Слайд 2
Introduction
Contraception is a part of Family Planning
(Contraception -
recurrent abortion and infertility management - genetic counseling)
Regulation of
family size
Wide range of methods is available
No ideal contraception exists
Contraception failure ( the perfect use rate - the typical rate )
Intelligent choice of contraception :
Medical care provider (information , advice) + Couple (needs)
Слайд 3
Stratification
Physiological - Natural
Hormonal
Mechanical - Barrier
Chemical
Oral - Vaginal
Intrauterine Device
Injectable
- Implant
Temporary - Permanent
Emergency contraception
Слайд 4
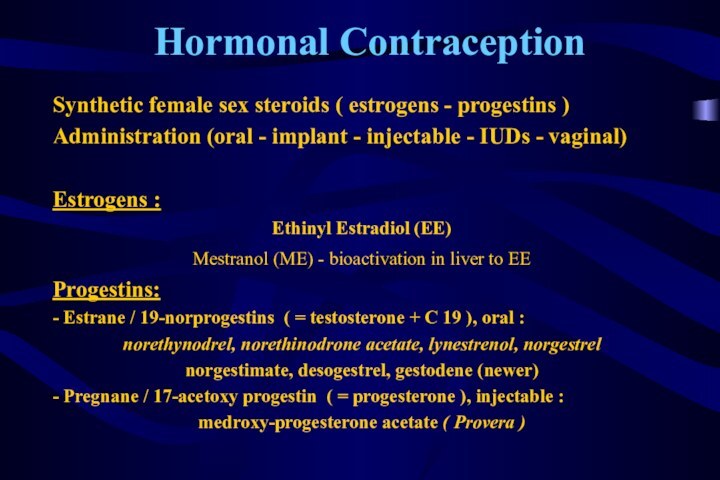
Hormonal Contraception
Synthetic female sex steroids ( estrogens -
progestins )
Administration (oral - implant - injectable - IUDs
- vaginal)
Estrogens :
Ethinyl Estradiol (EE)
Mestranol (ME) - bioactivation in liver to EE
Progestins:
- Estrane / 19-norprogestins ( = testosterone + C 19 ), oral :
norethynodrel, norethinodrone acetate, lynestrenol, norgestrel
norgestimate, desogestrel, gestodene (newer)
- Pregnane / 17-acetoxy progestin ( = progesterone ), injectable :
medroxy-progesterone acetate ( Provera )
Слайд 5
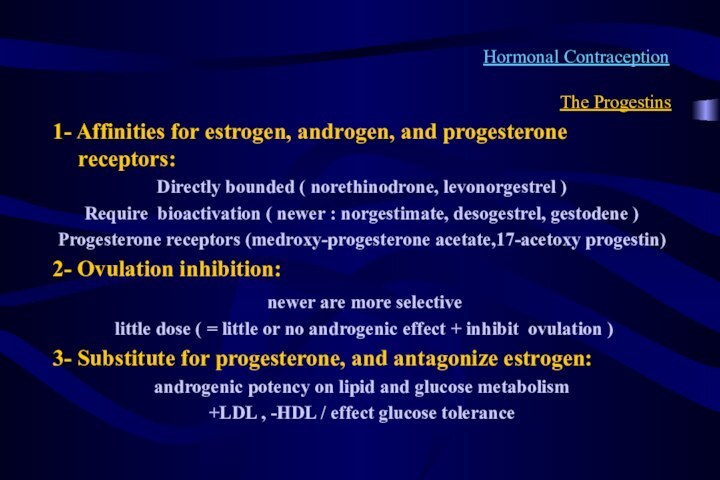
Hormonal Contraception
The Progestins
1- Affinities for estrogen, androgen, and
progesterone receptors:
Directly bounded ( norethinodrone, levonorgestrel )
Require bioactivation (
newer : norgestimate, desogestrel, gestodene )
Progesterone receptors (medroxy-progesterone acetate,17-acetoxy progestin)
2- Ovulation inhibition:
newer are more selective
little dose ( = little or no androgenic effect + inhibit ovulation )
3- Substitute for progesterone, and antagonize estrogen:
androgenic potency on lipid and glucose metabolism
+LDL , -HDL / effect glucose tolerance
Слайд 6
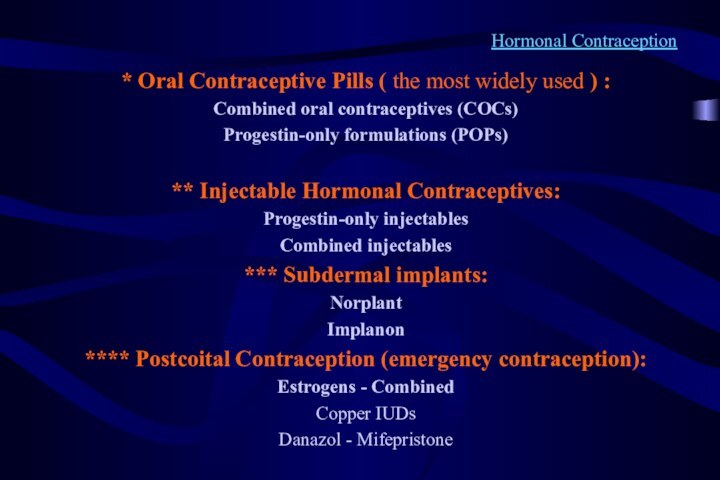
Hormonal Contraception
* Oral Contraceptive Pills ( the most
widely used ) :
Combined oral contraceptives (COCs)
Progestin-only formulations (POPs)
**
Injectable Hormonal Contraceptives:
Progestin-only injectables
Combined injectables
*** Subdermal implants:
Norplant
Implanon
**** Postcoital Contraception (emergency contraception):
Estrogens - Combined
Copper IUDs
Danazol - Mifepristone
Слайд 7
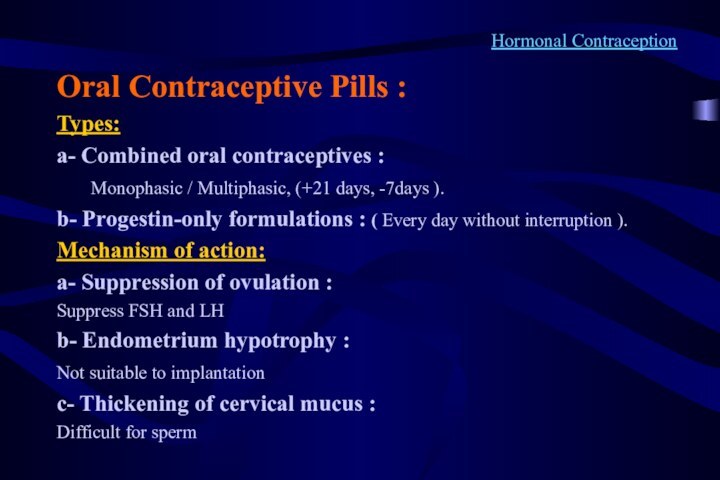
Hormonal Contraception
Oral Contraceptive Pills :
Types:
a- Combined oral contraceptives
:
Monophasic / Multiphasic, (+21 days, -7days
).
b- Progestin-only formulations : ( Every day without interruption ).
Mechanism of action:
a- Suppression of ovulation :
Suppress FSH and LH
b- Endometrium hypotrophy :
Not suitable to implantation
c- Thickening of cervical mucus :
Difficult for sperm
Слайд 8
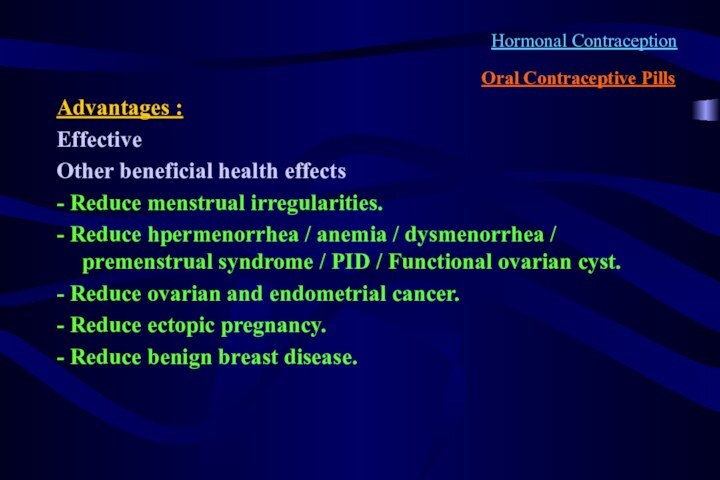
Hormonal Contraception
Oral Contraceptive Pills
Advantages :
Effective
Other beneficial health effects
-
Reduce menstrual irregularities.
- Reduce hpermenorrhea / anemia / dysmenorrhea
/ premenstrual syndrome / PID / Functional ovarian cyst.
- Reduce ovarian and endometrial cancer.
- Reduce ectopic pregnancy.
- Reduce benign breast disease.
Слайд 9
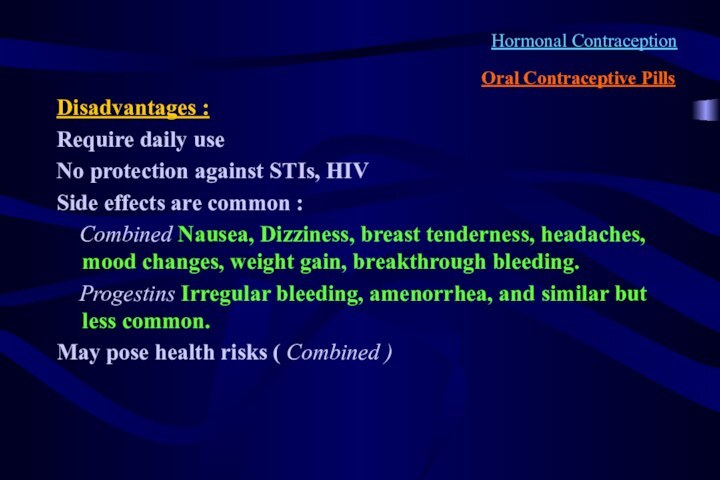
Hormonal Contraception
Oral Contraceptive Pills
Disadvantages :
Require daily use
No protection
against STIs, HIV
Side effects are common :
Combined Nausea, Dizziness, breast tenderness, headaches, mood changes, weight gain, breakthrough bleeding.
Progestins Irregular bleeding, amenorrhea, and similar but less common.
May pose health risks ( Combined )
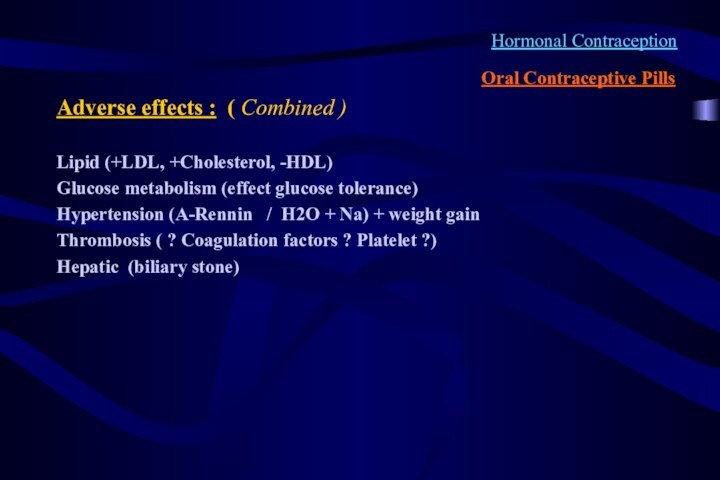
Слайд 10
Hormonal Contraception
Oral Contraceptive Pills
Adverse effects : ( Combined
)
Lipid (+LDL, +Cholesterol, -HDL)
Glucose metabolism (effect glucose tolerance)
Hypertension (A-Rennin
/ H2O + Na) + weight gain
Thrombosis ( ? Coagulation factors ? Platelet ?)
Hepatic (biliary stone)
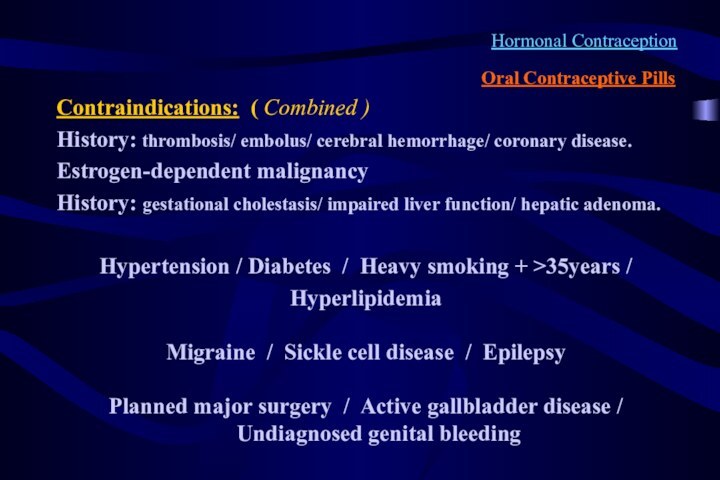
Слайд 11
Hormonal Contraception
Oral Contraceptive Pills
Contraindications: ( Combined )
History: thrombosis/
embolus/ cerebral hemorrhage/ coronary disease.
Estrogen-dependent malignancy
History: gestational cholestasis/
impaired liver function/ hepatic adenoma.
Hypertension / Diabetes / Heavy smoking + >35years /
Hyperlipidemia
Migraine / Sickle cell disease / Epilepsy
Planned major surgery / Active gallbladder disease / Undiagnosed genital bleeding
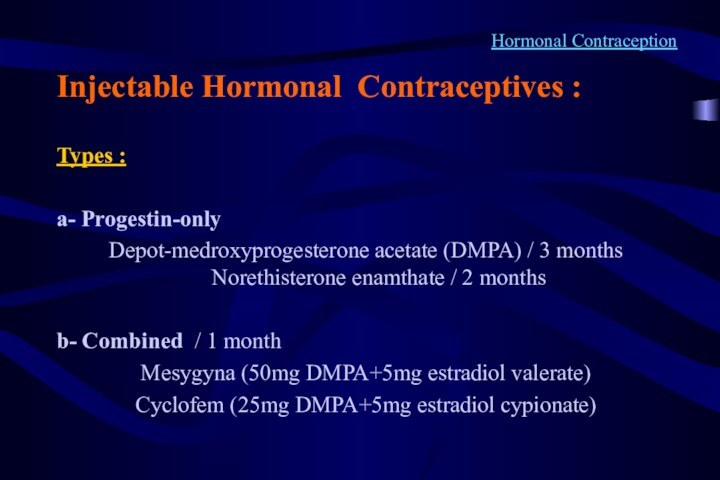
Слайд 12
Hormonal Contraception
Injectable Hormonal Contraceptives :
Types :
a- Progestin-only
Depot-medroxyprogesterone acetate
(DMPA) / 3 months Norethisterone enamthate / 2 months
b- Combined / 1 month
Mesygyna (50mg DMPA+5mg estradiol valerate)
Cyclofem (25mg DMPA+5mg estradiol cypionate)
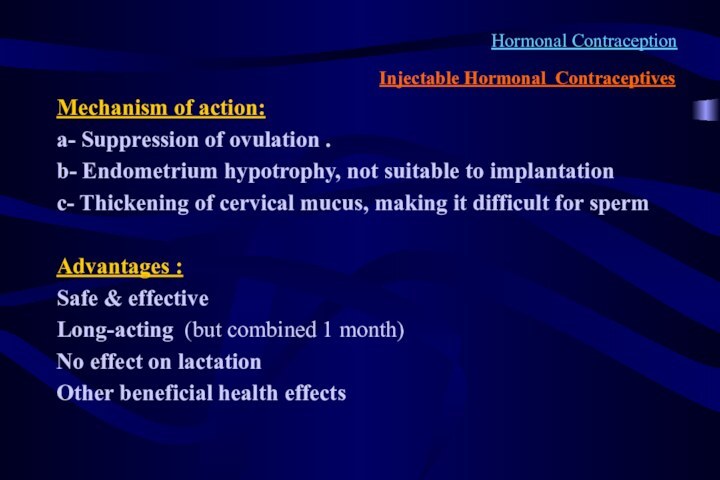
Слайд 13
Hormonal Contraception
Injectable Hormonal Contraceptives
Mechanism of action:
a- Suppression of
ovulation .
b- Endometrium hypotrophy, not suitable to implantation
c-
Thickening of cervical mucus, making it difficult for sperm
Advantages :
Safe & effective
Long-acting (but combined 1 month)
No effect on lactation
Other beneficial health effects
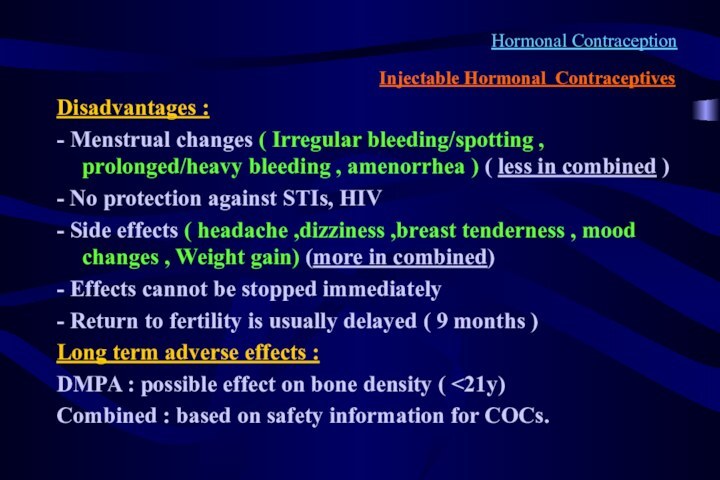
Слайд 14
Hormonal Contraception
Injectable Hormonal Contraceptives
Disadvantages :
- Menstrual changes (
Irregular bleeding/spotting , prolonged/heavy bleeding , amenorrhea ) (
less in combined )
- No protection against STIs, HIV
- Side effects ( headache ,dizziness ,breast tenderness , mood changes , Weight gain) (more in combined)
- Effects cannot be stopped immediately
- Return to fertility is usually delayed ( 9 months )
Long term adverse effects :
DMPA : possible effect on bone density ( <21y)
Combined : based on safety information for COCs.
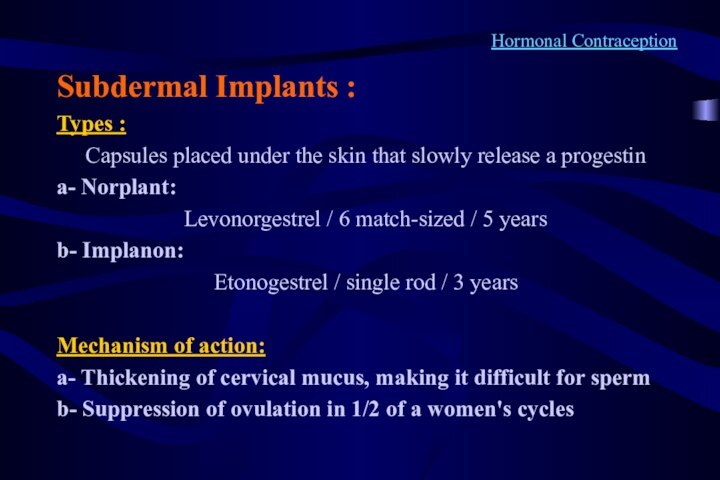
Слайд 15
Hormonal Contraception
Subdermal Implants :
Types :
Capsules placed under the
skin that slowly release a progestin
a- Norplant:
Levonorgestrel / 6
match-sized / 5 years
b- Implanon:
Etonogestrel / single rod / 3 years
Mechanism of action:
a- Thickening of cervical mucus, making it difficult for sperm
b- Suppression of ovulation in 1/2 of a women's cycles
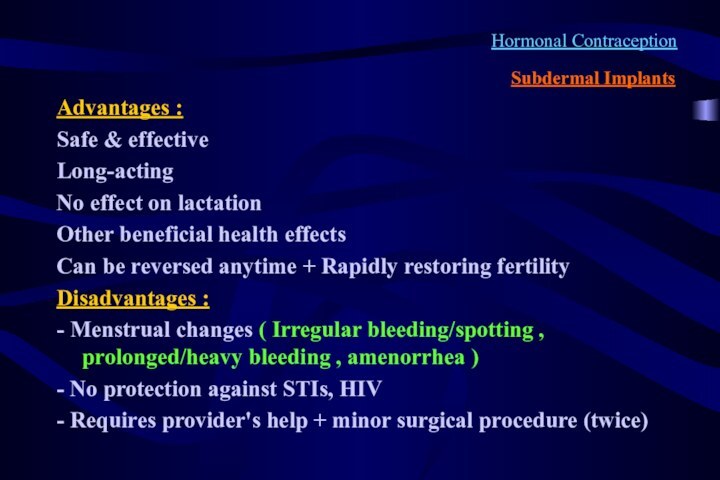
Слайд 16
Hormonal Contraception
Subdermal Implants
Advantages :
Safe & effective
Long-acting
No effect
on lactation
Other beneficial health effects
Can be reversed anytime +
Rapidly restoring fertility
Disadvantages :
- Menstrual changes ( Irregular bleeding/spotting , prolonged/heavy bleeding , amenorrhea )
- No protection against STIs, HIV
- Requires provider's help + minor surgical procedure (twice)
Слайд 17
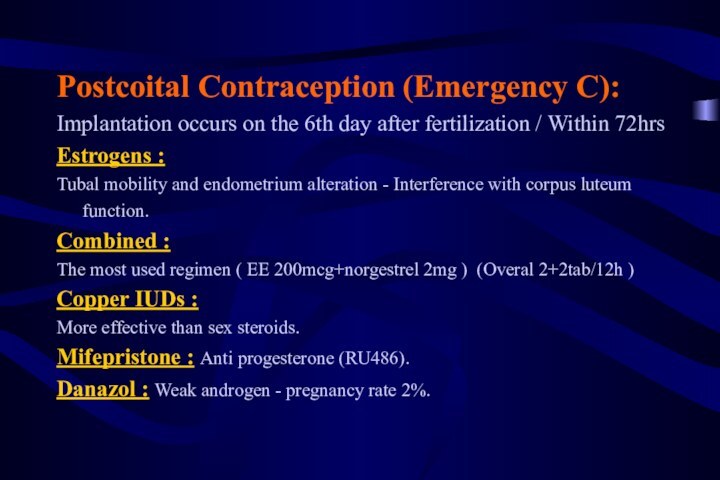
Postcoital Contraception (Emergency C):
Implantation occurs on the
6th day after fertilization / Within 72hrs
Estrogens :
Tubal
mobility and endometrium alteration - Interference with corpus luteum function.
Combined :
The most used regimen ( EE 200mcg+norgestrel 2mg ) (Overal 2+2tab/12h )
Copper IUDs :
More effective than sex steroids.
Mifepristone : Anti progesterone (RU486).
Danazol : Weak androgen - pregnancy rate 2%.
Слайд 18
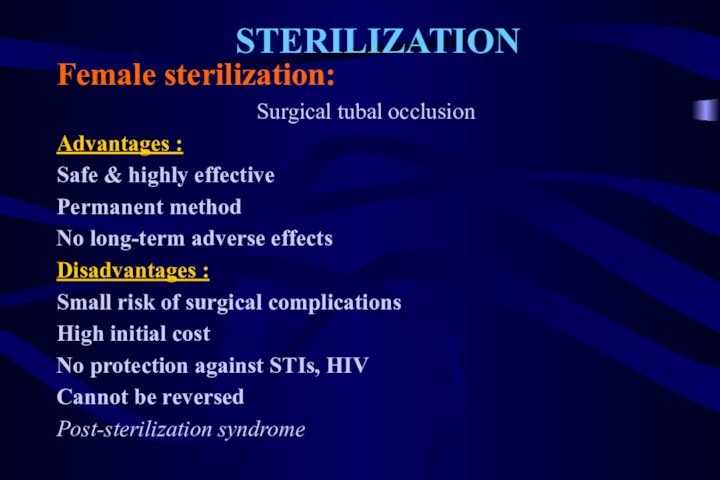
STERILIZATION
Female sterilization:
Surgical tubal occlusion
Advantages :
Safe & highly effective
Permanent
method
No long-term adverse effects
Disadvantages :
Small risk of surgical complications
High initial cost
No protection against STIs, HIV
Cannot be reversed
Post-sterilization syndrome
Слайд 19
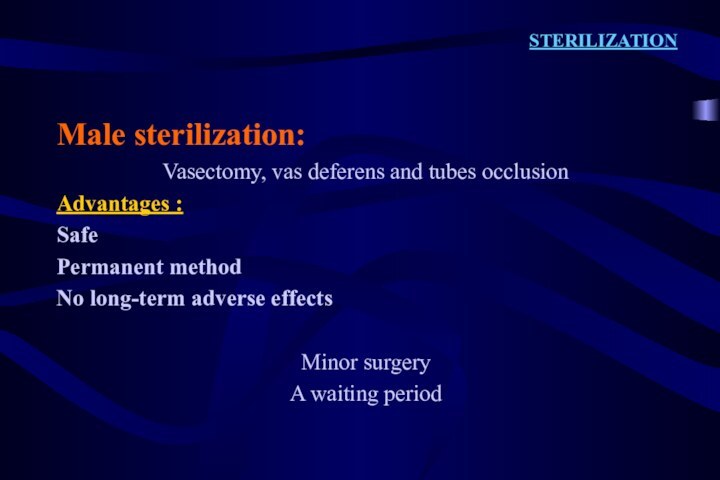
STERILIZATION
Male sterilization:
Vasectomy, vas deferens and tubes occlusion
Advantages
:
Safe
Permanent method
No long-term adverse effects
Minor surgery
A waiting period
Слайд 20
Non Hormonal Contraception
* Lactational amenorrhea method (LAM)
** Periodic
abstinence
*** Coitus interruptus
**** Barrier methods
Male, female condom
/ Diaphragm / Cervical cap
Vaginal spermicides
Слайд 21
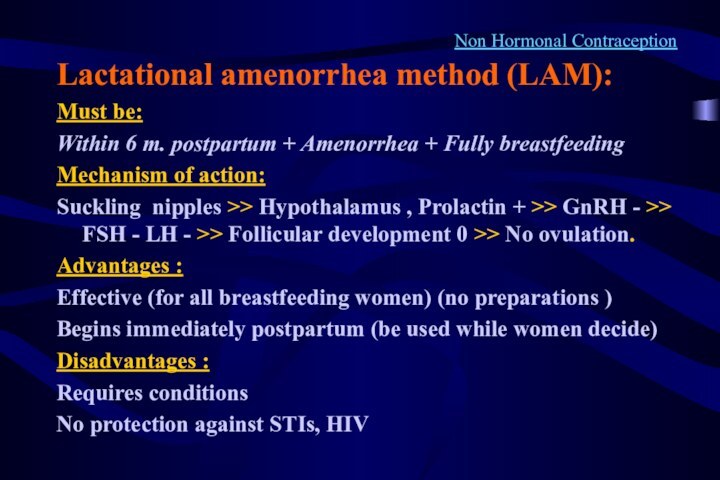
Non Hormonal Contraception
Lactational amenorrhea method (LAM):
Must be:
Within 6
m. postpartum + Amenorrhea + Fully breastfeeding
Mechanism of action:
Suckling
nipples >> Hypothalamus , Prolactin + >> GnRH - >> FSH - LH - >> Follicular development 0 >> No ovulation.
Advantages :
Effective (for all breastfeeding women) (no preparations )
Begins immediately postpartum (be used while women decide)
Disadvantages :
Requires conditions
No protection against STIs, HIV
Слайд 22
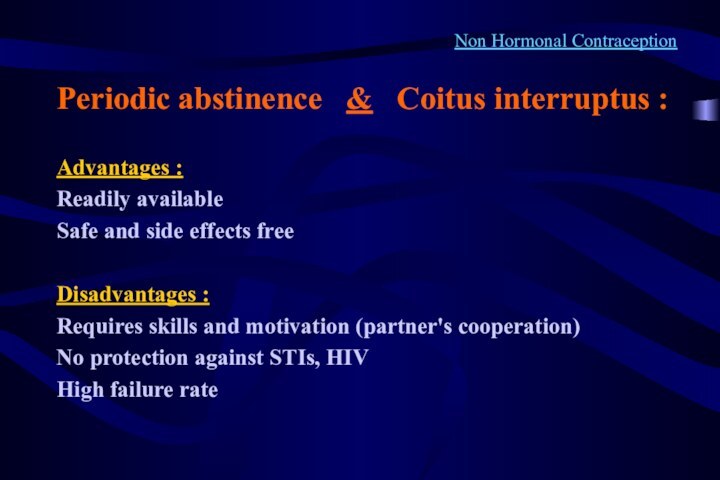
Non Hormonal Contraception
Periodic abstinence & Coitus
interruptus :
Advantages :
Readily available
Safe and side effects free
Disadvantages :
Requires
skills and motivation (partner's cooperation)
No protection against STIs, HIV
High failure rate
Слайд 23
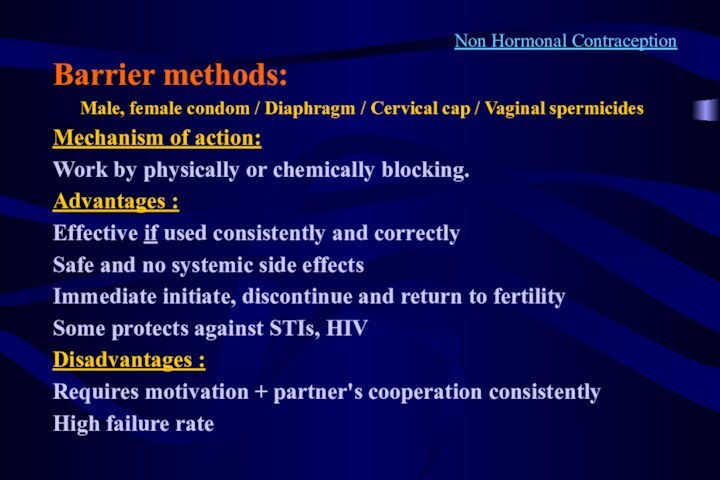
Non Hormonal Contraception
Barrier methods:
Male, female condom / Diaphragm
/ Cervical cap / Vaginal spermicides
Mechanism of action:
Work by
physically or chemically blocking.
Advantages :
Effective if used consistently and correctly
Safe and no systemic side effects
Immediate initiate, discontinue and return to fertility
Some protects against STIs, HIV
Disadvantages :
Requires motivation + partner's cooperation consistently
High failure rate
Слайд 24
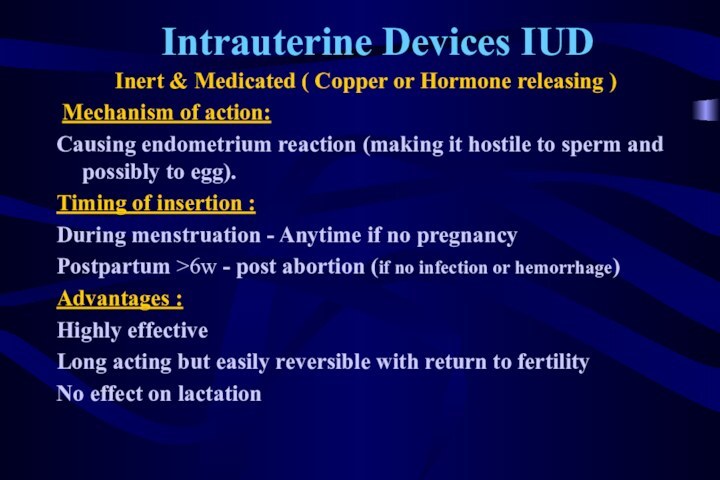
Intrauterine Devices IUD
Inert & Medicated ( Copper or
Hormone releasing )
Mechanism of action:
Causing endometrium reaction (making
it hostile to sperm and possibly to egg).
Timing of insertion :
During menstruation - Anytime if no pregnancy
Postpartum >6w - post abortion (if no infection or hemorrhage)
Advantages :
Highly effective
Long acting but easily reversible with return to fertility
No effect on lactation
Слайд 25
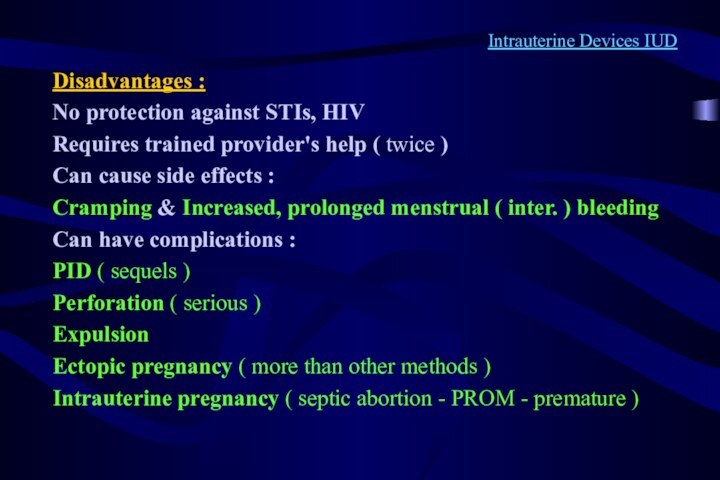
Intrauterine Devices IUD
Disadvantages :
No protection against STIs, HIV
Requires
trained provider's help ( twice )
Can cause side effects
:
Cramping & Increased, prolonged menstrual ( inter. ) bleeding
Can have complications :
PID ( sequels )
Perforation ( serious )
Expulsion
Ectopic pregnancy ( more than other methods )
Intrauterine pregnancy ( septic abortion - PROM - premature )
Слайд 26
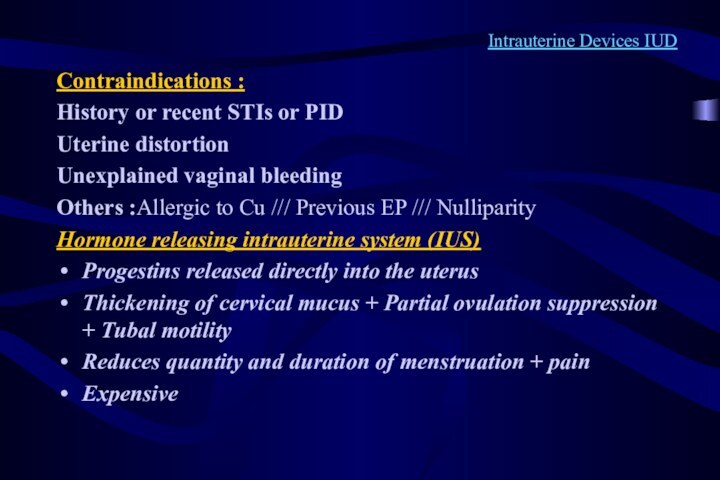
Intrauterine Devices IUD
Contraindications :
History or recent STIs or
PID
Uterine distortion
Unexplained vaginal bleeding
Others :Allergic to Cu /// Previous
EP /// Nulliparity
Hormone releasing intrauterine system (IUS)
Progestins released directly into the uterus
Thickening of cervical mucus + Partial ovulation suppression + Tubal motility
Reduces quantity and duration of menstruation + pain
Expensive
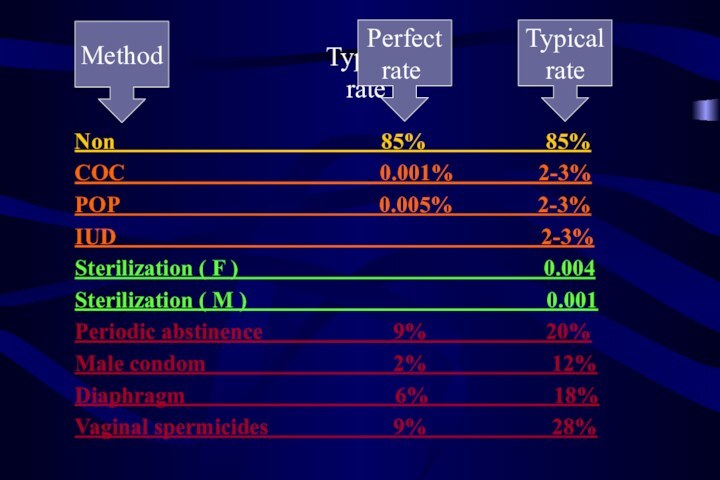
85% 85%
COC 0.001% 2-3%
POP 0.005% 2-3%
IUD 2-3%
Sterilization ( F ) 0.004
Sterilization ( M ) 0.001
Periodic abstinence 9% 20%
Male condom 2% 12%
Diaphragm 6% 18%
Vaginal spermicides 9% 28%
Typical
rate
Perfect
rate
Method
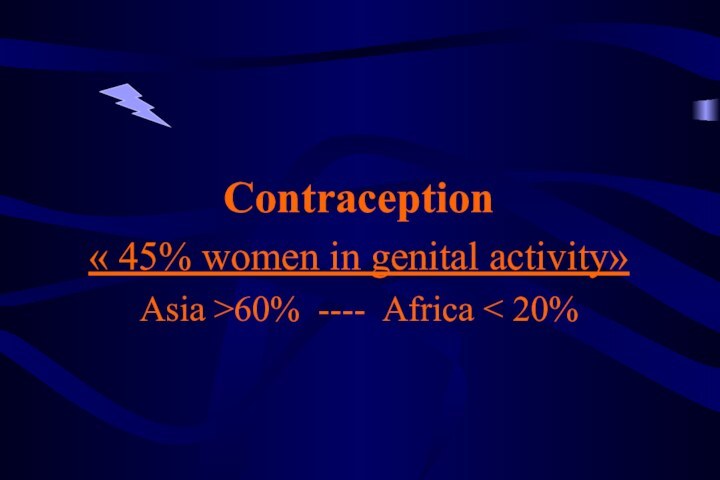
Contraception
« 45% women in genital activity»
Asia >60% ---- Africa < 20%