Слайд 2
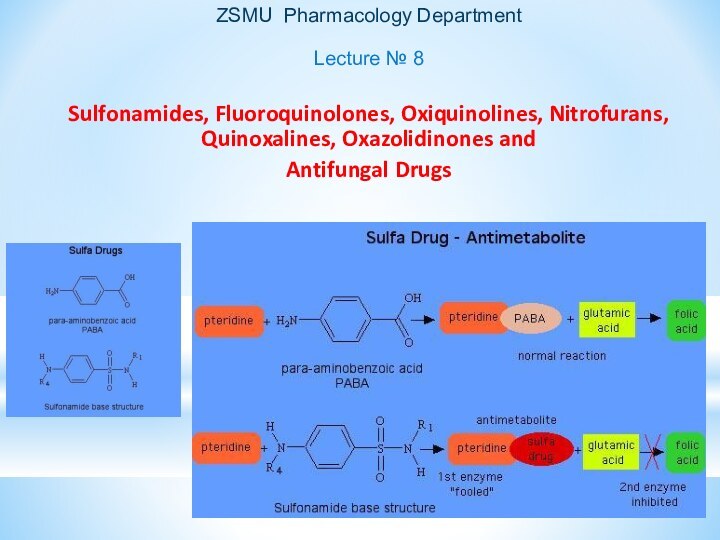
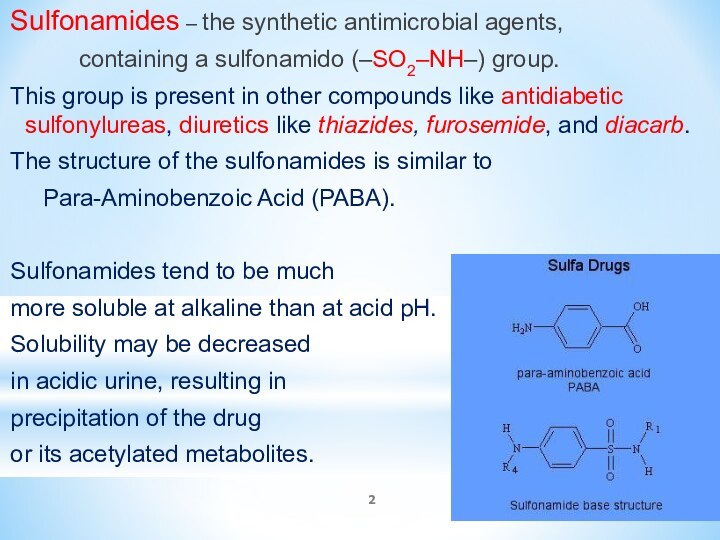
Sulfonamides – the synthetic antimicrobial agents,
containing a
sulfonamido (–SO2–NH–) group.
This group is present in other compounds
like antidiabetic sulfonylureas, diuretics like thiazides, furosemide, and diacarb.
The structure of the sulfonamides is similar to
Para-Aminobenzoic Acid (PABA).
Sulfonamides tend to be much
more soluble at alkaline than at acid pH.
Solubility may be decreased
in acidic urine, resulting in
precipitation of the drug
or its acetylated metabolites.
Слайд 3
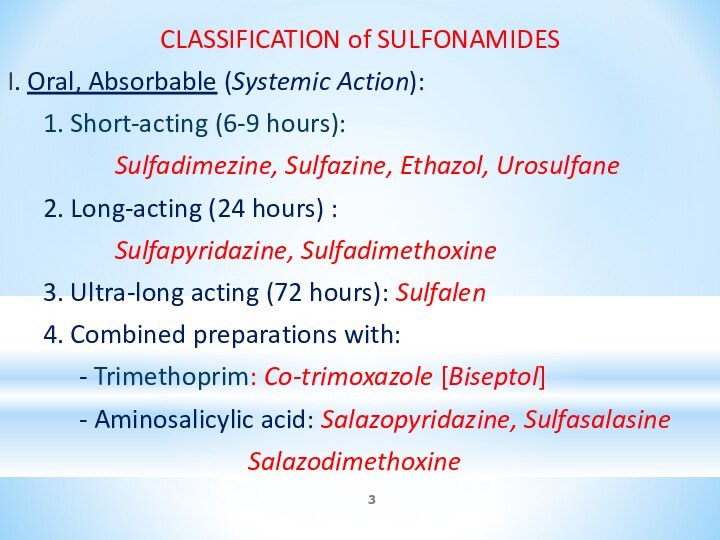
CLASSIFICATION of SULFONAMIDES
I. Oral, Absorbable (Systemic Action):
1. Short-acting
(6-9 hours):
Sulfadimezine, Sulfazine, Ethazol, Urosulfane
2. Long-acting (24 hours)
:
Sulfapyridazine, Sulfadimethoxine
3. Ultra-long acting (72 hours): Sulfalen
4. Combined preparations with:
- Trimethoprim: Co-trimoxazole [Biseptol]
- Aminosalicylic acid: Salazopyridazine, Sulfasalasine
Salazodimethoxine
Слайд 4
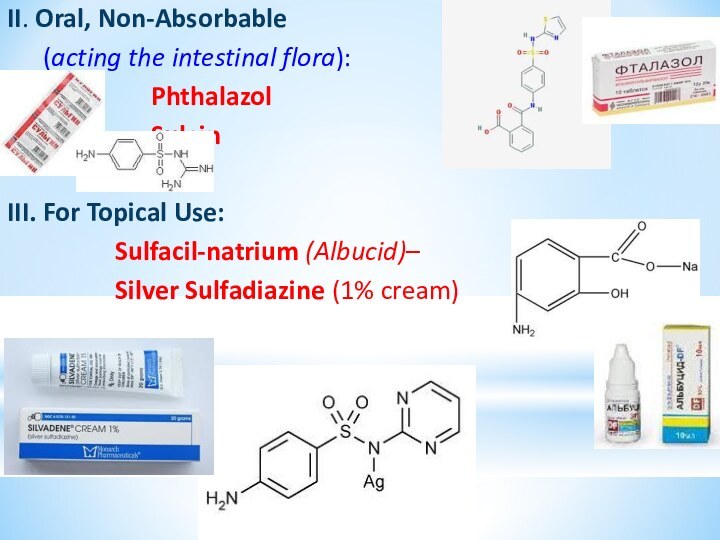
II. Oral, Non-Absorbable
(acting the intestinal flora):
Phthalazol
Sulgin
III. For
Topical Use:
Sulfacil-natrium (Albucid)–
Silver Sulfadiazine (1% cream)
Слайд 6
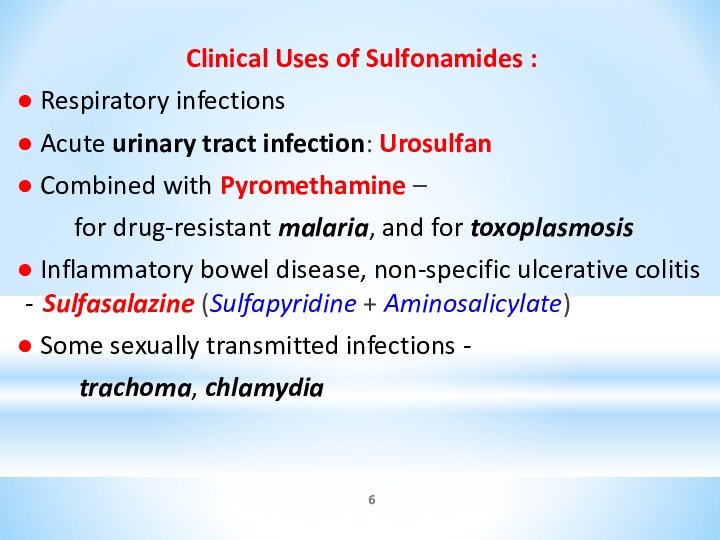
Clinical Uses of Sulfonamides :
● Respiratory infections
● Acute urinary tract infection: Urosulfan
● Combined with
Pyromethamine –
for drug-resistant malaria, and for toxoplasmosis
● Inflammatory bowel disease, non-specific ulcerative colitis - Sulfasalazine (Sulfapyridine + Aminosalicylate)
● Some sexually transmitted infections -
trachoma, chlamydia
Слайд 7
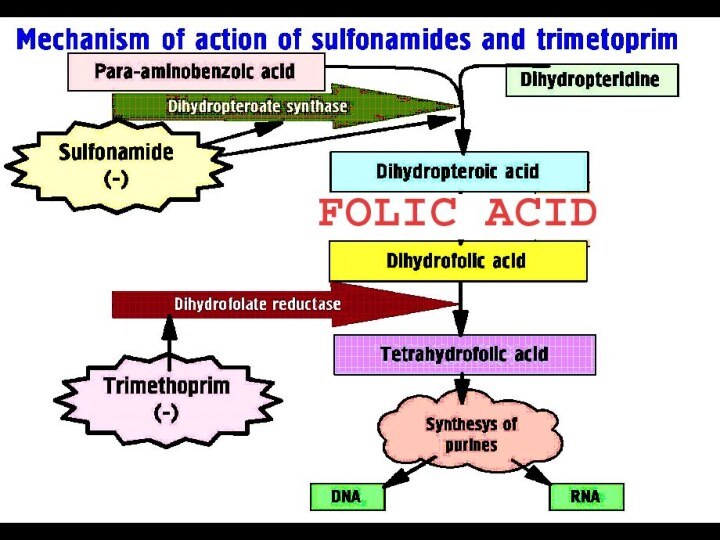
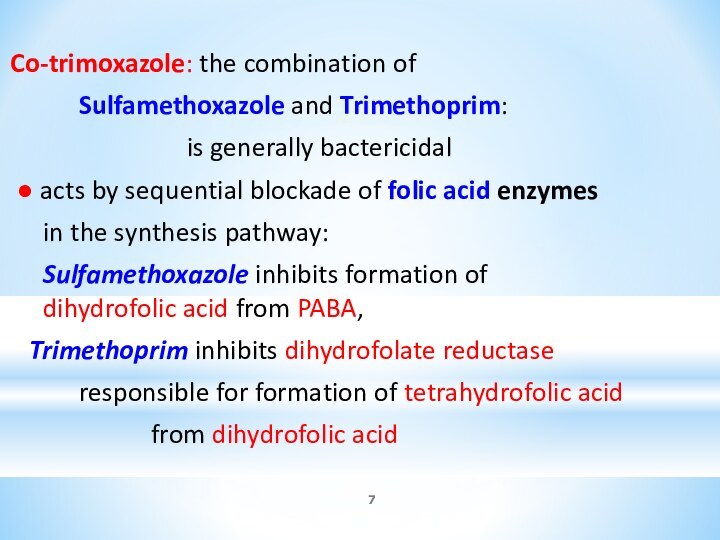
Co-trimoxazole: the combination of
Sulfamethoxazole and Trimethoprim:
is generally
bactericidal
● acts by sequential blockade of folic acid
enzymes
in the synthesis pathway:
Sulfamethoxazole inhibits formation of dihydrofolic acid from PABA,
Trimethoprim inhibits dihydrofolate reductase
responsible for formation of tetrahydrofolic acid
from dihydrofolic acid
Слайд 8
Co-trimoxazole is effective against :
Escherihia coli
Klebsiella
Enterobacter
Streptococcus pneumoniae
Staphylococcus aureus
Salmonella
Shigella
Clinical uses: Chronic Bronchitis,
Urinary tract infections, Otitis media,
Pneumocytis carini pneumonitis, Traveller’s Diarrhea, Pertussis, Cholera.
Слайд 9
Adverse Effects of Sulfonmides:
● Hypersensitivity Reactions: rashes, angioedema.
All sulfonamides and their derivatives, including
Diacarb, Thiazides, Furosemide,
Glibenclamide, Diazoxide are CROSS-ALLERGIC
● Nephrotoxicity, Urinary tract disturbances:
Sulfonamides precipitate in urine, esp. at neutral or acid pH, producing crystalluria, haematuria, or even obstruction.
Adequate HYDRATION and ALKALINIZATION of urine
prevent the problem
● Haemopoietic disturbances: hemolytic anemia,
agranulocytosis, leukopenia, thrombocytopenia
● CNS: Depression, aseptic meningitis, seizures
Слайд 10
Acute Poisoning/Overdose with Sulfonamides
Sulfonamides are able to:
● form methemoglobin and sulf-methemoglobine,
●
block the haemopoiesis and
● produce hepato- and nephrotoxicity.
Manifestation: dizziness, drowsiness, unconsciousness, anorexia,
abdominal pain, nausea, vomiting, haemolytic anemia, acidosis,
agranulocytosis, sensitivity reactions, jaundice, hepatomegalia
Treatment: gastric lavage, forced diuresis
ANTIDOTES:
Nicotinic acid IV 1% solution 2–5 ml or Nicotinamide
Chromosmon (1% Methylene Blue solution in 25% glucose)
IV 0.1 ml/kg
Lipoic acid IV 0.5% solution 60-80 ml
Folic acid PO 1 mg tid
Transfusion of appropriate BLOOD PRODUCT:
Fresh blood, Dry Plasma, Polyglucin , Rheopolyglucin
Слайд 11
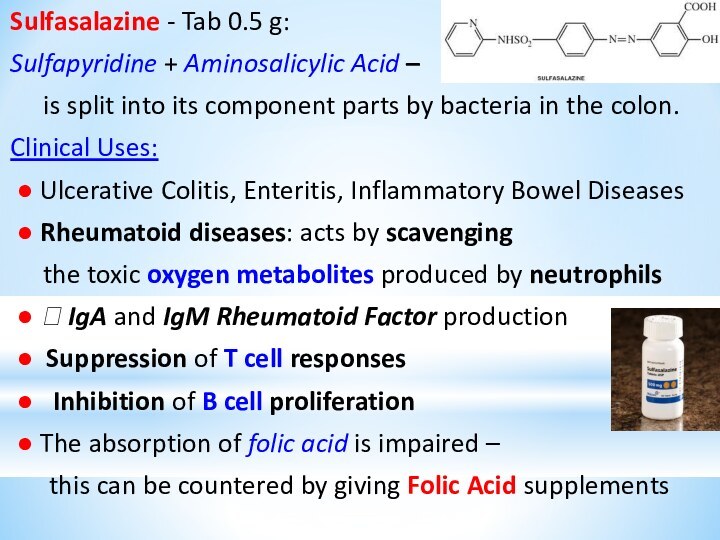
Sulfasalazine - Tab 0.5 g:
Sulfapyridine + Aminosalicylic
Acid –
is split into its component parts by
bacteria in the colon.
Clinical Uses:
● Ulcerative Colitis, Enteritis, Inflammatory Bowel Diseases
● Rheumatoid diseases: acts by scavenging
the toxic oxygen metabolites produced by neutrophils
● ? IgA and IgM Rheumatoid Factor production
● Suppression of T cell responses
● Inhibition of B cell proliferation
● The absorption of folic acid is impaired –
this can be countered by giving Folic Acid supplements
Слайд 12
Sulfacyl-sodium (Albucid) –
10%, 15%,
30% ophthalmic solution or
ointment -
effective for:
● Bacterial Conjunctivitis and
as adjunctive therapy for Trachoma.
● Ocular gonorrheal infection in newborns and adults.
It acts by inhibiting the uptake of PABA, which is required in the synthesis of Folic Acid needed for bacterial growth.
Слайд 15
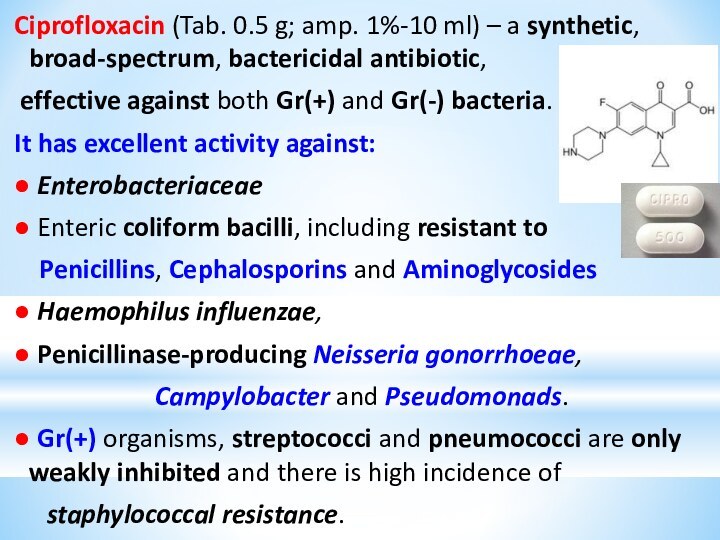
Ciprofloxacin (Tab. 0.5 g; amp. 1%-10 ml) –
a synthetic, broad-spectrum, bactericidal antibiotic,
effective against both
Gr(+) and Gr(-) bacteria.
It has excellent activity against:
● Enterobacteriaceae
● Enteric coliform bacilli, including resistant to
Penicillins, Cephalosporins and Aminoglycosides
● Haemophilus influenzae,
● Penicillinase-producing Neisseria gonorrhoeae,
Campylobacter and Pseudomonads.
● Gr(+) organisms, streptococci and pneumococci are only weakly inhibited and there is high incidence of
staphylococcal resistance.
Слайд 16
Clinical uses of Fluoroquinolones
● Urinary tract infections: Norfloxacin,
Ofloxacin
● Complicated respiratory tract infections - Gr(-) flora
Pseudomonas aeruginosa respiratory
infection
● External otitis caused by P. aeruginosa
● Chronic Gr(-) bacillary osteomyelitis
● Eradication of Salmonella typhi in carriers
● Gonorrhoea: Norfloxacin, Ofloxacin
● Anthrax
Слайд 17
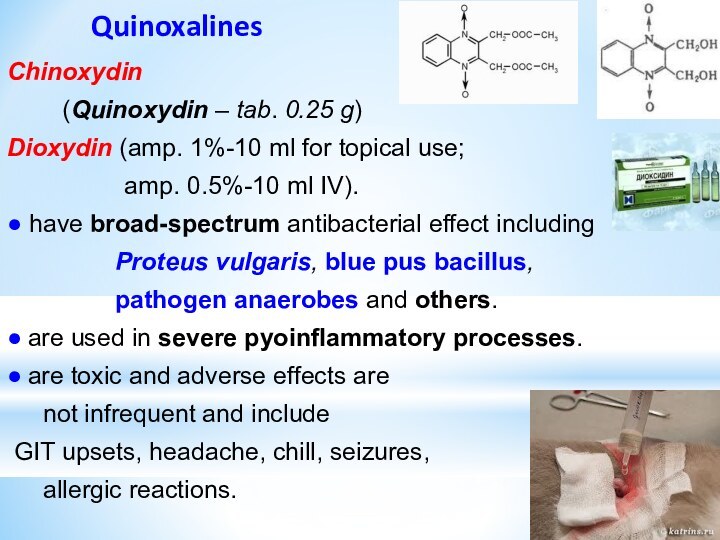
Quinoxalines
Chinoxydin
(Quinoxydin – tab. 0.25 g)
Dioxydin (amp. 1%-10
ml for topical use;
amp. 0.5%-10 ml IV).
● have broad-spectrum antibacterial effect including
Proteus vulgaris, blue pus bacillus,
pathogen anaerobes and others.
● are used in severe pyoinflammatory processes.
● are toxic and adverse effects are
not infrequent and include
GIT upsets, headache, chill, seizures,
allergic reactions.
Слайд 18
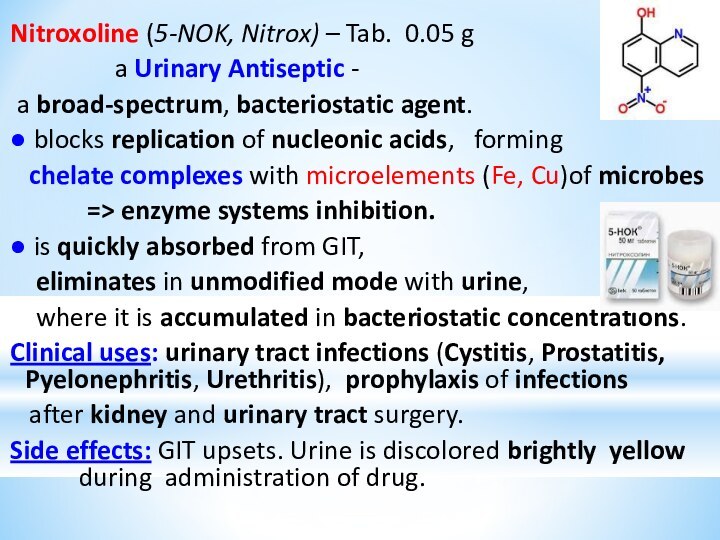
Nitroxoline (5-NOK, Nitrox) – Tab. 0.05 g
a
Urinary Antiseptic -
a broad-spectrum, bacteriostatic agent.
● blocks replication
of nucleonic acids, forming
chelate complexes with microelements (Fe, Cu)of microbes
=> enzyme systems inhibition.
● is quickly absorbed from GIT,
eliminates in unmodified mode with urine,
where it is accumulated in bacteriostatic concentrations.
Clinical uses: urinary tract infections (Cystitis, Prostatitis, Pyelonephritis, Urethritis), prophylaxis of infections
after kidney and urinary tract surgery.
Side effects: GIT upsets. Urine is discolored brightly yellow during administration of drug.
Слайд 20
Furacilin (Nitrofurazone, Furacin)
0.02% water solution, Tab. 0.02
and 0.1 g -
is a synthetic, broad-spectrum antibacterial nitrofuran
derivative used mainly for topic application as ANTISEPTIC:
● Externally for the treatment and prevention of pyoinflammatory processes, major burns
(esp. when resistance to other antibacterial agents occurs);
● Prevention of skin graft infections.
0.02% Furacilin Solution is applied directly to lesion or to dressing used to cover the affected area daily or
as indicated,
depending on severity of
burn or injury.
Слайд 21
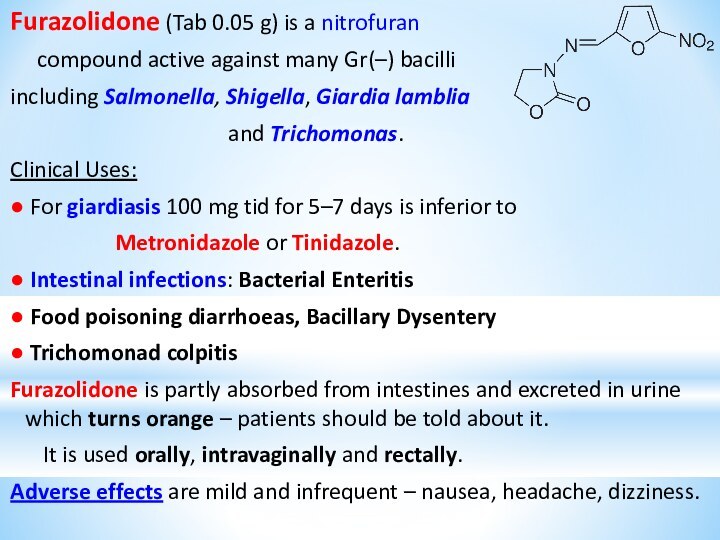
Furazolidone (Tab 0.05 g) is a nitrofuran
compound active against many Gr(–) bacilli
including
Salmonella, Shigella, Giardia lamblia
and Trichomonas.
Clinical Uses:
● For giardiasis 100 mg tid for 5–7 days is inferior to
Metronidazole or Tinidazole.
● Intestinal infections: Bacterial Enteritis
● Food poisoning diarrhoeas, Bacillary Dysentery
● Trichomonad colpitis
Furazolidone is partly absorbed from intestines and excreted in urine which turns orange – patients should be told about it.
It is used orally, intravaginally and rectally.
Adverse effects are mild and infrequent – nausea, headache, dizziness.
Слайд 22
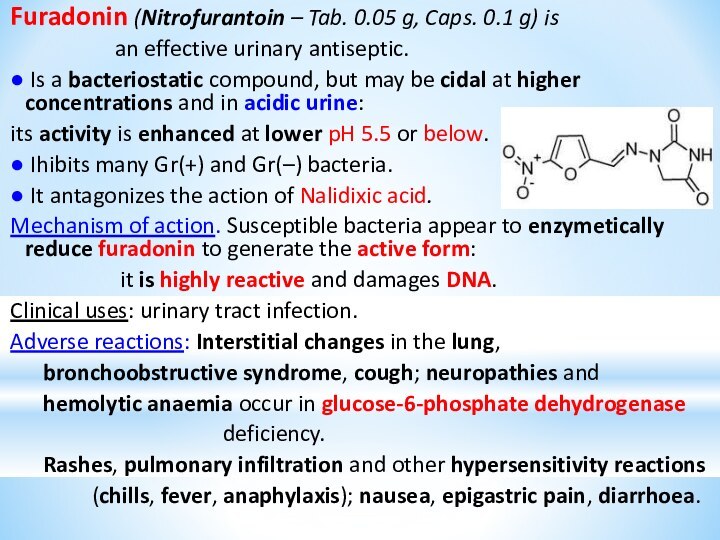
Furadonin (Nitrofurantoin – Tab. 0.05 g, Caps. 0.1
g) is
an effective urinary antiseptic.
● Is a bacteriostatic
compound, but may be cidal at higher concentrations and in acidic urine:
its activity is enhanced at lower pH 5.5 or below.
● Ihibits many Gr(+) and Gr(–) bacteria.
● It antagonizes the action of Nalidixic acid.
Mechanism of action. Susceptible bacteria appear to enzymetically reduce furadonin to generate the active form:
it is highly reactive and damages DNA.
Clinical uses: urinary tract infection.
Adverse reactions: Interstitial changes in the lung,
bronchoobstructive syndrome, cough; neuropathies and
hemolytic anaemia occur in glucose-6-phosphate dehydrogenase
deficiency.
Rashes, pulmonary infiltration and other hypersensitivity reactions
(chills, fever, anaphylaxis); nausea, epigastric pain, diarrhoea.
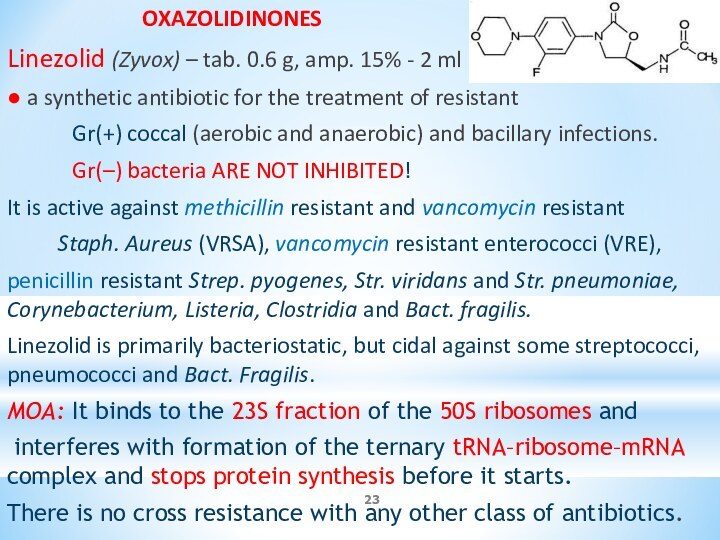
OXAZOLIDINONES
Linezolid (Zyvox) – tab.
0.6 g, amp. 15% - 2 ml
● a synthetic antibiotic for the treatment of resistant
Gr(+) coccal (aerobic and anaerobic) and bacillary infections.
Gr(–) bacteria ARE NOT INHIBITED!
It is active against methicillin resistant and vancomycin resistant
Staph. Aureus (VRSA), vancomycin resistant enterococci (VRE),
penicillin resistant Strep. pyogenes, Str. viridans and Str. pneumoniae, Corynebacterium, Listeria, Clostridia and Bact. fragilis.
Linezolid is primarily bacteriostatic, but cidal against some streptococci, pneumococci and Bact. Fragilis.
MOA: It binds to the 23S fraction of the 50S ribosomes and
interferes with formation of the ternary tRNA–ribosome–mRNA complex and stops protein synthesis before it starts.
There is no cross resistance with any other class of antibiotics.
Слайд 24
ANTIFUNGAL DRUGS
I. For the treatment of mycoses caused
by Pathogenic Fungi:
1. For subcutaneous and systemic mycoses:
Antibiotics:
Amphotericin B
Mycoheptin
Azole derivatives:
∙ Imidazoles: Ketoconazole, Miconazole
∙ Triazoles: Itraconazole, Fluconazole
Слайд 25
2. Drugs for Superficial Fungal Infections:
Antibiotics: Griseofulvin
Methylnaftaline derivative:
Terbinafine (Lamizyl – Tab. 0.25 g; 1% cream)
Imidazole
derivatives:
Miconazole
Clotrimazole (1% cream, Tab. vaginal 0.1 g)
Nitrophenol derivatives:
Nitrofungin
Iodine preparations:
Iodide alcohol solution
Potassium iodide solution
Слайд 26
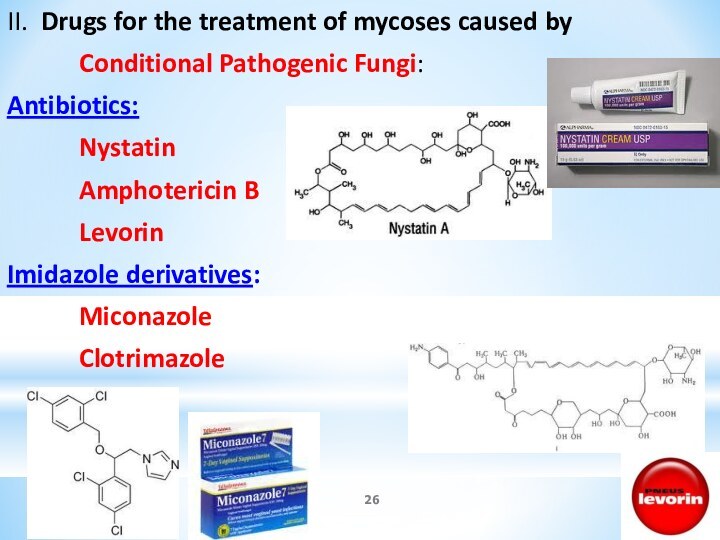
II. Drugs for the treatment of mycoses caused
by
Conditional Pathogenic Fungi:
Antibiotics:
Nystatin
Amphotericin B
Levorin
Imidazole derivatives:
Miconazole
Clotrimazole
Слайд 27
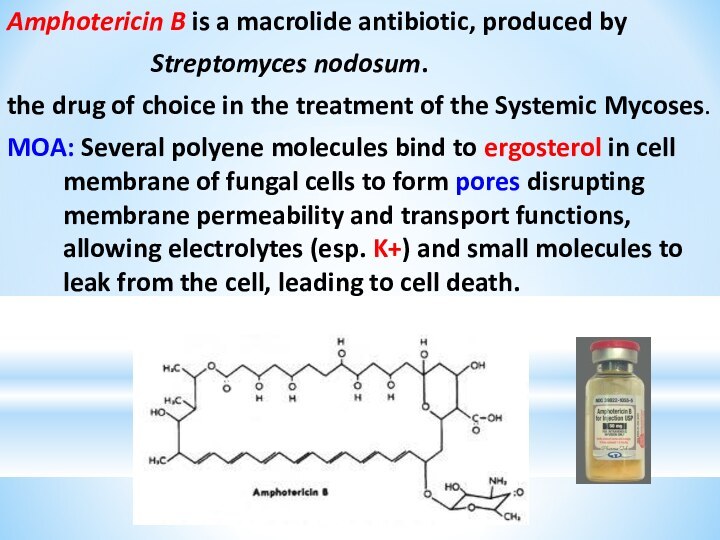
Amphotericin B is a macrolide antibiotic, produced by
Streptomyces nodosum.
the drug of choice in the treatment of
the Systemic Mycoses.
MOA: Several polyene molecules bind to ergosterol in cell membrane of fungal cells to form pores disrupting membrane permeability and transport functions, allowing electrolytes (esp. K+) and small molecules to leak from the cell, leading to cell death.
Слайд 28
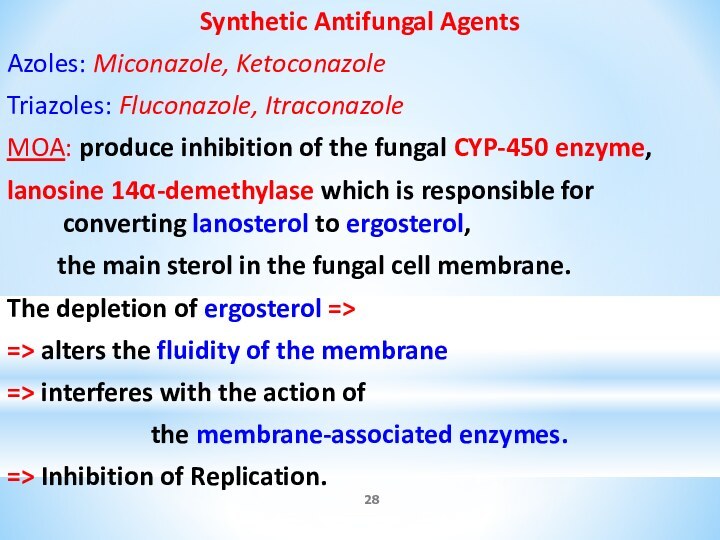
Synthetic Antifungal Agents
Azoles: Miconazole, Ketoconazole
Triazoles: Fluconazole,
Itraconazole
MOA: produce inhibition of the fungal CYP-450 enzyme,
lanosine 14α-demethylase which is responsible for converting lanosterol to ergosterol,
the main sterol in the fungal cell membrane.
The depletion of ergosterol =>
=> alters the fluidity of the membrane
=> interferes with the action of
the membrane-associated enzymes.
=> Inhibition of Replication.
Слайд 29
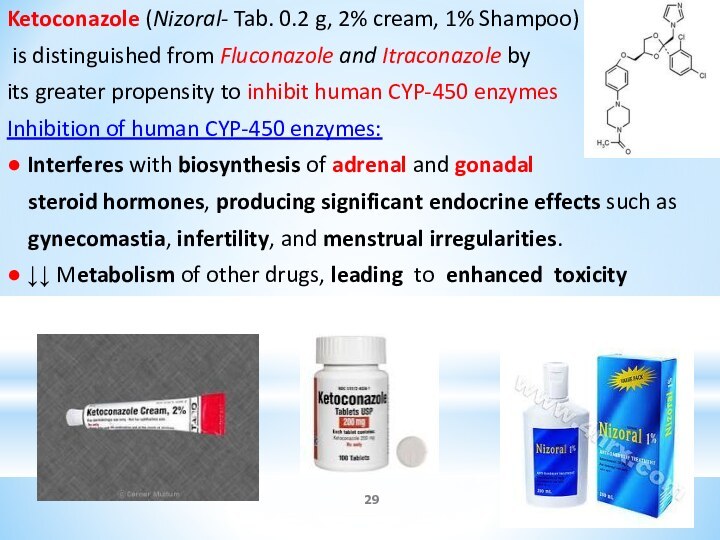
Ketoconazole (Nizoral- Tab. 0.2 g, 2% cream, 1%
Shampoo)
is distinguished from Fluconazole and Itraconazole by
its
greater propensity to inhibit human CYP-450 enzymes
Inhibition of human CYP-450 enzymes:
● Interferes with biosynthesis of adrenal and gonadal
steroid hormones, producing significant endocrine effects such as
gynecomastia, infertility, and menstrual irregularities.
● ↓↓ Metabolism of other drugs, leading to enhanced toxicity
Слайд 30
Clotrimazole – only for local administration
1% cream, lotion;
Tab. vaginal 0.1 g –
a synthetic imidazole derivative
for dermatophytic infections,
including Tinea corporis, Tinea pedis, Tinea cruris;
Vulvovaginal and Oropharyngeal Candidiasis, Keratitis.
MOA: by binding with phospholipids in the fungal cell membrane,
alters cell membrane permeability
It inhibits or kills many fungi, including yeast and dermatophytes, and also is acting against some Gr(+) bacteria.
Pharmacokinetics: Absorption is negligible and adverse effects are rare.
Слайд 31
Terbinafine (Lamizil – Tab 0.25 g; 1% cream)
-
Methylnaftaline derivative for
Superficial Fungal Infections –
a
highly lipophilic keratophilic fungicidal compound
● Inhibits the enzyme squalene epoxidase, which is involved in
the synthesis of ergosterol from squalene in the fungal cell wall.
The accumulation of squalene within the cell is toxic to the organism.
● Given orally, it is rapidly absorbed and is taken up by skin, nails and
adipose tissue.
● Given topically, it penetrates skin and mucous membranes.
● 1 tab. PO for 12 weeks achieves a cure rate of up to 90% for
onychomycosis (ringworm of nails)
Unwanted effects: GIT upsets, rashes, pruritus,
joint and muscle pains,
hepatitis.