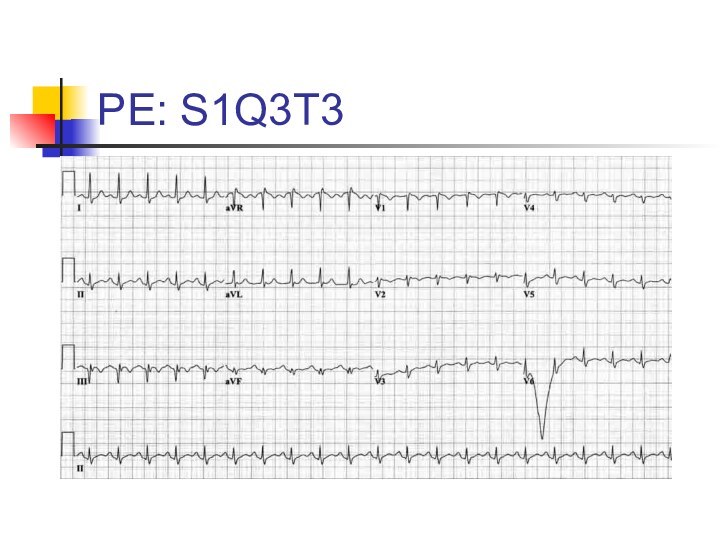
- 28. PE: DIAGNOSTIC TESTSECG: -Sinus tachycardia
- 29. PE: S1Q3T3
- 30. PE: DIAGNOSTIC TESTSCHEST X-RAY - Normal
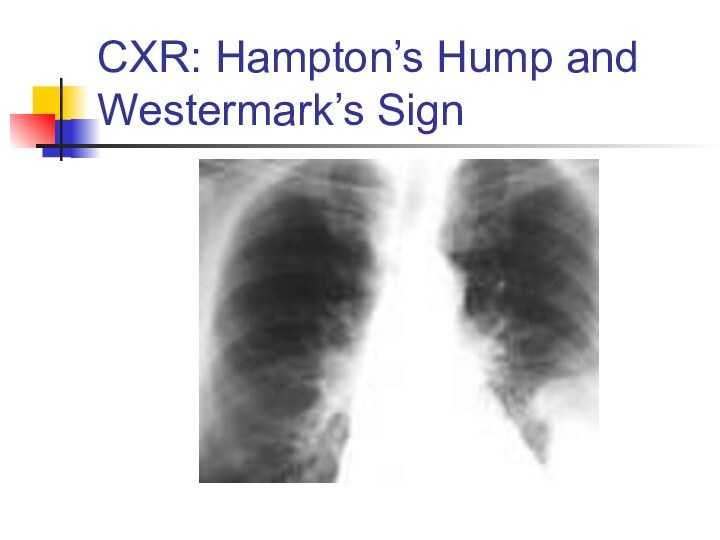
- 31. CXR: Hampton’s Hump and Westermark’s Sign
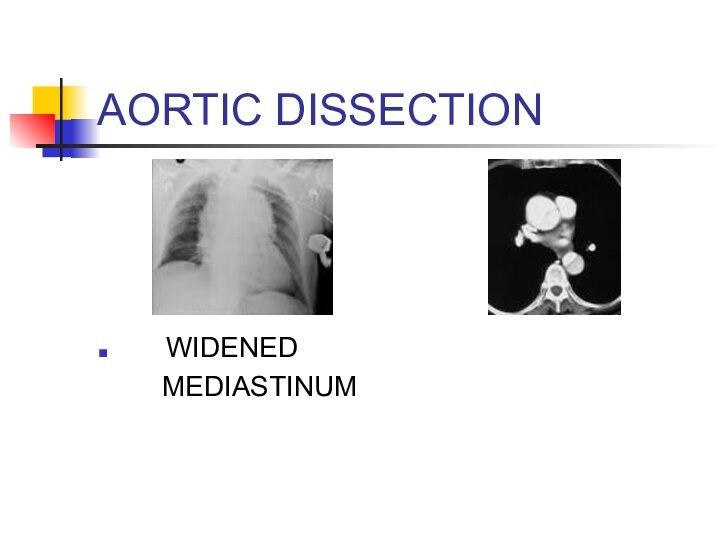
- 32. PE: DIAGNOSTIC TESTSABG: *Look
- 34. PE: DIAGNOSTIC TESTSVQ SCAN (Ventilation-Perfusion scan)- use
- 35. PE: TREATMENTInitiate Heparin * Unfractionated Heparin:
- 36. PNEUMONIACLINICAL FEATURES - Cough +/- sputum
- 37. PNEUMONIA: DIAGNOSISX-RayIf patient is to be hospitalized:Consider
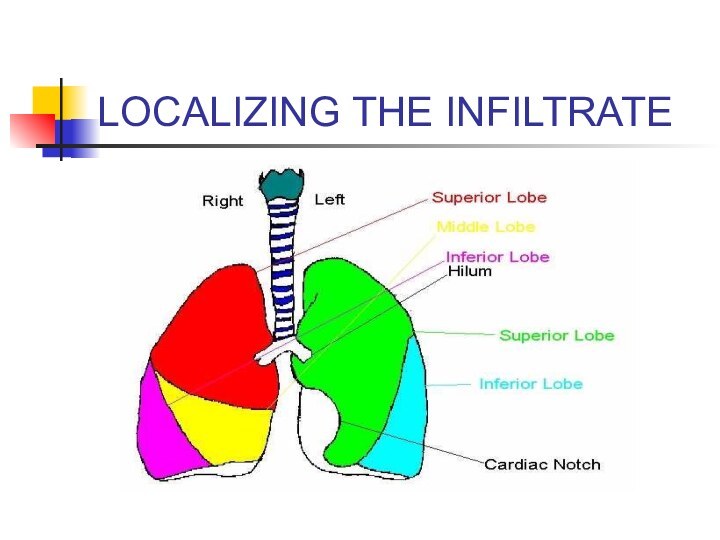
- 38. LOCALIZING THE INFILTRATE
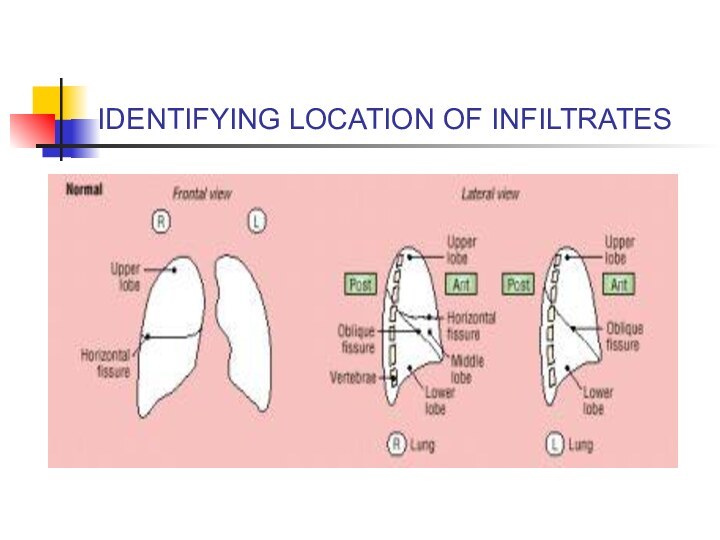
- 39. IDENTIFYING LOCATION OF INFILTRATES
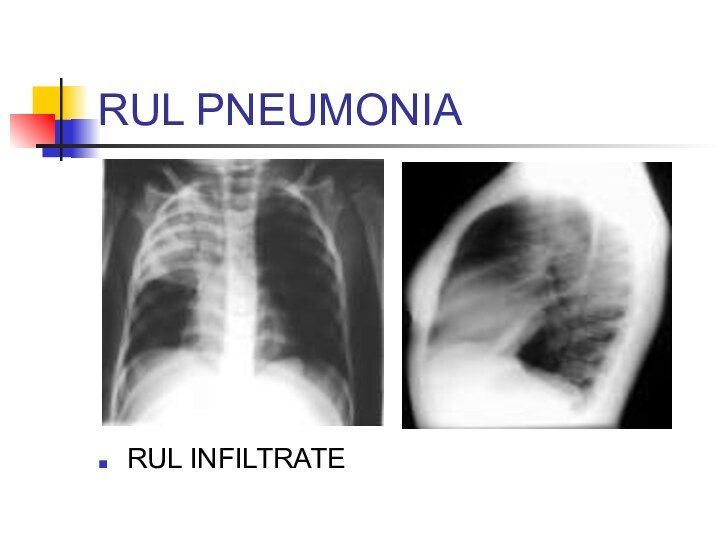
- 40. RUL PNEUMONIARUL INFILTRATE
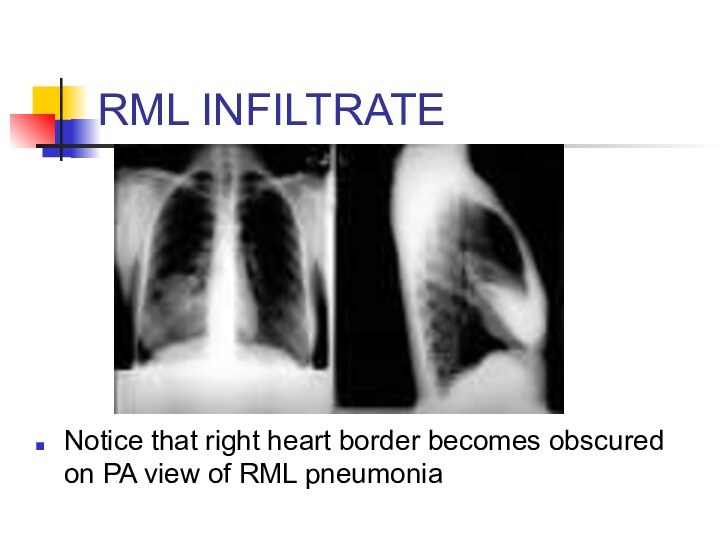
- 41. RML INFILTRATENotice that right heart border becomes obscured on PA view of RML pneumonia
- 42. RLL PNEUMONIARLL infiltrate
- 43. PNEUMONIA: TREATMENTCommunity- Acquired: - OUT-PATIENT
- 44. SPONTANEOUS PNEUMOTHORAXRISK FACTORS: - Primary
- 45. PNEUMOTHORAXCLINICAL FEATURES - Acute pleuritic chest
- 46. TENSION PNEUMOTHORAXWhat is wrong with this picture??
- 47. TENSION PNEUMOTHORAXAnswer: Chest X-ray should have never
- 48. Tension PneumothoraxTrachea deviates to contralateral sideMediastinum shifts
- 49. NEEDLE DECOMPRESSIONInsert large bore needle (14 or
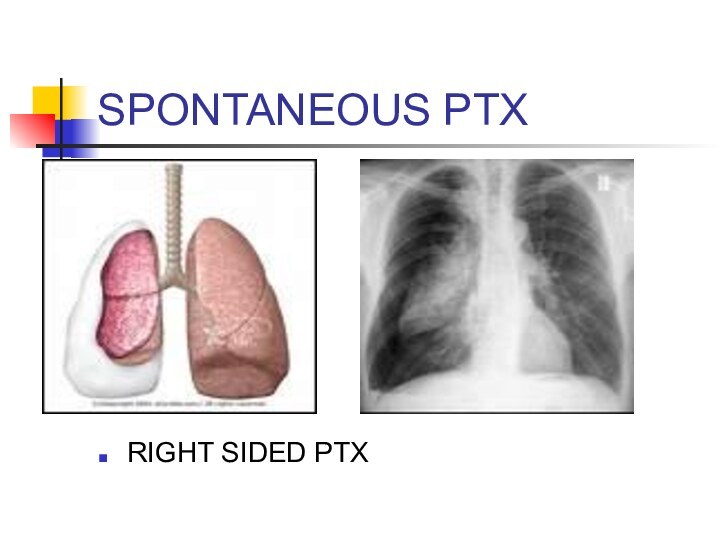
- 50. SPONTANEOUS PTXRIGHT SIDED PTX
- 51. SPONTANEOUS PTXTREATMENT: - If small (
- 52. PLEURITIS/SEROSITISInflammation of pleura that covers lungPleuritic chest
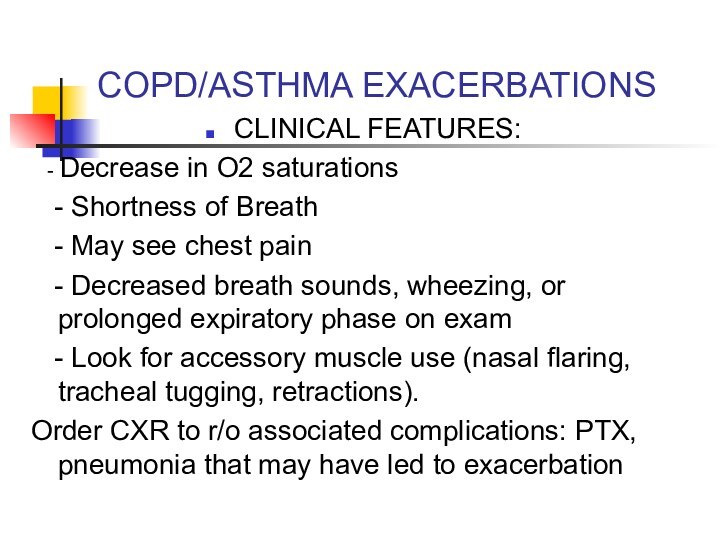
- 53. COPD/ASTHMA EXACERBATIONSCLINICAL FEATURES: - Decrease in
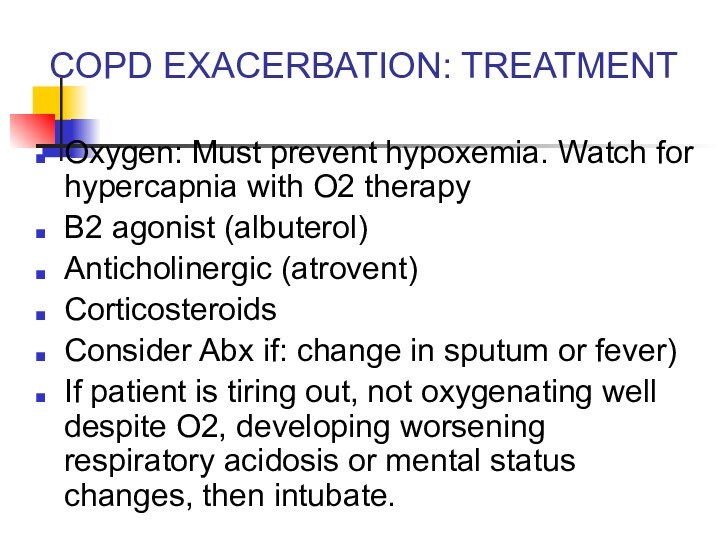
- 54. COPD EXACERBATION: TREATMENTOxygen: Must prevent hypoxemia. Watch
- 55. ASTHMA TREATMENTOxygenInhaled short acting B2 agonists: AlbuterolAnticholinergics:
- 56. CARDIAC CAUSES OF CHEST PAIN.
- 57. RISK FACTORS FOR CADAgeDiabetesHypertensionFamily HistoryTobacco UseHypercholesterolemiaCocaine use
- 58. ISCHEMIC CHEST PAINEXERTIONAL ANGINA * BRIEF
- 59. Angina pectorisStable angina pectoris is a clinical
- 60. Angina pectorisThe chest discomfort may be described
- 61. The chest discomfort usually lasts up to
- 62. ISCHEMIC CHEST PAIN: DIAGNOSIS12 LEAD EСG
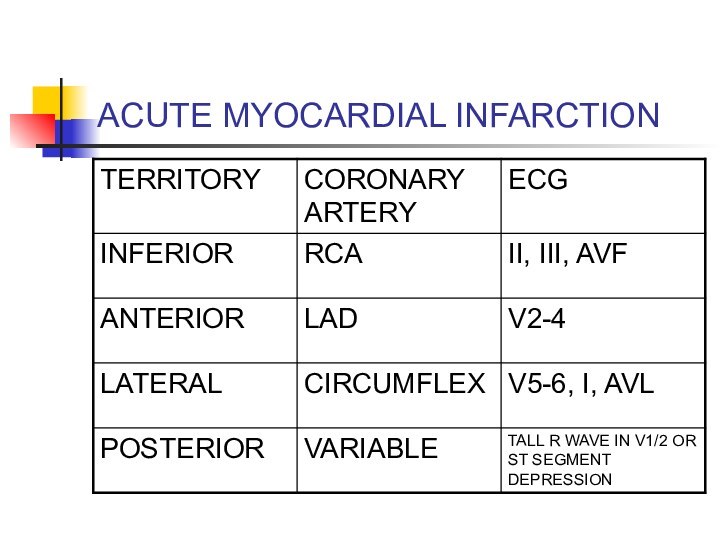
- 63. ACUTE MYOCARDIAL INFARCTION
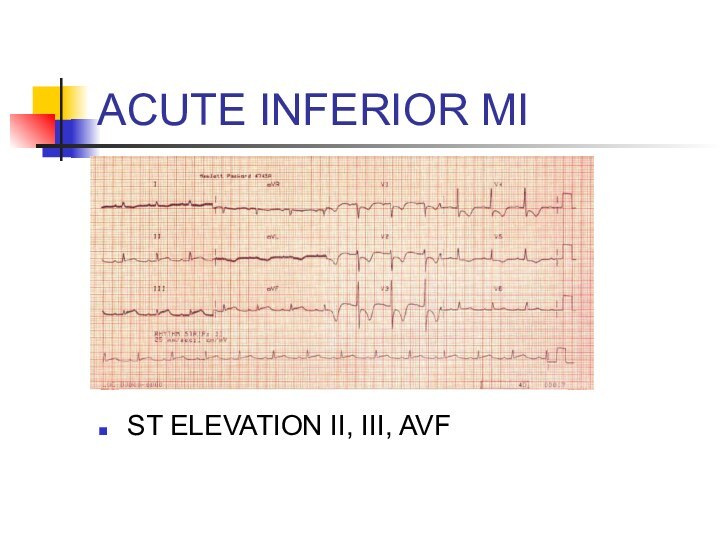
- 64. ACUTE INFERIOR MIST ELEVATION II, III, AVF
- 65. ACUTE ANTERIOR MIST SEGMENT ELEVATION V2-4
- 66. EСG CHANGES IN ISCHEMIC HEART DISEASE
- 67. EСG CHANGES IN ISCHEMIC HEART DISEASE
- 68. ISCHEMIC CHEST PAIN: DIAGNOSTIC TESTSCARDIAC ENZYMES
- 69. ISCHEMIC HEART DISEASE TREATMENT: ACUTE ST SEGMENT
- 70. ISCHEMIC HEART DISEASE TREATMENT: NONSTEMI AND UNSTABLE
- 71. LOW RISK CARDIAC CHEST PAINIf low risk
- 72. VALVULAR HEART DISEASEAORTIC STENOSIS *Classic triad:
- 73. ACUTE PERICARDITISCLINICAL FEATURES - Acute, stabbing chest
- 74. ACUTE PERICARDITISCOMMON CAUSES * IDIOPATHIC
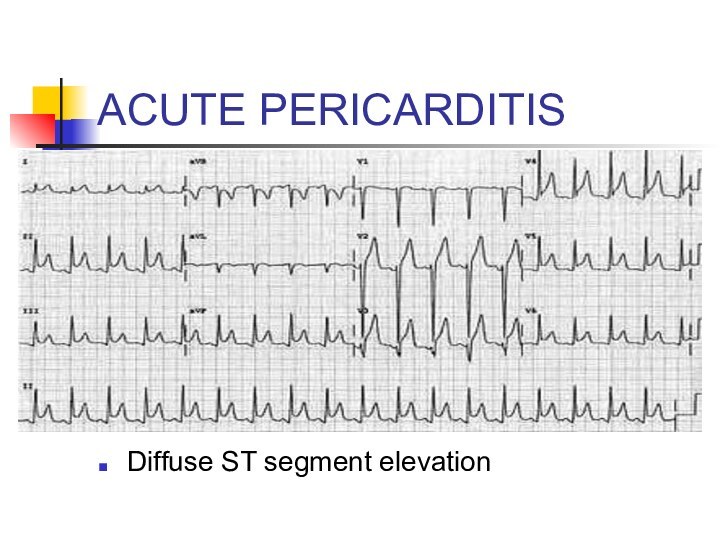
- 75. ACUTE PERICARDITIS: DIAGNOSTIC TESTSECG *Look for diffuse
- 76. ACUTE PERICARDITISDiffuse ST segment elevation
- 77. TAMPONADEELECTRICAL ALTERNANS
- 78. ACUTE PERICARDITISTREATMENT: - If idiopathic or viral: NSAIDs - Otherwise treat underlying pathology
- 79. MYOCARDITISInflammation of heart muscleFrequently accompanied by pericarditisFeverTachycardia
- 80. VASCULAR CAUSES OF CHEST PAIN.
- 81. AORTIC DISSECTIONRISK FACTORS - UNCONTROLLED HYPERTENSION
- 82. AORTIC DISSECTIONCLINICAL FEATURES * Abrupt onset of
- 83. DIAGNOSIS: AORTIC DISSECTIONCXR: Look for widened mediastinumCT
- 84. AORTIC DISSECTION WIDENED MEDIASTINUM
- 85. AORTIC DISSECTIONTREATMENT: - ANTIHYPERTENSIVE THERAPY
- 86. GI CAUSES OF CHEST PAIN.
- 87. ESOPHAGEAL CAUSESREFLUXESOPHAGITISESOPHAGEAL PERFORATIONSPASM/MOTILITY DISORDER/
- 88. GERDRISK FACTORS * High food fat
- 89. GERDCLINICAL FEATURES * Burning pain *
- 90. ESOPHAGITISCLINICAL FEATURES *Chest pain +Odynophagia (pain
- 91. ESOPHAGEAL PERFORATIONCAUSES *Iatrogenic: Endoscopy * Boerhaave
- 92. ESOPHAGEAL PERFORATIONCLINICAL FEATURES *Acute persistent chest pain
- 93. ESOPHAGEAL PERFORATIONDIAGNOSIS *x-Ray: May see pleural effusion
- 94. ESOPHAGEAL MOTILITY DISORDERSCLINICAL FEATURES: * Chest
- 95. OTHER GI CAUSES In appropriate setting, consider PUD, Biliary Disease, and Pancreatitis in differential of chest pain.
- 96. PSYCHOLOGIC CAUSESDiagnosis of exclusion
- 97. APPROACH TO THE PATIENT WITH CHEST PAINPUTTING IT ALL TOGETHER
- 98. INITIAL APPROACHLike everything else: ABCs A:
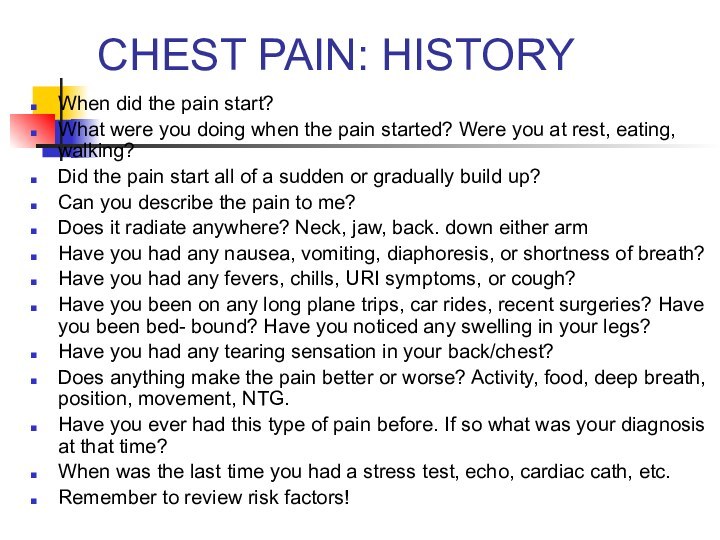
- 99. CHEST PAIN: HISTORYTime and character of onsetQualityLocationRadiationAssociated symptomsAggravating symptomsAlleviating symptomsPrior episodesSeverityReview risk factors
- 100. CHEST PAIN: HISTORYTIME AND CHARACTER OF ONSET:
- 101. CHEST PAIN: HISTORYQuality: *Pleuritic Pain: PE,
- 102. CHEST PAIN: HISTORYRADIATION: * To neck,
- 103. CHEST PAIN: HISTORYAGGRAVATING SYMPTOMS: * Activity: consider
- 104. CHEST PAIN: HISTORYALLEVIATING SYMPTOMS * Rest/ Cessation
- 105. CHEST PAIN: HISTORYRISK FACTORS * Hypertension,
- 106. CHEST PAIN: HISTORYWhen did the pain start?What
- 107. CHEST PAIN: PHYSICAL EXAMReview vital signs
- 108. CHEST PAIN: PHYSICAL EXAMCV EXAM * Assess
- 109. CHEST PAIN: ANCILLARY TESTINGLABS: Consider……. * Baseline
- 110. CHEST PAIN: ANCILLARY TESTSIMAGING: CONSIDER…… *
- 111. Скачать презентацию
- 112. Похожие презентации
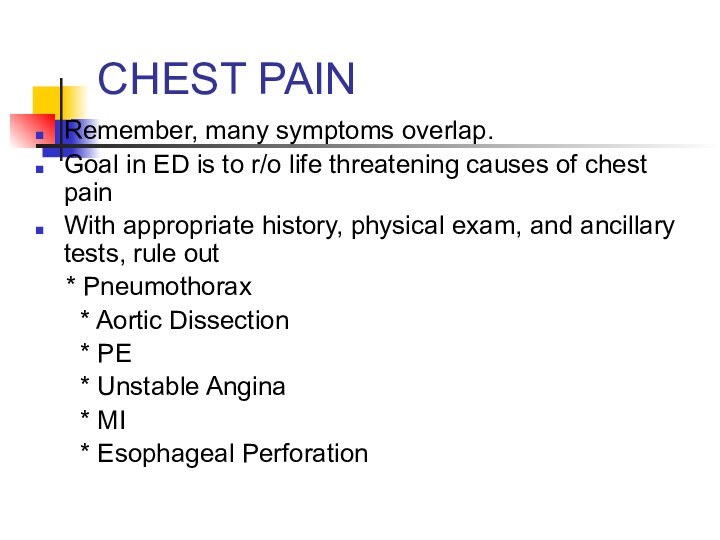
CHEST PAIN5% of all ED visits per yearDifferential diagnosis is difficult








































































Слайд 3
CHEST PAIN
ANATOMY
DIFFERENTIAL DIAGNOSIS
BRIEF OVERVIEW OF DISEASE PROCESSES CAUSING
CHEST PAIN
APPROACH TO CHEST PAIN
Слайд 4
ANATOMY
In devising a differential diagnosis for chest pain,
it becomes essential to review the anatomy of the
thorax.The various components of the thorax can all be responsible for chest pain
Слайд 10
DIFFERENTIAL DIAGNOSIS OF CHEST PAIN
CHEST WALL PAIN
PULMONARY CAUSES
CARDIAC
CAUSES
VASCULAR CAUSES
GI CAUSES
OTHER (PSYCHOGENIC CAUSES)
Слайд 11
DD: CHEST PAIN
CHEST WALL PAIN
1
- Skin and sensory nerves
-Herpes Zoster2 - Musculoskeletal system
- Isolated Musculoskeletal Chest Pain Syndrome
*Costochondritis
*Xiphoidalgia
*Precordial Catch Syndrome
*Rib Fractures
- Rheumatic and Systemic Diseases causing
chest wall pain
Слайд 12
DD: CHEST PAIN
PULMONARY CAUSES
1 - Pulmonary Embolism
2
– Pneumonia
3 - Pneumothorax/ Tension PTX
4 -
Pleuritis/Serositis5 - Sarcoidosis
6 - Asthma/COPD
7 - Lung cancer (rare cases)
Слайд 13
DD: CHEST PAIN
CARDIAC CAUSES
- Coronary
Heart Disease
*Myocardial Ischemia
*Unstable Angina*Angina
- Valvular Heart Disease
*Mitral Valve Prolapse
*Aortic Stenosis
- Pericarditis/Myocarditis
Слайд 15
DD: CHEST PAIN
GI CAUSES
-ESOPHAGEAL
*Reflux
* Esophagitis
* Rupture (Boerhaave Syndrome)* Spasm/Motility Disorder/Foreign Body Secondary to Stricture/Web/Etc
-OTHER
*Consider Pain referred from PUD, Biliary Disease, or Pancreatitis
Слайд 19
CHEST WALL PAIN
HERPES ZOSTER
-Reactivation of Herpes
Varicellae
- Immunocompromised patients often
at risk for
reactivation. - 60% of zoster infections involve the trunk
- Pain may precede rash
Слайд 20
HERPES ZOSTER
Clusters of vesicles (with clear or purulent
fluid) grouped on an erythematous base. Lesions eventually rupture
and crust.Dermatome distribution.
Usually unilateral involvement that halts at midline
Слайд 21
HERPES ZOSTER
TREATMENT:
* Antivirals: reduce duration of
symptoms; incidence of postherpatic neuralgia.
* +/- corticosteroids:
may reduce inflammation* Analgesia
POSTHERPETIC NEURALGIA:
* May follow course of acute zoster
* Shooting, acute pain.
* Hyperesthesia in involved dermatome
* Treatment: analgesics, antidepressants, gabapentin
Слайд 22
CHEST WALL PAIN
Musculoskeletal Pain
- Usually localized, acute,
positional;
- Pain often reproducible by palpation, by turning
or arm movement;- May elicit history of repetitive or unaccustomed activity involving trunk/arms
- Rheumatic diseases will cause musculoskeletal pain via thoracic joint involvement
Слайд 23
MUSCULOSKELETAL PAIN
DIAGNOSIS
COSTOCHONDRITIS
TIETZE SYNDROME
XIPHODYNIA
PRECORDIAL CATCH SYNDROME
RIB FRACTURE
CLINICAL FEATURES
Inflammation of
costal cartilages +/- sternal articulations. No swelling
Painful swelling in
one or more upper costal cartilages.Discomfort over xyphoid reproduced by palpation
Sharp pain lasting for 1-2 min episodes near the cardiac apex and associated with inspiration, poor posture, and inactivity
Pain over involved rib
Слайд 26
PULMONARY EMBOLISM
RISK FACTORS: VIRCHOW’S TRIAD
- Hypercoagulability
*Malignancy
*Pregnancy, Early Postpartum, OCPs, HRT
*Genetic Mutations: Factor V Leiden, Prothrombin, Protein C or S deficiencies, antiphospholipid Ab, etc- Venous Stasis
* Long distance travel
* Prolonged bed rest or recent hospitalization
* Cast
- Venous Injury:
* Recent surgery or Trauma
Слайд 27
PULMONARY EMBOLISM (PE)
CLINICAL FEATURES
- Shortness of
breath
- Chest pain: often pleuritic
-
Tachycardia, tachypnea, hypoxemia- Hemoptysis, Cough
- Consider diagnosis in new onset A fib
- Look for asymmetric leg swelling (signs of
DVT) which places patients at risk for PE
- If massive PE, may present with hypotension, unstable vital signs, and acute cor pulmonale. Also may present with cardiac arrest (PEA >>asystole).
Слайд 28
PE: DIAGNOSTIC TESTS
ECG:
-Sinus tachycardia
most common
- Often see nonspecific abnormalities
- Look for S1 Q3 T3 (S wave in lead I, Q wave in lead III, inverted T wave in lead III)
Слайд 30
PE: DIAGNOSTIC TESTS
CHEST X-RAY
- Normal in
25% of cases
- Often nonspecific findings
- Look for Hampton’s Hump (triangular pleural based density with apex pointed towards hilum): sign of pulmonary infarction-Look for Westermark’s sign: Dilation of pulmonary vessels proximal to embolism and collapse distal
Слайд 32
PE: DIAGNOSTIC TESTS
ABG:
*Look for
abnormal PaO2 or A-a gradient
D-Dimer:
*Often
elevated in PE. * Useful test in low probability patients.
*May be abnormally high in various conditions:
(Malignancy, Pregnancy, sepsis, recent surgery)
Слайд 34
PE: DIAGNOSTIC TESTS
VQ SCAN (Ventilation-Perfusion scan)- use in
setting of renal insufficiency
Helical CT scan with IV contrast
Pulmonary
angiography - Gold Standard
Слайд 35
PE: TREATMENT
Initiate Heparin
* Unfractionated Heparin: 80
Units/Kg bolus IV, then
18units/kg/hr
* Fractionated Heparin (Lovenox): 1mg/kg SubQ BID* If high pre-test probability for PE, initiate empiric heparin
while waiting for imaging
* Make sure no intraparenchymal brain hemorrhage or GI
hemorrhage prior to initiating heparin.
Consider Fibrinolytic Therapy:
* Especially if PE + hypotension
Слайд 36
PNEUMONIA
CLINICAL FEATURES
- Cough +/- sputum production
- Fevers/chills
- Pleuritic chest pain
- Shortness of breath- May be preceded by viral URI symptoms
- Weakness/malaise/ myalgias
- If severe: tachycardia, tachypnea, hypotension
- Decreased sats
-Abnormal findings on pulmonary auscultation: (rales, decreased breath sounds, wheezing, rhonchi)
Слайд 37
PNEUMONIA: DIAGNOSIS
X-Ray
If patient is to be hospitalized:
Consider GBC
(to look for leukocytosis)
Consider sputum cultures
Consider blood cultures
Consider ABG
if in respiratory distress
Слайд 43
PNEUMONIA: TREATMENT
Community- Acquired:
- OUT-PATIENT
*Doxycycline: Low cost option
* Macrolide
*Newer fluoroquinolone: Moxifloxacin, Levofloxacin, Gatifloxacin- IN-PATIENT:
* Second or third generation cephalosporin +macrolide
* Fluoroquinolone: Avelox
Nursing Home: * Zosyn + Erythromcyin
* Clindamycin + Cipro
Слайд 44
SPONTANEOUS PNEUMOTHORAX
RISK FACTORS:
- Primary
* No underlying lung disease
* Young male
with greater height to weight ratio* Smoking: 20:1 relative risk compared to nonsmokers.
-Secondary
* COPD
* Cystic Fibrosis
* AIDS/PCP
* Neoplasms
Слайд 45
PNEUMOTHORAX
CLINICAL FEATURES
- Acute pleuritic chest pain:
95%
- Usually pain localized to side of
PTX- Dyspnea
- May see tachycardia or tachypnea
- Decreased breath sounds on side of PTX
- Hyperresonance on side of PTX
- If tension PTX, will have above findings + tracheal deviation + unstable vital signs. This is rare complication with spontaneous PTX
Слайд 47
TENSION PNEUMOTHORAX
Answer: Chest X-ray should have never been
obtained
Tension PTX is a clinical diagnosis requiring immediate life
saving measures
Слайд 48
Tension Pneumothorax
Trachea deviates to contralateral side
Mediastinum shifts to
contralateral side
Decreased breath sounds and hyperresonance on affected side
JVD
Treatment:
Emergent needle decompression followed by chest tube insertion
Слайд 49
NEEDLE DECOMPRESSION
Insert large bore needle (14 or 16
Gauge) with catheter in the 2nd intercostal space mid-clavicular
line. Remove needle and leave catheter in place. Should hear air.
Слайд 51
SPONTANEOUS PTX
TREATMENT:
- If small (
repeated X-rays
- Give oxygen: Increases pleural air absorption
- If large, place chest tube
Слайд 52
PLEURITIS/SEROSITIS
Inflammation of pleura that covers lung
Pleuritic chest pain
Causes:
- Viral etiology
- SLE
-
Rheumatoid Arthritis- Drugs causing lupus like reaction:
Procainamide, Hydralazine, Isoniazid
Слайд 53
COPD/ASTHMA EXACERBATIONS
CLINICAL FEATURES:
- Decrease in O2
saturations
- Shortness of Breath
- May
see chest pain- Decreased breath sounds, wheezing, or prolonged expiratory phase on exam
- Look for accessory muscle use (nasal flaring, tracheal tugging, retractions).
Order CXR to r/o associated complications: PTX, pneumonia that may have led to exacerbation
Слайд 54
COPD EXACERBATION: TREATMENT
Oxygen: Must prevent hypoxemia. Watch for
hypercapnia with O2 therapy
B2 agonist (albuterol)
Anticholinergic (atrovent)
Corticosteroids
Consider Abx if:
change in sputum or fever)If patient is tiring out, not oxygenating well despite O2, developing worsening respiratory acidosis or mental status changes, then intubate.
Слайд 55
ASTHMA TREATMENT
Oxygen
Inhaled short acting B2 agonists: Albuterol
Anticholinergics: Atrovent
Corticosteroids
Magnesium
Systemic
B2 agonists: Terbutaline
Heliox
If tiring (normalization of CO2/ rising CO2
or mental status changes) or poorly oxygenating despite O2, then intubate
Слайд 57
RISK FACTORS FOR CAD
Age
Diabetes
Hypertension
Family History
Tobacco Use
Hypercholesterolemia
Cocaine use
Слайд 58
ISCHEMIC CHEST PAIN
EXERTIONAL ANGINA
* BRIEF EPISODES
BROUGHT ON BY EXERTION AND RELIEVED BY REST ON
NTGUNSTABLE ANGINA
* NEW ONSET
* CHANGE IN FREQUENCY/SEVERITY
* OCCURS AT REST
AMI
* SEVERE PERSISTENT SYMPTOMS
* ELEVATED TROPONIN
Слайд 59
Angina pectoris
Stable angina pectoris is a clinical syndrome
characterized by precordial or anterior chest discomfort, often with
radiation to the left shoulder or arm.The pain typically accompanies physical activity or emotional stress, although many patients with chronic stable angina pectoris have intermittent rest pain.
The pain may radiate to the left side of the neck or jaw.
Слайд 60
Angina pectoris
The chest discomfort may be described by
the patient either as a true pain or as
a variety of symptoms, such as heaviness, squeezing, tightness, pressure, or aching.True angina is accompanied by some sternal or substernal localization.
Some individuals may experience an associated sensation of dyspnea, which can be the dominant symptom (angina equivalent) in a small number of patients.
Слайд 61
The chest discomfort usually lasts up to 20
minutes; a typical episode of angina rarely lasts longer
than 20 minutes unless the precipitating stimulus continues. Usually, the chest pain abates when the aggravating activity is stopped. Emotion‐triggered symptoms can last longer. Most patients obtain relief from angina in 3 to 10 minutes with sublingual or oral‐spray nitroglycerin.
Слайд 62
ISCHEMIC CHEST PAIN: DIAGNOSIS
12 LEAD EСG
-
Look for ST segment elevation (at least
1mm in two contiguous leads)- Look for ST segment depression
- Look for T wave inversions
- Look for Q waves
- Look for new LBBB
- Always compare to old EСGs
Слайд 68
ISCHEMIC CHEST PAIN: DIAGNOSTIC TESTS
CARDIAC ENZYMES
-
Myoglobin
* Will rise within 3 hours,
peak within 4-9hours, and return to baseline within 24 hrs.
- CKMB
* Will rise within 4 hours, peak within 12- 24
hours and return to baseline in 2-3 days
- TROPONIN I
* Will rise within 6 hours, peak in 12 hours
and return to baseline in 3-4 days
Слайд 69
ISCHEMIC HEART DISEASE TREATMENT:
ACUTE ST SEGMENT ELEVATION MI
- OXYGEN
- ASPIRIN (4 BABY ASPIRIN)
- IV
NITROGLYCERIN* Hold for SBP <100
* Use cautiously in inferior wall MI. Some of these patients have Right
ventricular involvement which is volume/preload dependent.
- BETA BLOCKERS
* Hold for SBP <100 or HR <60
* Hold if wheezing
* Hold if cocaine use (unopposed alpha)
- MORPHINE
- HEPARIN: Before starting,
*Check rectal exam.
*Check CXR: to r/o dissection
- CATH LAB VS TPA
Слайд 70
ISCHEMIC HEART DISEASE TREATMENT: NONSTEMI AND UNSTABLE ANGINA
- OXYGEN
- ASPIRIN (4 BABY ASPIRIN)
- NITROGLYCERIN
* Hold for SBP <100* Use cautiously in inferior wall MI. Some of these patients have Right
ventricular involvement which is volume/preload dependent.
- PLAVIX
- BETA BLOCKERS
* Hold for SBP <100 or HR <60
* Hold if wheezing
* Hold if cocaine use (unopposed alpha)
- MORPHINE
- HEPARIN: Before starting, *Check rectal exam.
*Check CXR: to r/o dissection
Слайд 71
LOW RISK CARDIAC CHEST PAIN
If low risk chest
pain, can consider serial EСGs and enzymes. If normal,
can order stress test in ED if available.
Слайд 72
VALVULAR HEART DISEASE
AORTIC STENOSIS
*Classic triad: dyspnea,
chest pain, and syncope
* Harsh systolic ejection
murmur at right 2nd intercostal space radiating towards carotids* Carotid pulse: slow rate of increase
* Brachioradial delay: Delay in pulses between right brachial and right radial arteries
* Try to avoid nitrates: Theses patients are preload dependent
MITRAL VALVE PROLAPSE
* Symptoms include atypical chest pain, palpitations, fatigue, dyspnea
* Often hear mid-systolic click
* Patients with chest pain or palpitations often respond to β-blockers.
Слайд 73
ACUTE PERICARDITIS
CLINICAL FEATURES
- Acute, stabbing chest pain
- Pleuritic chest pain
- Pain often
referred to left trapezial ridge- Pain more severe when supine.
- Pain often relieved when sitting up and leaning forward
- Listen for pericardial friction rub
Слайд 74
ACUTE PERICARDITIS
COMMON CAUSES
* IDIOPATHIC
*
INFECTIOUS
* MALIGNANCY
* UREMIA
*
RADIATION INDUCED* POST MI (DRESSLER SYNDROME)
* MYXEDEMA
* DRUG INDUCED
* SYSTEMIC RHEUMATIC DISEASES
Слайд 75
ACUTE PERICARDITIS: DIAGNOSTIC TESTS
ECG
*Look for diffuse ST
segment elevation and PR depression.
* If large
pericardial effusion/tamponade, may see low voltage and electrical alternansX-Ray
* Of limited value.
* Look at size of cardiac silhouette
US
*To look for pericardial effusion
Слайд 78
ACUTE PERICARDITIS
TREATMENT:
- If idiopathic or viral:
NSAIDs
- Otherwise treat underlying pathology
Слайд 79
MYOCARDITIS
Inflammation of heart muscle
Frequently accompanied by pericarditis
Fever
Tachycardia out
of proportion to fever
If mild, signs of pericarditis +fevers,
myalgias, rigors, headacheIf severe, will also see signs of heart failure
May see elevated cardiac enzymes
Treatment: Largely supportive
Слайд 81
AORTIC DISSECTION
RISK FACTORS
- UNCONTROLLED HYPERTENSION
- CONGENITAL HEART DISEASE
- CONNECTIVE TISSUE DISEASE
- PREGNANCY- IATROGENIC: S/P AORTIC CATHETERIZATION OR CARDIAC SURGERY
Слайд 82
AORTIC DISSECTION
CLINICAL FEATURES
* Abrupt onset of chest
pain or pain between scapulae
* Tearing or
ripping pain* Pain often worst at symptom onset
* As other vessels become affected, will see
- Stroke symptoms: carotid artery involvement
- Tamponade: Ascending dissection into aortic root
- New onset Aortic Regurgitation
- Abdominal/Flank pain/Limb Ischemia: Dissection into abdominal aorta, renal arteries, iliac arteries
- AMI
* Decreased pulsations in radial, femoral, carotid arteries
* Significant blood pressure differences between extremities
* Usually hypertension (but if tamponade, hypotension)
Слайд 83
DIAGNOSIS: AORTIC DISSECTION
CXR: Look for widened mediastinum
CT SCAN:
ANGIOGRAPHY
TEE
** suspected dissectons must be confirmed radiologically prior to
operative repair.
Слайд 85
AORTIC DISSECTION
TREATMENT:
- ANTIHYPERTENSIVE THERAPY
*Start with beta blockers (smell, labetalol)
* Can add vasodilators (nitroprusside) if further BP control is needed ONLY after have achieved HR control with beta-blockers- If ascending dissection: OR
- If descending: May be able to medically manage
Слайд 88
GERD
RISK FACTORS
* High food fat
* Caffeine
* Nicotine, alcohol
* Medicines:
CCB, nitrates, Anticholinergics* Pregnancy
* DM
* Scleroderma
Слайд 89
GERD
CLINICAL FEATURES
* Burning pain
* Association
with sour taste in mouth, nausea/vomiting
* May
be relieved by antacids* May find association with food
* May mimic ischemic disease and visa versa
TREATMENT
* Can try GI coctail in ED (30cc Mylanta, 10 cc viscous lidocaine)
* H2 blockers and PPI
* Behavior modification:
- Avoid alcohol, nicotine, caffeine, fatty foods
- Avoiding eating prior to sleep.
- Sleep with Head of Bed elevated.
Слайд 90
ESOPHAGITIS
CLINICAL FEATURES
*Chest pain +Odynophagia (pain with
swallowing)
Causes
*Inflammatory process: GERD or med related
*Infectious
process: Candida or HSV (often seen in immunocompromised patients)DIAGNOSIS: Endoscopy with biopsy and culture
TREATMENT: Address underlying pathology
Слайд 91
ESOPHAGEAL PERFORATION
CAUSES
*Iatrogenic: Endoscopy
* Boerhaave Syndrome:
Spontaneous rupture secondary to increased intraesophageal pressure.
- Often presents as sudden onset of chest pain immediately following episode of forceful vomiting*Trauma
*Foreign Body
Слайд 92
ESOPHAGEAL PERFORATION
CLINICAL FEATURES
*Acute persistent chest pain that
may radiate to back, shoulders, neck
* Pain
often worse with swallowing* Shortness of breath
* Tachypnea and abdominal rigidity
* If severe, will see fever, tachycardia, hypotension, subQ emphysema, necrotizing mediastinitis
* Listen for Hammon crunch (pneumomediastinum)
Слайд 93
ESOPHAGEAL PERFORATION
DIAGNOSIS
*x-Ray: May see pleural effusion (usually
on left). Also may see subQ emphysema, pneumomediastinum,pneumothorax
*CT chest* Esophagram
TREATMENT
*Broad spectrum Antibiotics
*Immediate surgical consultation
Слайд 94
ESOPHAGEAL MOTILITY DISORDERS
CLINICAL FEATURES:
* Chest pain
often induced by ingestion of liquids at extremes of
temperature* Often will experience dysphagia
DIAGNOSIS:
Esophageal manometry
Слайд 95
OTHER GI CAUSES
In appropriate setting, consider PUD, Biliary
Disease, and Pancreatitis in differential of chest pain.
Слайд 98
INITIAL APPROACH
Like everything else: ABCs
A: Airway
B: Breathing
C: Circulation
IV, O2, cardiac monitor
Vital
signs
Слайд 99
CHEST PAIN: HISTORY
Time and character of onset
Quality
Location
Radiation
Associated symptoms
Aggravating
symptoms
Alleviating symptoms
Prior episodes
Severity
Review risk factors
Слайд 100
CHEST PAIN: HISTORY
TIME AND CHARACTER OF ONSET:
* Abrupt onset with greatest intensity at start:
-Aortic dissection
-PTX
-Occasionally PE will present in this manner
* Chest pain lasting seconds or constant over weeks is not likely to be due to ischemia
Слайд 101
CHEST PAIN: HISTORY
Quality:
*Pleuritic Pain: PE, Pleurisy,
Pneumonia, Pericarditis, PTX
*Esophageal: Burning, etc
*MI:
squeezing, tightness, pressure, heavy weight on chest. Can also be burning* acute, tearing, ripping pain: Aortic Dissection
Location:
* If very localized, consider chest wall pain or pain of pleural origin
Слайд 102
CHEST PAIN: HISTORY
RADIATION:
* To neck, jaw,
down either arm: consider Ischemia
ASSOCIATED SYMPTOMS:
* Fevers, chills,
URI symptoms, productive cough: Pneumonia* Nausea, vomiting, diaphoresis, shortness of breath: MI
* Shortness of breath: PE, PTX, MI, Pneumonia, COPD / Asthma
* Asymmetric leg swelling: DVT
* With new onset neurologic findings or limb ischemia: consider dissection
* Pain with swallowing, acid taste in mouth: Esophageal disease
Слайд 103
CHEST PAIN: HISTORY
AGGRAVATING SYMPTOMS:
* Activity: consider ischemic
heart disease
* Food: Consider esophageal disease
* Position: If worse with laying back, consider pericarditis* Swallowing: Esophageal disease
* Movement: Chest wall pain
* Respiration: PE, PTX, Pneumonia, pleurisy
* Palpation: Chest Wall Pain
Слайд 104
CHEST PAIN: HISTORY
ALLEVIATING SYMPTOMS
* Rest/ Cessation of
Activity: Ischemic
* NTG: (Cardiac or esophageal)
* Sitting up: Pericarditis* Antacids: Usually GI system
PRIOR EPISODES
* Have they had this kind of pain before
* Does this feel like prior cardiac pain, esophageal pain, etc
* What diagnostic work-up have they had so far?
Last echo, last stress test, last cath, last EGD, etc
SEVERITY
Слайд 105
CHEST PAIN: HISTORY
RISK FACTORS
* Hypertension, DM,
high cholesterol, tobacco, family history: Ischemia
* Long
plane trips, car rides, recent surgery or immobility, hypercoagulable state: PE* Uncontrolled HTN/ Marfan’s: Dissection
* Rheumatic Diseases: Pleurisy
* Smoking: PTX, COPD, Ischemia
Слайд 106
CHEST PAIN: HISTORY
When did the pain start?
What were
you doing when the pain started? Were you at
rest, eating, walking?Did the pain start all of a sudden or gradually build up?
Can you describe the pain to me?
Does it radiate anywhere? Neck, jaw, back. down either arm
Have you had any nausea, vomiting, diaphoresis, or shortness of breath?
Have you had any fevers, chills, URI symptoms, or cough?
Have you been on any long plane trips, car rides, recent surgeries? Have you been bed- bound? Have you noticed any swelling in your legs?
Have you had any tearing sensation in your back/chest?
Does anything make the pain better or worse? Activity, food, deep breath, position, movement, NTG.
Have you ever had this type of pain before. If so what was your diagnosis at that time?
When was the last time you had a stress test, echo, cardiac cath, etc.
Remember to review risk factors!
Слайд 107
CHEST PAIN: PHYSICAL EXAM
Review vital signs
* Fever: Pericarditis, Pneumonia
* Check BP in
both arms: Dissection* Decreased SATs: More commonly in pneumonia, PE, COPD
* Unexplained sinus tachy: consider PE
Neck:
* Look for tracheal deviation: PTX
* Look for JVD: Tension PTX, Tamponade, (CHF)
* Look for accessory muscle use: Respiratory Distress - COPD/Asthma
Chest wall exam
* Look for lesions: Herpes Zoster
* Palpate for localized tenderness: Likely musculoskeletal cause
Lung exam
* Decreased breath sounds/hyperresonance: PTX
* Look for signs of consolidation: Pneumonia
* Listen for wheezing/prolonged expiration: COPD
Слайд 108
CHEST PAIN: PHYSICAL EXAM
CV EXAM
* Assess heart
rate
* Listen for murmurs:
*
Listen for S3/S4* Pericardial friction rub: pericarditis
* Hammon crunch: Esophageal Perforation
* Muffled heart sounds: Tamponade
* Assess distal pulses
ABDOMINAL EXAM
* Assess RUQ and epigastrium (GI disorders that can cause chest pain)
NEURO EXAM
* Chest pain +neurologic findings: consider dissection
Слайд 109
CHEST PAIN: ANCILLARY TESTING
LABS: Consider…….
* Baseline labs:
CBC, BMP, PT/PTT
* D dimer (PE)
* Blood cultures (pneumonia)* Sputum cultures (pneumonia)
* Peak flow (Asthma)
* ABG
* Cardiac Enzymes ( MI)
* Urine tox (cocaine- MI)
* ESR (pericarditis)
ECG
Слайд 110
CHEST PAIN: ANCILLARY TESTS
IMAGING: CONSIDER……
* x-Ray
- Rib fractures
-
Hampton’s Hump/ Westermark’s sign: PE- Infiltrates: Pneumonia
- Widened mediastinum: Aortic dissection
- Pneumothorax
- Cardiac size: enlarged silhouette without CHF: pericardial effusion
* CT CHEST if suspect PE or Aortic Dissection
* VQ SCAN: PE
* STRESS TESTS: Angina
* CATH: Ischemia
* ECHO
* EGD: Esophageal disease