Слайд 2
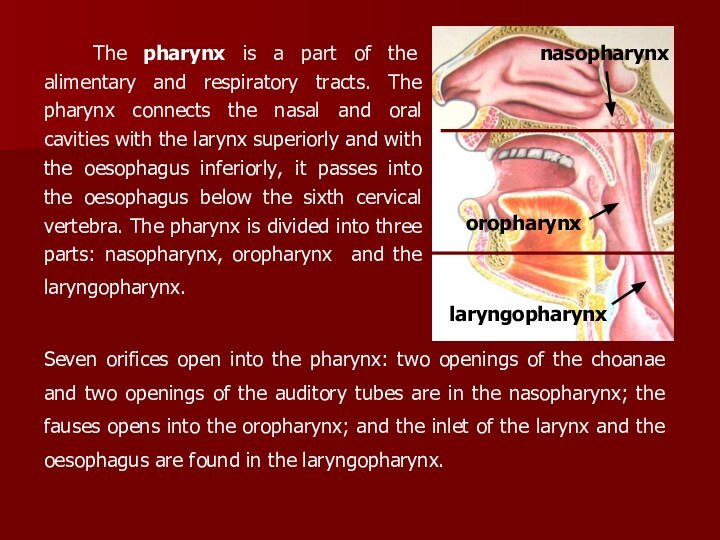
The pharynx is a part of the alimentary
and respiratory tracts. The pharynx connects the nasal and
oral cavities with the larynx superiorly and with the oesophagus inferiorly, it passes into the oesophagus below the sixth cervical vertebra. The pharynx is divided into three parts: nasopharynx, oropharynx and the laryngopharynx.
nasopharynx
oropharynx
laryngopharynx
Seven orifices open into the pharynx: two openings of the choanae and two openings of the auditory tubes are in the nasopharynx; the fauses opens into the oropharynx; and the inlet of the larynx and the oesophagus are found in the laryngopharynx.
Слайд 3
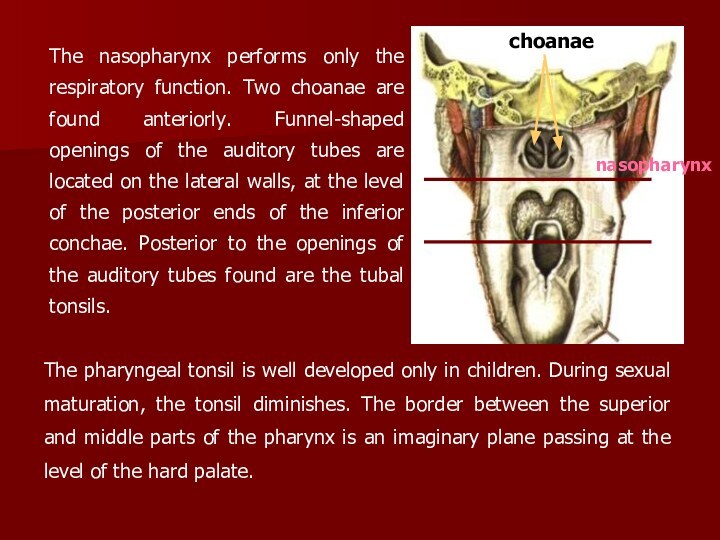
The nasopharynx performs only the respiratory function. Two
choanae are found anteriorly. Funnel-shaped openings of the auditory
tubes are located on the lateral walls, at the level of the posterior ends of the inferior conchae. Posterior to the openings of the auditory tubes found are the tubal tonsils.
The pharyngeal tonsil is well developed only in children. During sexual maturation, the tonsil diminishes. The border between the superior and middle parts of the pharynx is an imaginary plane passing at the level of the hard palate.
nasopharynx
Слайд 4
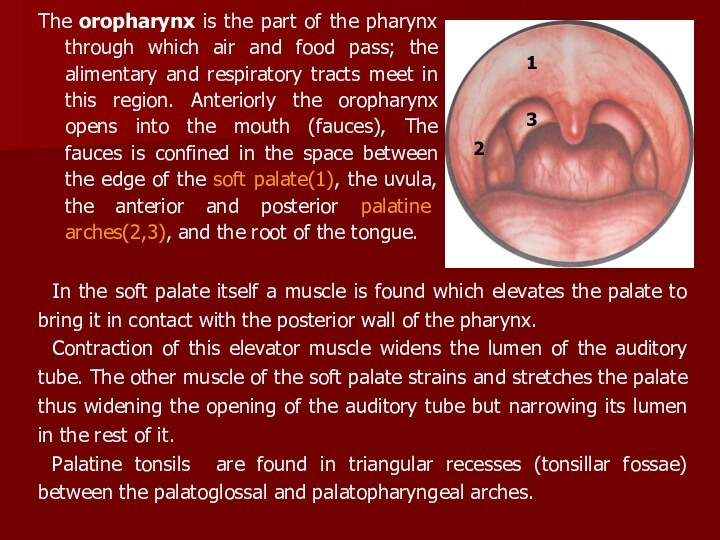
The oropharynx is the part of the pharynx
through which air and food pass; the alimentary and
respiratory tracts meet in this region. Anteriorly the oropharynx opens into the mouth (fauces), The fauces is confined in the space between the edge of the soft palate(1), the uvulа, the anterior and posterior palatine arches(2,3), and the root of the tongue.
In the soft palate itself a muscle is found which elevates the palate to bring it in contact with the posterior wall of the pharynx.
Contraction of this elevator muscle widens the lumen of the auditory tube. The other muscle of the soft palate strains and stretches the palate thus widening the opening of the auditory tube but narrowing its lumen in the rest of it.
Palatine tonsils are found in triangular recesses (tonsillar fossae) between the palatoglossal and palatopharyngeal arches.
Слайд 5
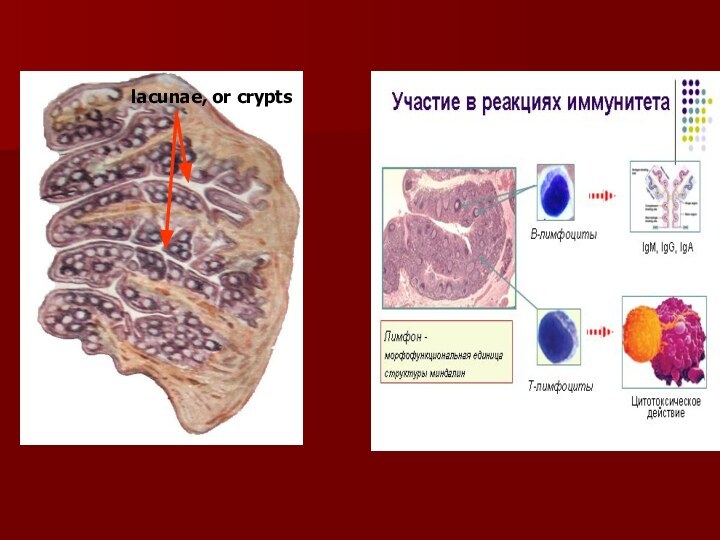
The histological structure of the lymphoid tissue of
the pharynx is uniform: a mass of lymphocytes with
spheric formations known as follicles is located between connective-tissue fibres. The structure of the palatine tonsils is important from the clinical standpoint. Their free surface is exposed to the pharyngeal cavity and is lined with mucous membrane with stratified squamous epithelium. The tonsil has 16-18 deep pits known as lacunae, or crypts. The total summ of the surface area of the crypt is about 300sm2.
The outer surface of the tonsils is connected with the lateral wall of tht pharynx by a firm fibrous membrane called the capsule. The lacunae penetrate into the depth of the tonsil where they ramify.
Слайд 6
Located underneath the epithelium of the crypt are
diffuse lymphoid tissues and groups of follicles, which are
differentiated into: a) so called primary follicles, which are made up only of lymphocytes; b) bigger sized secondary follicles with an germinal centre, surrounded by lymphocytes.
The basic cell element of the tonsil is the lymphocyte. T-lymphocytes (about 25%) appear in the palatine tonsils only after the formation of the thymus. They are mostly represented by T-helpers and T-suppressors. A small number of T-helpers located in the secondary follicle. In addition the tonsils also have plasmatic cells, the so called normal killers; immunoglobuline synthesizing cells of the classes G, A, M, U, D, small lymphocytes with a relatively massive nucleus – the carrier of encoded information. These are the so called memory cells.
Слайд 8
In the defense function of the tonsils an
important role is played by the synthesis of a
factor of local immunity of mucous membranes IgA,; produce a powerful factor of nonspecific immunity, mainly antiviral defense – interferons, and also the lysosomes.
The structure of the palatine tonsils foresees the continuous prolonged contact of the antigens with the lymphoid cells which migrate into the lacunar lumen; a more intense migration of lymphocytes takes place in regions where the connective tissue is absent.
This contact in itself helps the lymphoid cells in obtaining antigenic information. With the formation of clone cells in tonsils tissues which are specific in relation to the given antigen.
Слайд 9
The former assure the informative function of the
tonsil tissue, carried out by the smaller lymphocytes (memory
cells), who are capable of giving out a fast secondary immunological answer.
This function enables the sustainment of the normal mictoflora.
In such a manner, the tonsils, mainly, are responsible for carrying out 3 biologically important functions:
defensive, informative and sustenance of the bacteriological homeostasis.
The lingual tonsil (IV) is located on the root of the tongue.. All these tonsils are called the throat ring (Pirogov-Waldeyer tonsillar ring).
Слайд 10
The laryngopharynx. The superior edge of the epiglottis
and the root of the tongue form the border
between the oropharynx and the laryngopharynx. The lower end of the laryngopharynx narrows into a funnel and is continuous with the oesophagus. Along the sides of the entrance to the larynx, between the entrance and the lateral walls of the pharynx, are found the piriform recesses. Food moves to the oesophagus by these piriform recesses. The pharyngeal wall consists of four layers. The main layer is a fibrous membrane, which is lined with mucosa on the inside, and with muscles on the outside.
Слайд 11
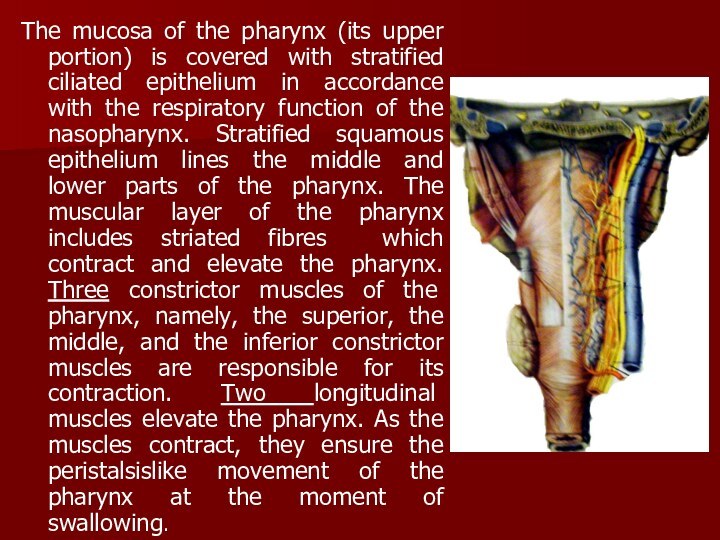
The mucosa of the pharynx (its upper portion)
is covered with stratified ciliated epithelium in accordance with
the respiratory function of the nasopharynx. Stratified squamous epithelium lines the middle and lower parts of the pharynx. The muscular layer of the pharynx includes striated fibres which contract and elevate the pharynx. Three constrictor muscles of the pharynx, namely, the superior, the middle, and the inferior constrictor muscles are responsible for its contraction. Two longitudinal muscles elevate the pharynx. As the muscles contract, they ensure the peristalsislike movement of the pharynx at the moment of swallowing.
Слайд 12
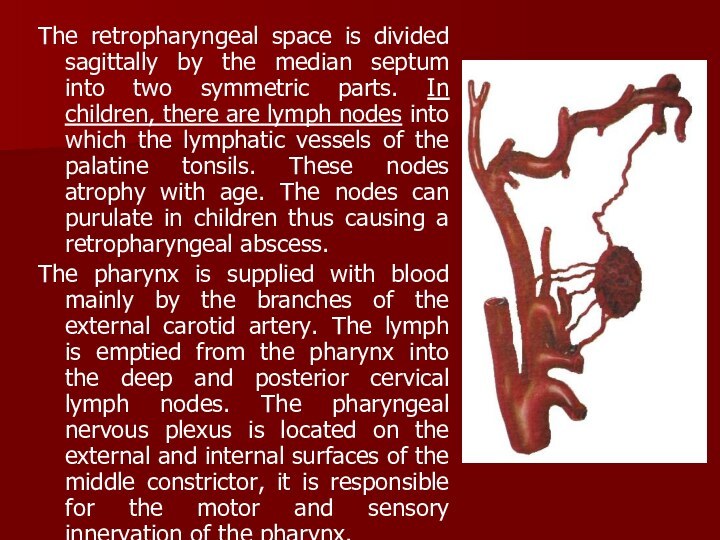
The retropharyngeal space is divided sagittally by the
median septum into two symmetric parts. In children, there
are lymph nodes into which the lymphatic vessels of the palatine tonsils. These nodes atrophy with age. The nodes can purulate in children thus causing a retropharyngeal abscess.
The pharynx is supplied with blood mainly by the branches of the external carotid artery. The lymph is emptied from the pharynx into the deep and posterior cervical lymph nodes. The pharyngeal nervous plexus is located on the external and internal surfaces of the middle constrictor, it is responsible for the motor and sensory innervation of the pharynx.
Слайд 13
CLINICAL PHYSIOLOGY OF THE PHARYNX. The pharynx is
involved in the following vital functions: (1) ingestion of
food (sucking and swallowing); (2) production of vocal sounds; (3) respiration; (4) protective function (during eating and respiration).
Ingestion of food during the first months of life can only be accomplished by sucking. The passage of food by the pharynx, from the mouth into the oesophagus, is accomplished by a complicated and well coordinated swallowing reflex. The muscles of the tongue, pharynx and the larynx contract in a specific sequence.
The vocal function of the pharynx includes intensification of sounds produced in the larynx by resonance.
Слайд 14
All parts of the pharynx are involved in
the respiratory function. But if the nasal passages are
obstructed, breathing is accomplished through the mouth.
The protective function of the pharynx consists in reflex contraction of the pharyngeal muscles when a foreign body or an irritating substance.
Inspired air is first warmed in the nose and then in the pharynx, where it is also cleaned from dust which sticks to the mucous lining of the pharyngeal walls. The physiology of the palatine tonsils is not autonomous. It is part of the function of the entire lymphatic system of the body. During the first years of life, the lymphoid structures of the pharynx attain maximum growth, but during sexual maturation (at the age of 14-15) they undergo partial and gradual back development.
Слайд 15
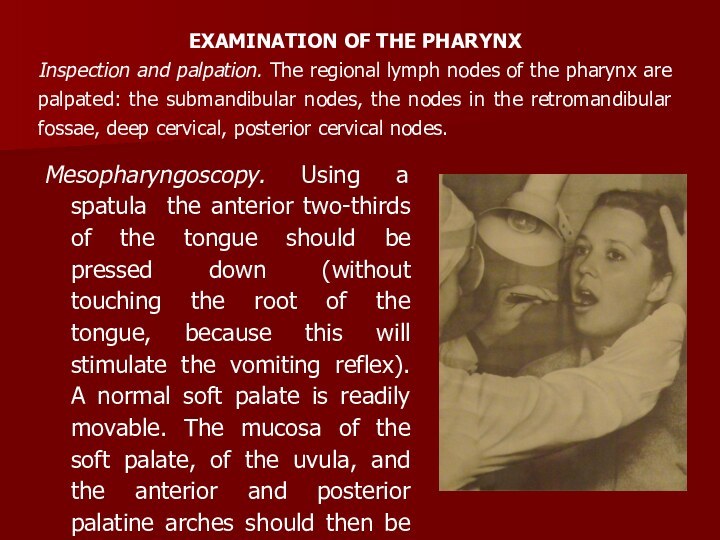
Mesopharyngoscopy. Using a spatula the anterior two-thirds of
the tongue should be pressed down (without touching the
root of the tongue, because this will stimulate the vomiting reflex). A normal soft palate is readily movable. The mucosa of the soft palate, of the uvula, and the anterior and posterior palatine arches should then be inspected.
EXAMINATION OF THE PHARYNX
Inspection and palpation. The regional lymph nodes of the pharynx are palpated: the submandibular nodes, the nodes in the retromandibular fossae, deep cervical, posterior cervical nodes.
Слайд 16
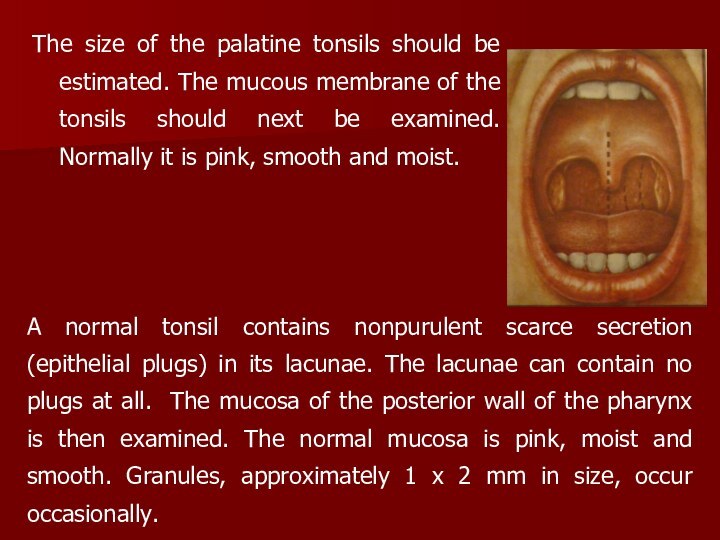
The size of the palatine tonsils should be
estimated. The mucous membrane of the tonsils should next
be examined. Normally it is pink, smooth and moist.
A normal tonsil contains nonpurulent scarce secretion (epithelial plugs) in its lacunae. The lacunae can contain no plugs at all. The mucosa of the posterior wall of the pharynx is then examined. The normal mucosa is pink, moist and smooth. Granules, approximately 1 x 2 mm in size, occur occasionally.
Слайд 17
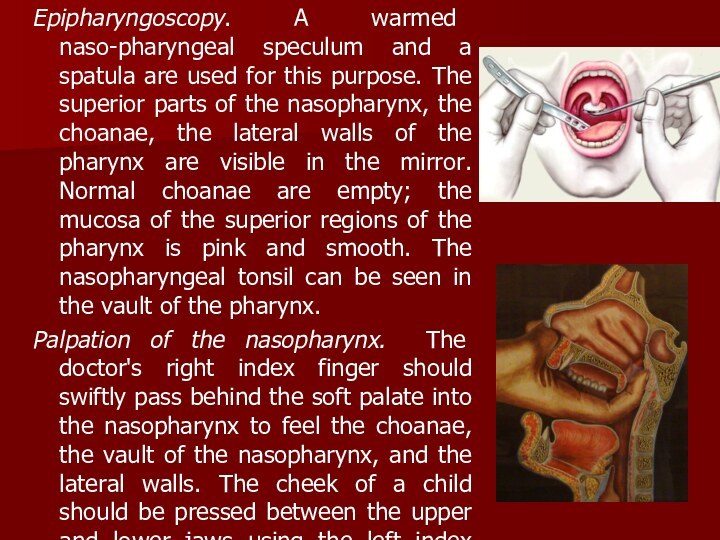
Epipharyngoscopy. A warmed naso-pharyngeal speculum and a spatula
are used for this purpose. The superior parts of
the nasopharynx, the choanae, the lateral walls of the pharynx are visible in the mirror. Normal choanae are empty; the mucosa of the superior regions of the pharynx is pink and smooth. The nasopharyngeal tonsil can be seen in the vault of the pharynx.
Palpation of the nasopharynx. The doctor's right index finger should swiftly pass behind the soft palate into the nasopharynx to feel the choanae, the vault of the nasopharynx, and the lateral walls. The cheek of a child should be pressed between the upper and lower jaws using the left index finger.
Слайд 18
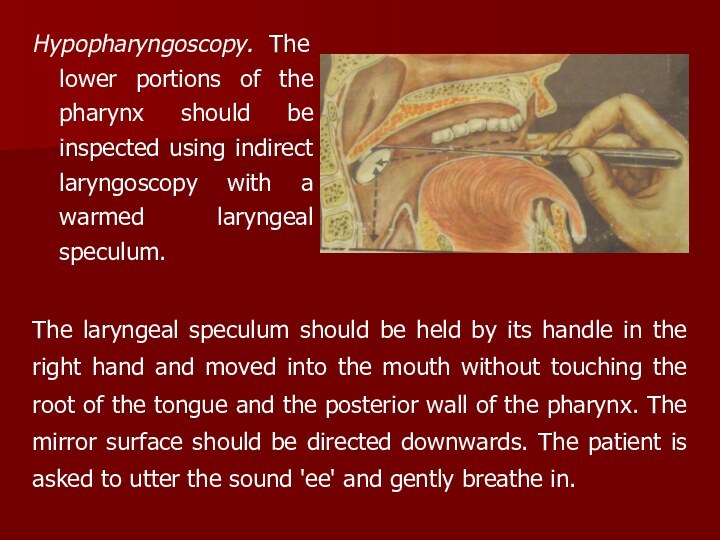
Hypopharyngoscopy. The lower portions of the pharynx should
be inspected using indirect laryngoscopy with a warmed laryngeal
speculum.
The laryngeal speculum should be held by its handle in the right hand and moved into the mouth without touching the root of the tongue and the posterior wall of the pharynx. The mirror surface should be directed downwards. The patient is asked to utter the sound 'ee' and gently breathe in.
Слайд 19
INFLAMMATION OF THE TONSILS
Acute tonsillitis is a general
infectious disease in which the lymphoid tissue of the
tonsils is affected by inflammation.
Aetiology and pathogenesis. Among many microbes that can provoke acute tonsillitis the leading aetiological role belongs to beta-haemolytic streptococcus of group A.
The exogenic factor attacks the tonsillar mucosa via airborne and alimentary route, and also by direct contact. Three main forms of the development of common acute tonsillitis are distinguished: (1) ocassional acute tonsillitis manifested as autoinfection due to impaired environmental conditions, often as a result of chilling; (2) epidemic form arising as a result of infection from a tonsillitis patient; (3) exacerbation of chronic tonsillitis.
The commonly used classification includes the following forms: I-catarrhal; II-follicular; III-lacunar; IV-necrotic.
Слайд 20
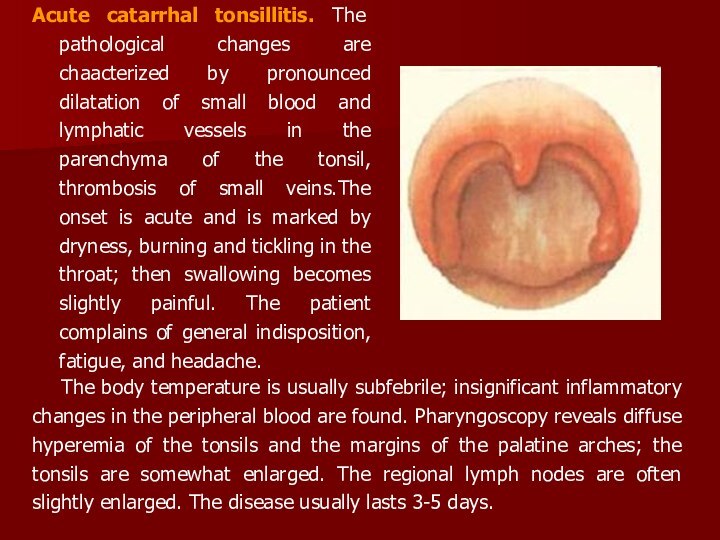
Acute catarrhal tonsillitis. The pathological changes are chaacterized
by pronounced dilatation of small blood and lymphatic vessels
in the parenchyma of the tonsil, thrombosis of small veins.The onset is acute and is marked by dryness, burning and tickling in the throat; then swallowing becomes slightly painful. The patient complains of general indisposition, fatigue, and headache.
The body temperature is usually subfebrile; insignificant inflammatory changes in the peripheral blood are found. Pharyngoscopy reveals diffuse hyperemia of the tonsils and the margins of the palatine arches; the tonsils are somewhat enlarged. The regional lymph nodes are often slightly enlarged. The disease usually lasts 3-5 days.
Слайд 21
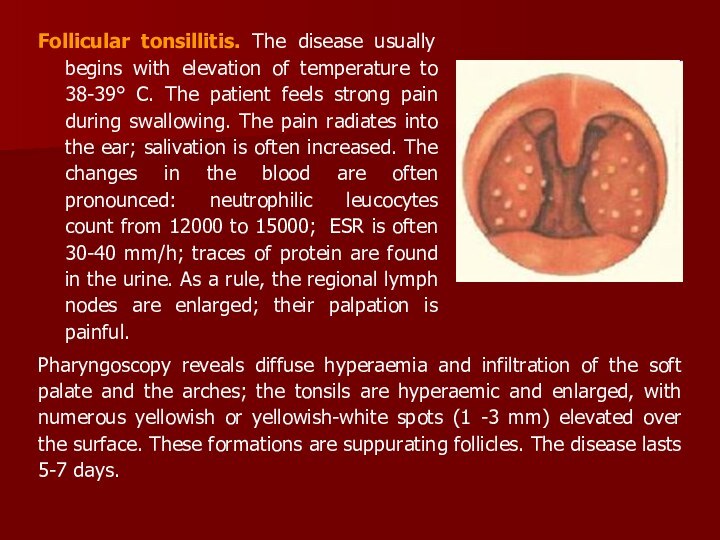
Follicular tonsillitis. The disease usually begins with elevation
of temperature to 38-39° C. The patient feels strong
pain during swallowing. The pain radiates into the ear; salivation is often increased. The changes in the blood are often pronounced: neutrophilic leucocytes count from 12000 to 15000; ESR is often 30-40 mm/h; traces of protein are found in the urine. As a rule, the regional lymph nodes are enlarged; their palpation is painful.
Pharyngoscopy reveals diffuse hyperaemia and infiltration of the soft palate and the arches; the tonsils are hyperaemic and enlarged, with numerous yellowish or yellowish-white spots (1 -3 mm) elevated over the surface. These formations are suppurating follicles. The disease lasts 5-7 days.
Слайд 22
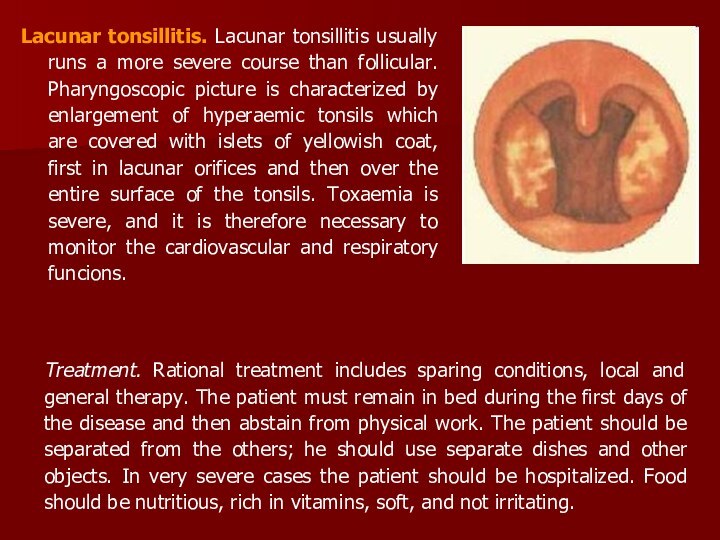
Lacunar tonsillitis. Lacunar tonsillitis usually runs a more
severe course than follicular. Pharyngoscopic picture is characterized by
enlargement of hyperaemic tonsils which are covered with islets of yellowish coat, first in lacunar orifices and then over the entire surface of the tonsils. Toxaemia is severe, and it is therefore necessary to monitor the cardiovascular and respiratory funcions.
Treatment. Rational treatment includes sparing conditions, local and general therapy. The patient must remain in bed during the first days of the disease and then abstain from physical work. The patient should be separated from the others; he should use separate dishes and other objects. In very severe cases the patient should be hospitalized. Food should be nutritious, rich in vitamins, soft, and not irritating.
Слайд 23
Treatment includes also gargling with a warm solution
of hydrocarbonate, furacilin. A warming compress should be applied
to the neck. Salicylates and antibacterial preparations should be used for general treatment.
The choice of antibacterial preparations depends on the gravity of the disease and the danger of complications. The antibiotic is administered usually for 5 days, which is, as a rule, sufficient to normalize body temperature and to improve the patient's condition. In order to eliminate reliably the infectious focus, it is necessary to continue the antibiotic therapy (amoxil 0,5 or amoxiclav 0,625) for another 5-7 days. Desensitizing preparations such as loratadin, ksisal etc. are recommended.
Слайд 24
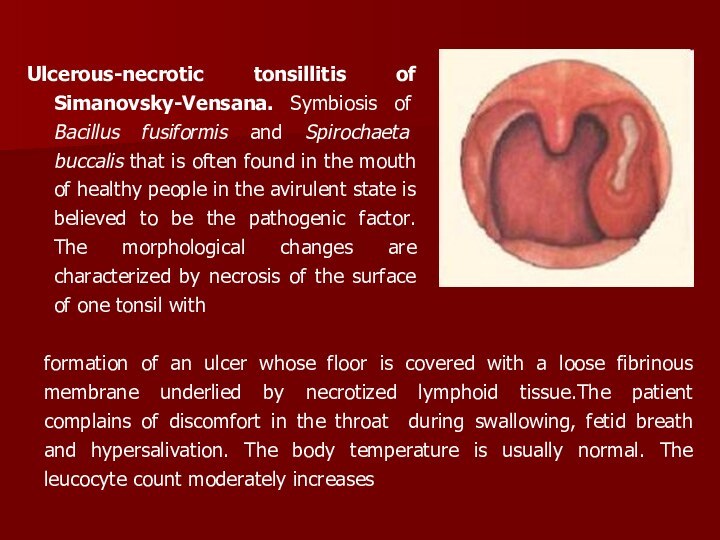
Ulcerous-necrotic tonsillitis of Simanovsky-Vensana. Symbiosis of Bacillus fusiformis
and Spirochaeta buccalis that is often found in the
mouth of healthy people in the avirulent state is believed to be the pathogenic factor. The morphological changes are characterized by necrosis of the surface of one tonsil with
formation of an ulcer whose floor is covered with a loose fibrinous membrane underlied by necrotized lymphoid tissue.The patient complains of discomfort in the throat during swallowing, fetid breath and hypersalivation. The body temperature is usually normal. The leucocyte count moderately increases
Слайд 25
The regional lymph nodes are enlarged on the
involved side; they are moderately painful to palpation. Swallowing
is usually painless. The disease lasts 1 to 3 weeks but can in some cases persist for several months.
Treatment consists in tending the mouth cavity, cleaning the ulcers from necrotized matter, gargling with disinfectant solutions. The surface of the ulcer is treated with an iodine
tincture, silver nitrate or other solution.
Antibiotic therapy (amoxiclav 0,625) for another 5-7 days.
Слайд 26
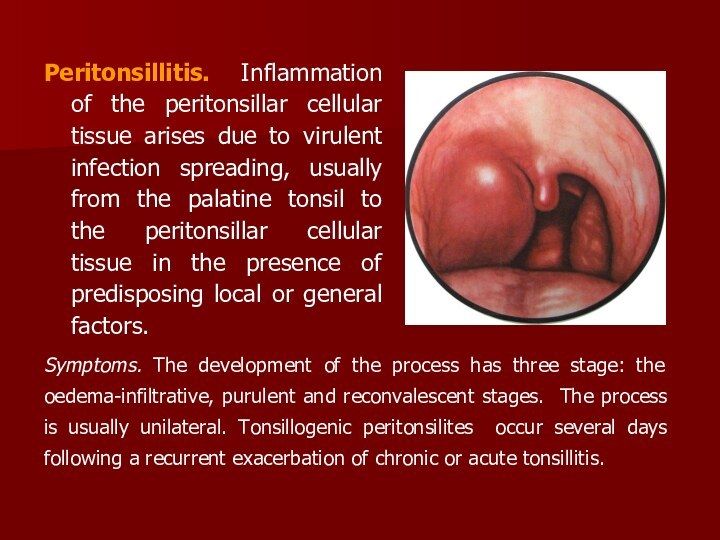
Peritonsillitis. Inflammation of the peritonsillar cellular tissue arises
due to virulent infection spreading, usually from the palatine
tonsil to the peritonsillar cellular tissue in the presence of predisposing local or general factors.
Symptoms. The development of the process has three stage: the oedema-infiltrative, purulent and reconvalescent stages. The process is usually unilateral. Tonsillogenic peritonsilites occur several days following a recurrent exacerbation of chronic or acute tonsillitis.
Слайд 27
A peritonsillar abscess can be found in the
antero-superior part, between the tonsillar capsule and the upper
part of the anterior palatine arch. The supratonsillar location of the abscess is most common. Posterior peritonsillitis (developing between the tonsil and the posterior arch) may cause oedema of the larynx. Peritonsillitis can also be inferior, with location of the focus between the inferior pole of the tonsil and the lateral pharyngeal wall, or lateral, occurring between the middle portion of the tonsil and the lateral wall of the pharynx. Lateral abscess runs the most severe course because of difficult spontaneous drainage.
The onset of the disease is manifested by severe pain during swallowing. The patient complains of headache and fatigue; the body temperature rises to febrile. Spontaneous pain in the throat becomes more intense, it radiates into the ear, teeth, and becomes so intense during swallowing that the patient refuses food and drinks. Trismus of the masticatory muscles develops. The speech becomes nasal and slurred.
Слайд 28
Inflammation of the pharyngeal muscles and also cervical
lymphadenitis cause pain as the patient moves his head
to one side. The leucocyte counts are 10-15 x 109 per 1; the blood count is shifted to the left; the erythrocyte sedimentation rate increases. Pharyngoscopy is difficult due to trismus: the mouth usually would open not wider than 2-3 cm. Anterosuperior peritonsillites are characterized by marked protrusion of the upper pole of the tonsil together with the palatine arches and the soft palate toward the median line. Half of the soft palate, together with the superior tonsillar pole and the upper part of the arches form a sphere whose surface is tense and hyperaemic; the uvula is moved to the opposite side, the tonsil is displaced posteriorly and inferiorly. The tongue is covered with a thick coat, the saliva is tenacious. Fluctuation is observed in the region of the strongest protrusion; the abscess opens at this point, often through the supratonsillar recess or the anterior arch.
Слайд 29
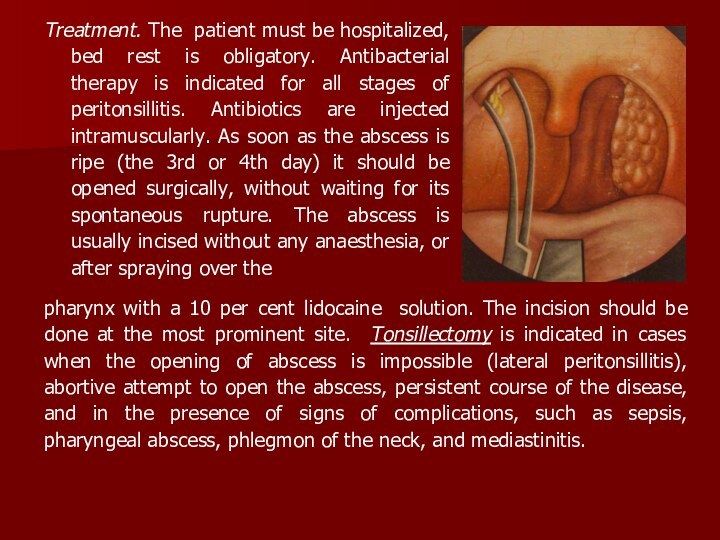
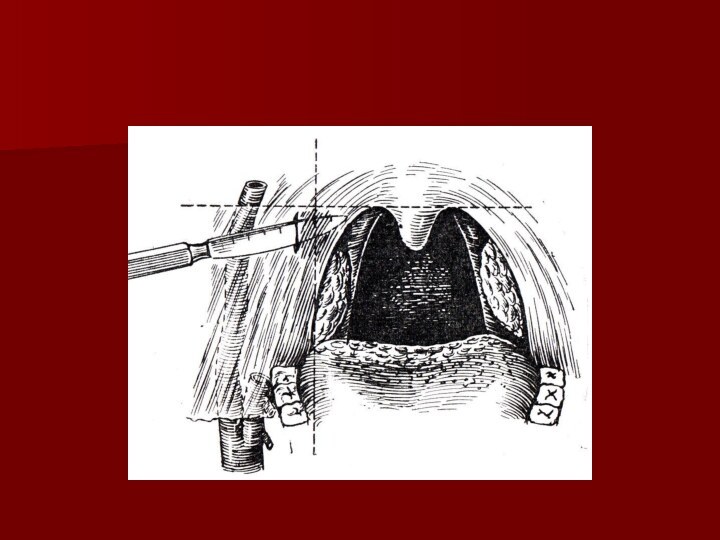
Treatment. The patient must be hospitalized, bed rest
is obligatory. Antibacterial therapy is indicated for all stages
of peritonsillitis. Antibiotics are injected intramuscularly. As soon as the abscess is ripe (the 3rd or 4th day) it should be opened surgically, without waiting for its spontaneous rupture. The abscess is usually incised without any anaesthesia, or after spraying over the
pharynx with a 10 per cent lidocaine solution. The incision should be done at the most prominent site. Tonsillectomy is indicated in cases when the opening of abscess is impossible (lateral peritonsillitis), abortive attempt to open the abscess, persistent course of the disease, and in the presence of signs of complications, such as sepsis, pharyngeal abscess, phlegmon of the neck, and mediastinitis.
Слайд 31
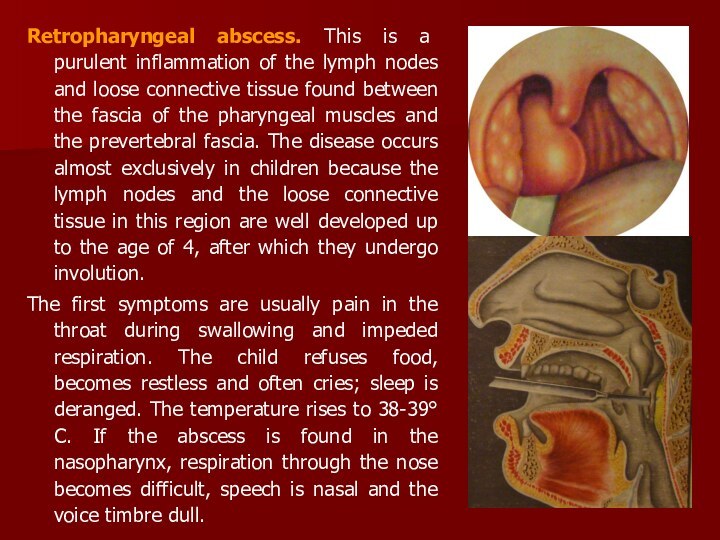
Retropharyngeal abscess. This is a purulent inflammation of
the lymph nodes and loose connective tissue found between
the fascia of the pharyngeal muscles and the prevertebral fascia. The disease occurs almost exclusively in children because the lymph nodes and the loose connective tissue in this region are well developed up to the age of 4, after which they undergo involution.
The first symptoms are usually pain in the throat during swallowing and impeded respiration. The child refuses food, becomes restless and often cries; sleep is deranged. The temperature rises to 38-39° C. If the abscess is found in the nasopharynx, respiration through the nose becomes difficult, speech is nasal and the voice timbre dull.
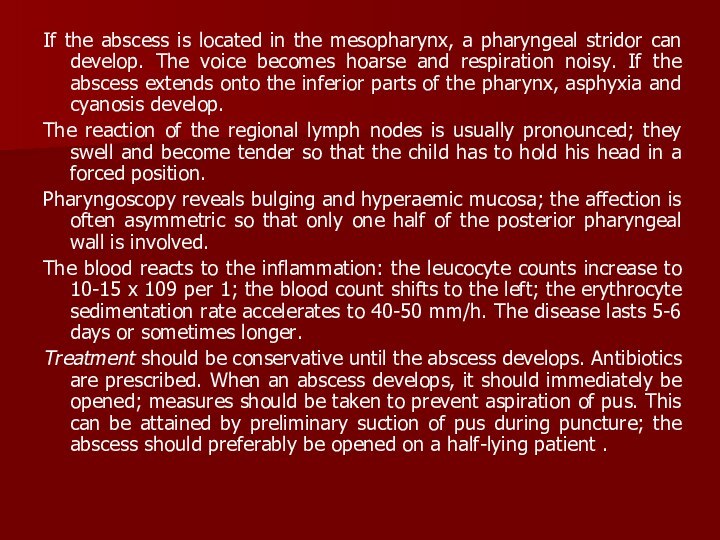
Слайд 32
If the abscess is located in the mesopharynx,
a pharyngeal stridor can develop. The voice becomes hoarse
and respiration noisy. If the abscess extends onto the inferior parts of the pharynx, asphyxia and cyanosis develop.
The reaction of the regional lymph nodes is usually pronounced; they swell and become tender so that the child has to hold his head in a forced position.
Pharyngoscopy reveals bulging and hyperaemic mucosa; the affection is often asymmetric so that only one half of the posterior pharyngeal wall is involved.
The blood reacts to the inflammation: the leucocyte counts increase to 10-15 x 109 per 1; the blood count shifts to the left; the erythrocyte sedimentation rate accelerates to 40-50 mm/h. The disease lasts 5-6 days or sometimes longer.
Treatment should be conservative until the abscess develops. Antibiotics are prescribed. When an abscess develops, it should immediately be opened; measures should be taken to prevent aspiration of pus. This can be attained by preliminary suction of pus during puncture; the abscess should preferably be opened on a half-lying patient .
Слайд 33
AFFECTIONS OF THE PHARYNX IN SYSTEMIC DISEASES
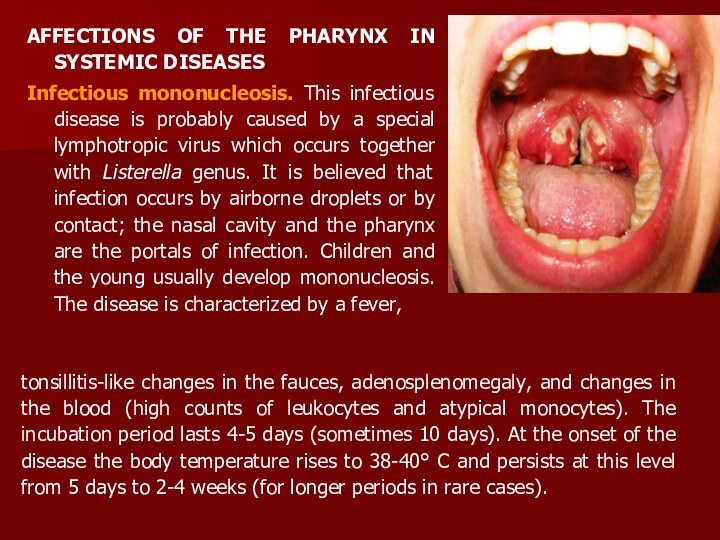
Infectious
mononucleosis. This infectious disease is probably caused by a
special lymphotropic virus which occurs together with Listerella genus. It is believed that infection occurs by airborne droplets or by contact; the nasal cavity and the pharynx are the portals of infection. Children and the young usually develop mononucleosis. The disease is characterized by a fever,
tonsillitis-like changes in the fauces, adenosplenomegaly, and changes in the blood (high counts of leukocytes and atypical monocytes). The incubation period lasts 4-5 days (sometimes 10 days). At the onset of the disease the body temperature rises to 38-40° C and persists at this level from 5 days to 2-4 weeks (for longer periods in rare cases).
Слайд 34
The symptoms are sometimes alleviated periodically during this
stage. An early and permanent sign of the disease
is enlarged lymph nodes, first on the neck and then in the groin, armpits, and the abdomen. The spleen and the liver are also enlarged in most patients. Changes in the fauces usually follow the enlargement of the lymph nodes; they are similar to those occurring in catarrhal, lacunar, fibrinous, and less frequently necrotic tonsillitis.
The most characteristic symptom of the disease is a moderate leucocytosis with a predominance of mononuclear cells, which may number 50 to 90 per cent of the total leukocytes, a great number of altered monocytes .
Treatment. Bed rest and high-calorie diet rich in vitamins are prescribed. Antibacterial preparations prevent secondary infection; the causative agent is insensitive to them. Gargling with disinfectant or astringent solutions is useful. Necrotized areas are treated with a 10 per cent silver nitrate solution.
Слайд 35
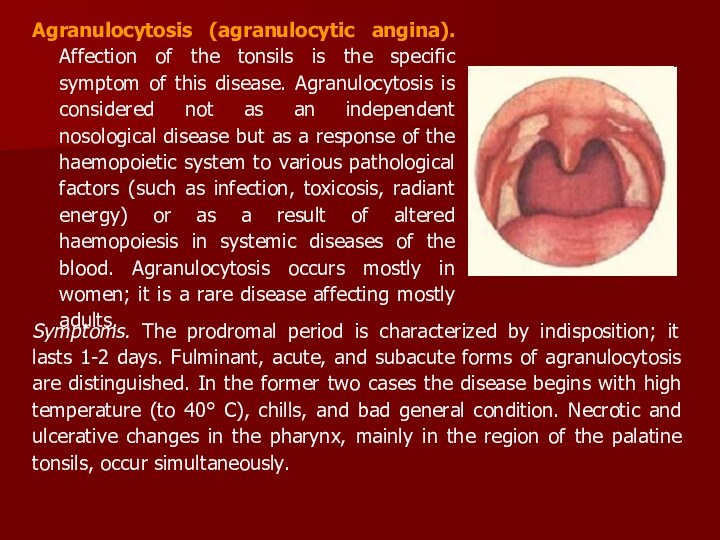
Agranulocytosis (agranulocytic angina). Affection of the tonsils is
the specific symptom of this disease. Agranulocytosis is considered
not as an independent nosological disease but as a response of the haemopoietic system to various pathological factors (such as infection, toxicosis, radiant energy) or as a result of altered haemopoiesis in systemic diseases of the blood. Agranulocytosis occurs mostly in women; it is a rare disease affecting mostly adults.
Symptoms. The prodromal period is characterized by indisposition; it lasts 1-2 days. Fulminant, acute, and subacute forms of agranulocytosis are distinguished. In the former two cases the disease begins with high temperature (to 40° C), chills, and bad general condition. Necrotic and ulcerative changes in the pharynx, mainly in the region of the palatine tonsils, occur simultaneously.
Слайд 36
Necrosis often spreads onto the mucous of the
pharynx, gums, and the larynx. In rare cases, the
destructive changes occur in the intestine and the urinary bladder. Necrosis can extend onto deep underlying soft tissues and bones.
The blood is characterized by a very low count of polymorphonuclear leukocytes, or they can be absent.
Treatment is aimed at activizing the haemopoietic system and controlling secondary infection. Exeption of all medicines that can cause agranulocytosis (amidopyrine, sulphanilamide, salvarsan, etc.). Blood transfusion, antibioticotherapy, hormone preparations and other means of treating agranulocytosis are prescribed. The diet should be sparing; the patient must gargle the throat with antiseptic solutions; the necrotized matter should be removed.
Слайд 37
CHRONIC TONSILLITIS
Chronic tonsillitis is infectious-allergic diseases of human
body. According to some authors, the incidence of chronic
tonsillitis is 4-10 per cent among adult population and 12-15 per cent among children.
The factors predisposing the onset of chronic tonsillitis are the anatomo-topographic properties of the tonsils (the presence of crypts, and some others) the presence of microflora in the lacunae and conditions favorable for its cultivation, and disordered biological and protective-adaptation mechanisms in the tonsil tissue.
In chronic tonsillitis the flora is not polymorphous in deep parts of the lacunae. Monoflora is usually found: various forms of streptococci (especially of haemolytic staphylococcus). Chronic tonsillitis should be regarded as an infectious disease caused mostly by autoinfection.
Слайд 38
Chronic tonsillitis is usually secondary to acute tonsillitis.
Acute inflammation of the tonsillar tissue is not followed
by complete resolution; it continues and turns into a chronic form. In rare cases chronic tonsillitis can develop without preceding acute inflammation. Permanent autoinfection from chronic foci such as carious teeth, chronic inflammation in the nasal cavity and the paranasal sinuses, or in the pharynx, and also bacterial and local tissue and general autoallergy provoke the onset of chronic tonsillitis.
Слайд 39
The pathological inflammatory changes
are localized in the epithelial coat of the fauces
and in the walls of the tonsillar lacunae, in their parenchyma and stroma, and also in the peritonsillar connective tissue.
The squamous epithelium of the crypts comes off in scales to form fetid caseous masses plugging the crypts and containing numerous bacteria and leukocytes.
The crypts become a most convinient place for the retention and propagation of virulent streptococci and staphylococci whose vital activity keeps up the inflammatory process in the tonsils.
Слайд 40
In unfavourable conditions, like chilling or reduced body
resistance, etc., these bacteria may cause exacerbations, such as
acute tonsillitis, peritonsillar abscess and a number of general complications, for example, infectious polyarthritis, rheumatic heart, nephritis, etc.
Слайд 41
Symptoms and clinical classification of chronic tonsillitis.
Frequently recurring acute tonsillitis in the anamnesis is the
most reliable evidence of chronic tonsillitis. According to various authors, chronic tonsillitis can develop without preceding acute tonsillitis in about 2-4 per cent of cases.
The diagnosis should be based on the assessment of all symptoms taken together because each separate sign can be caused by some other disease of the pharynx, teeth, jaws, nose, etc. Chronic tonsillitis cannot be diagnosed during exacerbation because all pharyngoscopic symptoms will characterize acute rather than chronic tonsillitis.
Only 2-4 weeks after exacerbation it is possible to assess the objective signs of chronic inflammation of the palatine tonsils
Слайд 42
Chronic tonsillitis would be usually exacerbated 2 or
3 times a year, but acute tonsillitis can also
occur 5 and 6 times during one year. In some patients chronic tonsillitis is exacerbated once or twice in the course of 3 or 4 years, but this recurrence should also be considered frequent.
The complaints of the patients are frequently recurring acute inflammation of the tonsils, unpleasant breath, discomfort and feeling of a foreign body in the throat during swallowing, dryness and prickling. The patient often complains of fatigue, flaccidity, headache, decreased working capacity, the temperature is often subfebrile. For many patients, sore throat in the anamnesis is the only complaint.
Inspection of the tonsils and the surrounding tissues reveals ridgelike thickening in the margins of the anterior and posterior palatine arches, their oedema, especially of the upper parts, hyperaemic margins of the palatine arches, often their adhesion to the tonsils and the triangular fold.
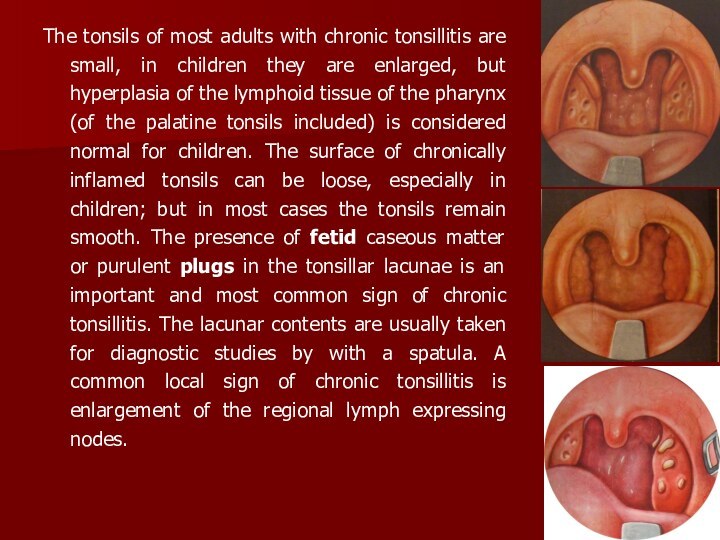
Слайд 43
The tonsils of most adults with chronic tonsillitis
are small, in children they are enlarged, but hyperplasia
of the lymphoid tissue of the pharynx (of the palatine tonsils included) is considered normal for children. The surface of chronically inflamed tonsils can be loose, especially in children; but in most cases the tonsils remain smooth. The presence of fetid caseous matter or purulent plugs in the tonsillar lacunae is an important and most common sign of chronic tonsillitis. The lacunar contents are usually taken for diagnostic studies by with a spatula. A common local sign of chronic tonsillitis is enlargement of the regional lymph expressing nodes.
Слайд 44
Classification of tonsillitis tracts them as following form.
In first compensatory form there are only local symptoms
of chronic inflammation of tonsils. General reaction of organism doesn’t occurs due to sufficient barrier of tonsils and resistance of human body. Second decompensatory form is characterized by disturbance of tosilla function in form of residual tonsillitis, paratonsillitis, paratonsillary abscess, different pathological reactions, diseases of other organs and systems.
Examples of formulating diagnosis: chronic tonsillitis, compensatory type;
chronic tonsillitis, decompensatory type (residual tonsillitis, rheumatism).
Treatment. Treatment of chronic tonsillitis depends on its form. Simple chronic tonsillitis is as a rule managed conservatively, and only if this treatment proves ineffective in 3-4 courses, the tonsils should be removed.
Слайд 46
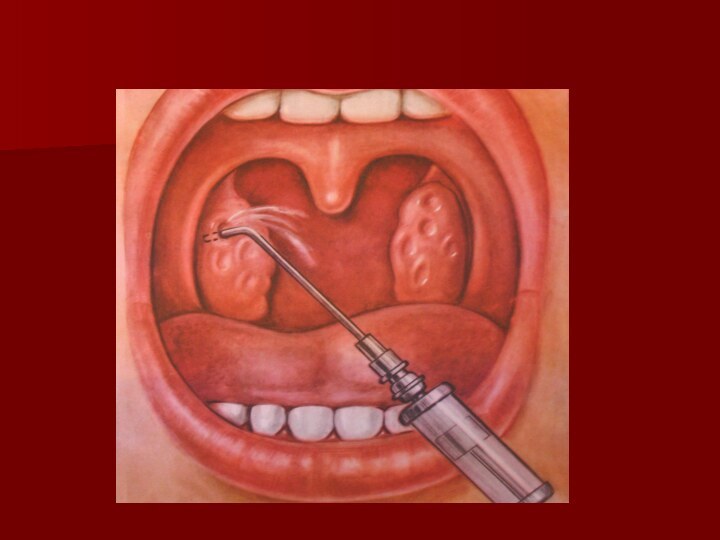
Indications for tonsillectomy are the following:
1. Chronic tonsillitis,
simple in the absence of effect from conservative treatment.
2.
Decompensatory form chronic tonsillitis.
3. Chronic tonsillitis complicated with peritonsillitis.
4. Tonsillogenic sepsis.
Tonsillectomy is absolutely contraindicated in the presence of severe systemic diseases of the cardiovascular system with circulatory insufficiency of the second and third degrees, renal failure with threatening uraemia, severe diabetes mellitus with threatening coma, severe hypertension with possible vascular crises, haemophilia (haemorrhagic diatheses), and other diseases of the blood and the circulatory system (chromocytopaenic purpura, Osler-Rendu syndrome).
Слайд 47
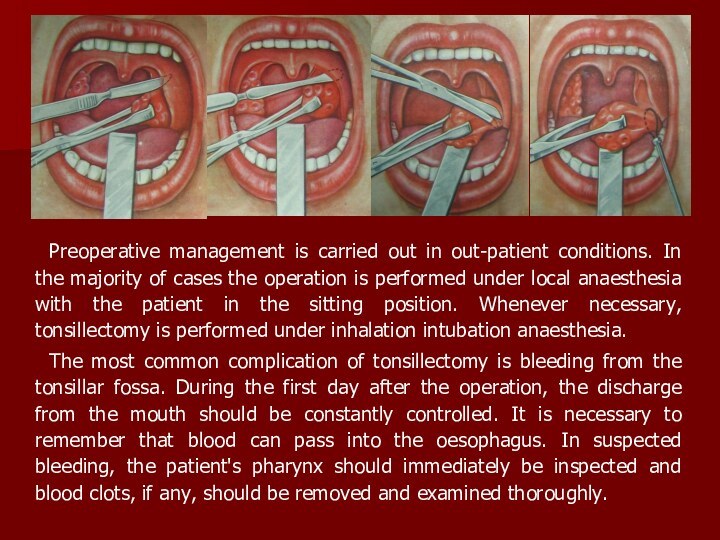
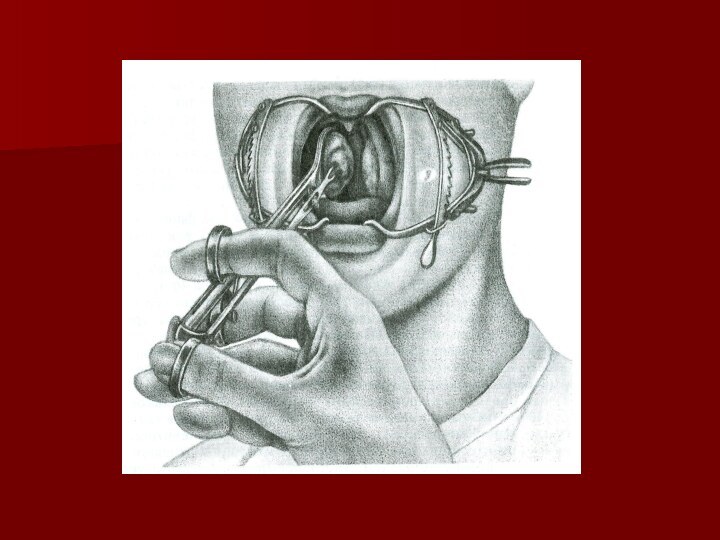
Preoperative management is carried out in out-patient conditions.
In the majority of cases the operation is performed
under local anaesthesia with the patient in the sitting position. Whenever necessary, tonsillectomy is performed under inhalation intubation anaesthesia.
The most common complication of tonsillectomy is bleeding from the tonsillar fossa. During the first day after the operation, the discharge from the mouth should be constantly controlled. It is necessary to remember that blood can pass into the oesophagus. In suspected bleeding, the patient's pharynx should immediately be inspected and blood clots, if any, should be removed and examined thoroughly.
Слайд 48
.
As distinct from vascular bleeding, parenchymatous bleeding
is usually not profuse. It can be managed by
haemostatics, such as дицинон ln parenterally, a 10 per cent calcium gluconate solution intravenously. The tonsillar fossa should be packed with a tampon soaked with haemostatics.
In rare cases bleeding occurs at later terms: in 7-10 days after the operation. It should be arrested as described above. The patient should be hospitalized.
Prophylactic measures against chronic tonsillitis are substantially the same as against acute tonsillitis. There exist individual and social aspects in prevention of tonsillitis. Individual prophylaxis includes invigorating measures which strengthen the patient's resistance to infection and unfavorable environmental conditions.
Слайд 49
HYPERTROPHY OF LYMPHOID TISSUE OF THE PHARYNX
The volume
of lymphoid tissue of the pharynx can vary significantly
depending on its functional activity.
But hypertrophy of the pharyngeal lymphoid tissue can sometimes be persistent. Hypertrophy may be so significant that respiration not only through the nose but also through the mouth becomes difficult; food is swallowed with difficulty and speech is impaired.
The function of the auditory tubes is affected as well. In the overwhelming majority of cases, the palatine tonsils are hypertrophied significantly only before the onset of sexual maturation. Less frequently they are enlarged in persons aged under 30.
Слайд 50
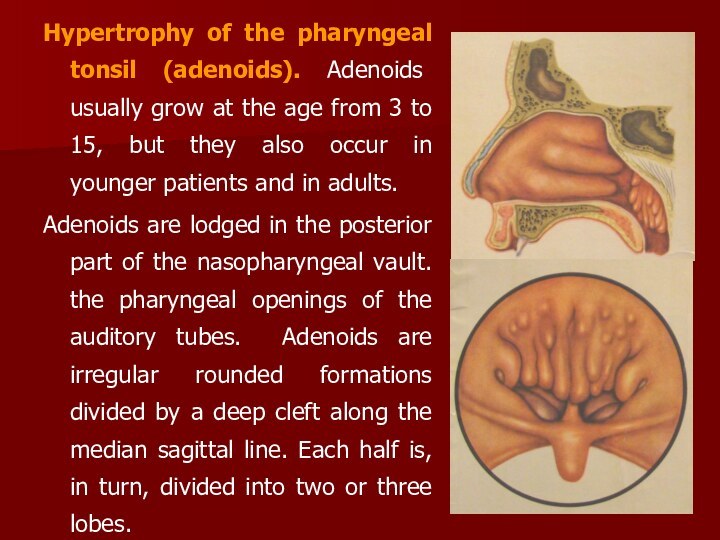
Hypertrophy of the pharyngeal tonsil (adenoids). Adenoids usually
grow at the age from 3 to 15, but
they also occur in younger patients and in adults.
Adenoids are lodged in the posterior part of the nasopharyngeal vault. the pharyngeal openings of the auditory tubes. Adenoids are irregular rounded formations divided by a deep cleft along the median sagittal line. Each half is, in turn, divided into two or three lobes.
Слайд 51
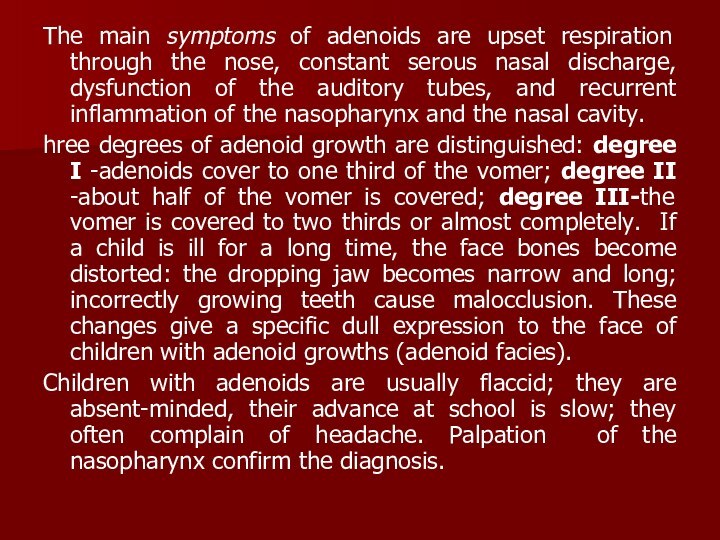
The main symptoms of adenoids are upset respiration
through the nose, constant serous nasal discharge, dysfunction of
the auditory tubes, and recurrent inflammation of the nasopharynx and the nasal cavity.
hree degrees of adenoid growth are distinguished: degree I -adenoids cover to one third of the vomer; degree II -about half of the vomer is covered; degree III-the vomer is covered to two thirds or almost completely. If a child is ill for a long time, the face bones become distorted: the dropping jaw becomes narrow and long; incorrectly growing teeth cause malocclusion. These changes give a specific dull expression to the face of children with adenoid growths (adenoid facies).
Children with adenoids are usually flaccid; they are absent-minded, their advance at school is slow; they often complain of headache. Palpation of the nasopharynx confirm the diagnosis.
Слайд 52
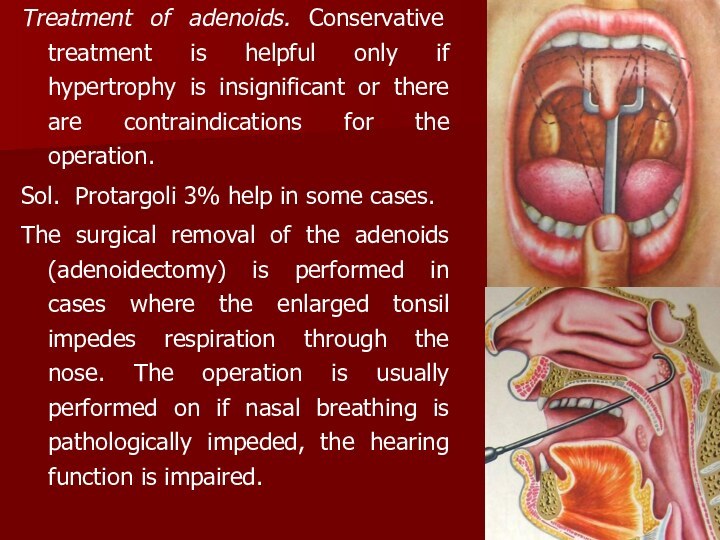
Treatment of adenoids. Conservative treatment is helpful only
if hypertrophy is insignificant or there are contraindications for
the operation.
Sol. Protargoli 3% help in some cases.
The surgical removal of the adenoids (adenoidectomy) is performed in cases where the enlarged tonsil impedes respiration through the nose. The operation is usually performed on if nasal breathing is pathologically impeded, the hearing function is impaired.
Слайд 53
Children can be operated under out-patient conditions, while
adults only in hospital. Contraindications for adenoidectomy are diseases
of the blood, severe diseases of the cardiovascular system, and infectious diseases (the patient may be operated on only in 1-2 months after the disease). Hot or spicy foods should not be given, since bleeding can resume for 4-5 days. Physical strain, active movements and chilling should be avoided.
Hypertrophy of the palatine tonsils. Hypertrophied tonsils can interfere with normal respiration through the mouth, speech, and swallowing of food. If hypertrophy of the palatine tonsils concurs with adenoids, the respiratory function is severely upset. The child suffers from paroxysmal asphyxia during sleep, he is tortured by cough and frequently wakes up during sleep.
Слайд 54
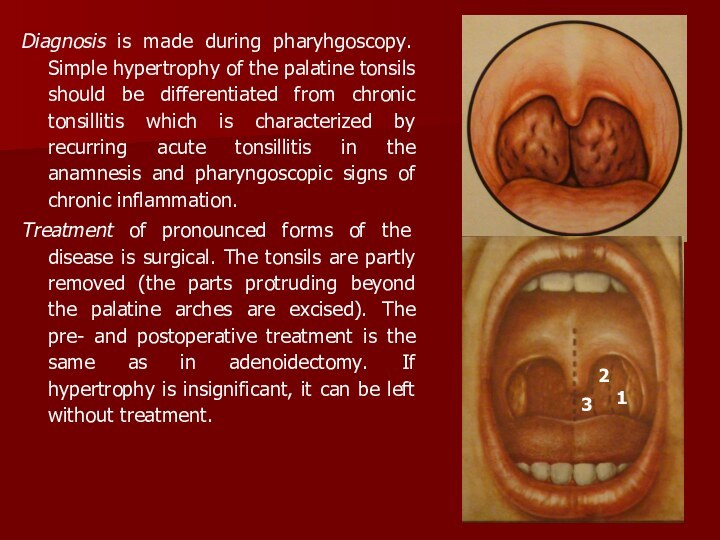
Diagnosis is made during pharyhgoscopy. Simple hypertrophy of
the palatine tonsils should be differentiated from chronic tonsillitis
which is characterized by recurring acute tonsillitis in the anamnesis and pharyngoscopic signs of chronic inflammation.
Treatment of pronounced forms of the disease is surgical. The tonsils are partly removed (the parts protruding beyond the palatine arches are excised). The pre- and postoperative treatment is the same as in adenoidectomy. If hypertrophy is insignificant, it can be left without treatment.
3
2
1