- Главная
- Разное
- Бизнес и предпринимательство
- Образование
- Развлечения
- Государство
- Спорт
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Религиоведение
- Черчение
- Физкультура
- ИЗО
- Психология
- Социология
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Геометрия
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Что такое findslide.org?
FindSlide.org - это сайт презентаций, докладов, шаблонов в формате PowerPoint.
Обратная связь
Email: Нажмите что бы посмотреть
Презентация на тему Diabetes Anterior hypophysis Diabetes insipidus
Содержание
- 2. DiabetesDefinition ,classification, type 1 and 2, acute and chronic complications , treatment
- 3. Diabetes definitionDiabetes is a heterogeneous, complex metabolic
- 4. Classification of disorders of glycemia Type 1-
- 5. Criteria for diabetes diagnosis according to
- 6. Factors affecting HbA1C
- 7. Diabetes type 1Usually caused by autoimmune heterogenic
- 8. Diabetes type 1Roughly 5-15% of all cases
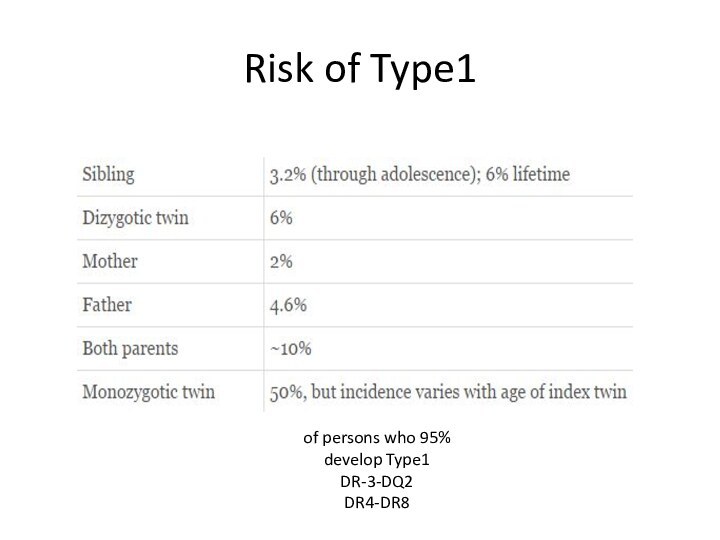
- 9. Risk of Type195% of persons who develop Type1DR-3-DQ2DR4-DR8
- 10. Autoantibodies (90% at the diagnosis of type
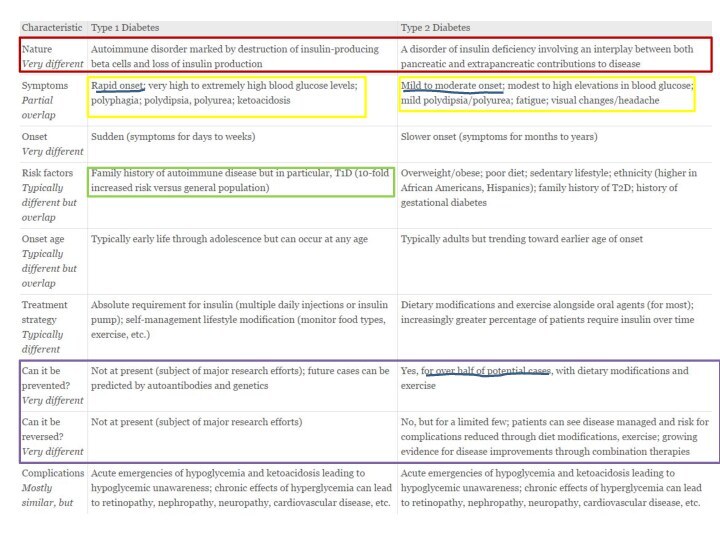
- 12. Diabetes type290 % of all diabetes in
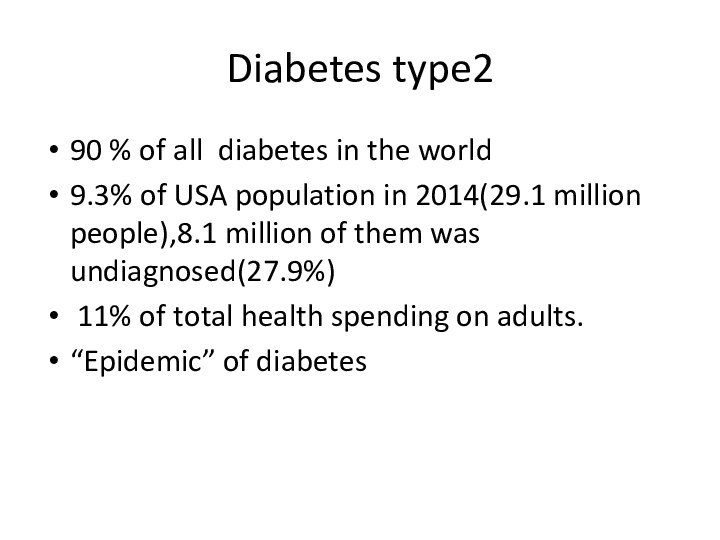
- 13. Pathogenesis of type 2
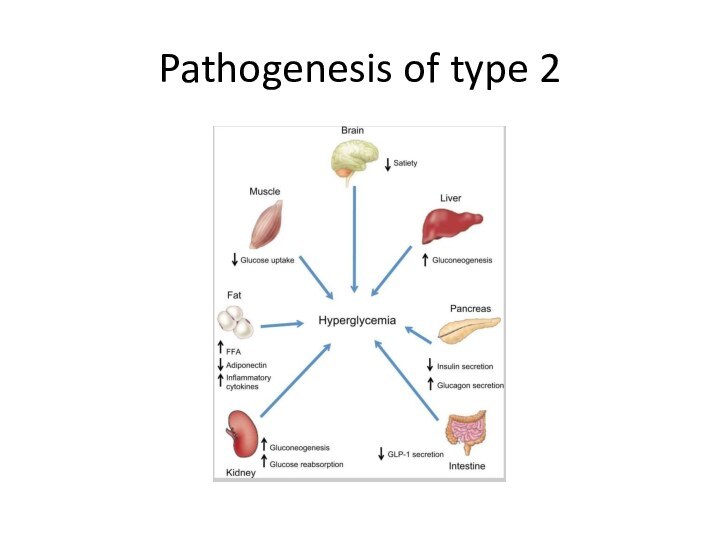
- 14. Genetic defects of insulin secretion2-5% of
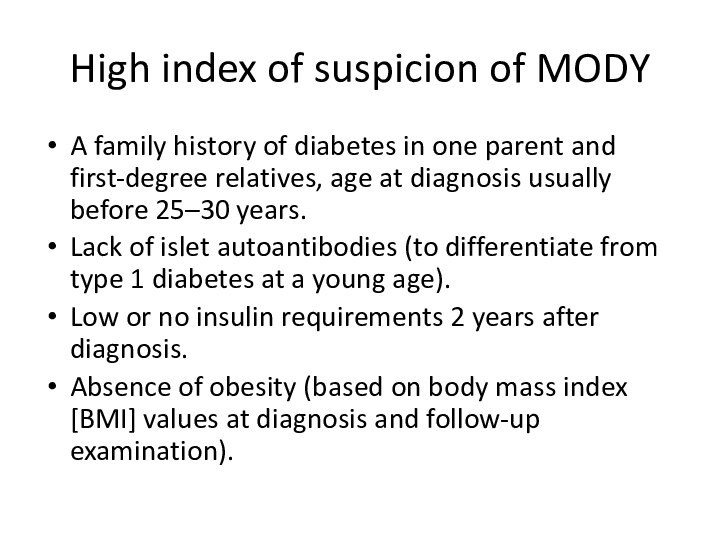
- 15. High index of suspicion of MODYA family
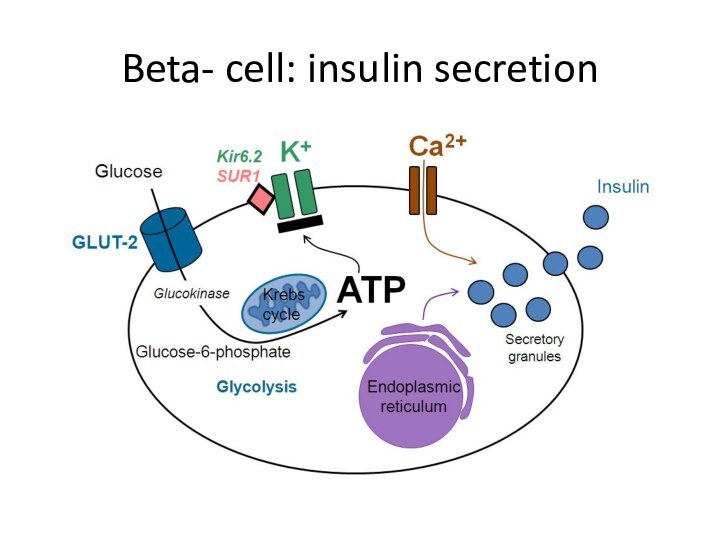
- 16. Beta- cell: insulin secretion
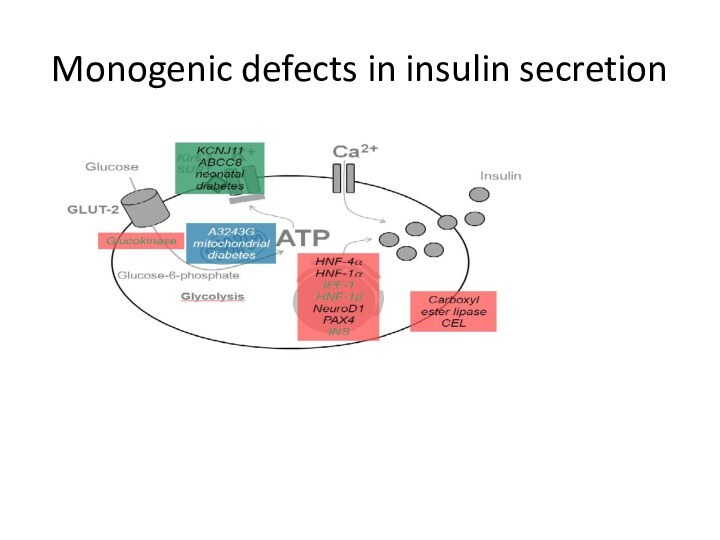
- 17. Monogenic defects in insulin secretion
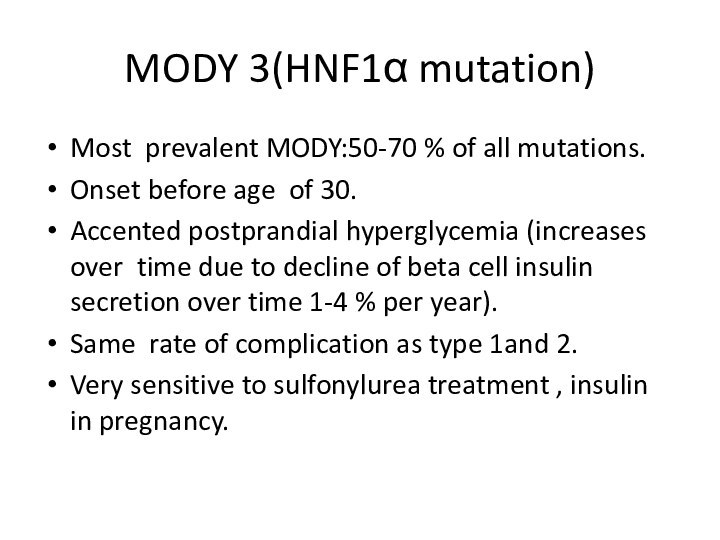
- 18. MODY 3(HNF1α mutation)Most prevalent MODY:50-70 % of
- 19. MODY 2Mild hyperglycemia started at birth.The glucokinase
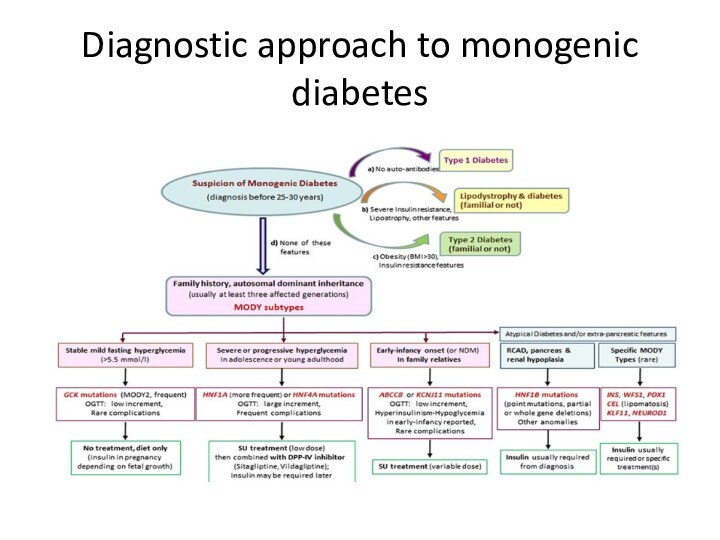
- 20. Diagnostic approach to monogenic diabetes
- 21. Genetic defects in insulin actionRabson Mendenhall :short
- 22. Disorder of exocrine pancreasChronic pancreatitis: more than
- 23. EndocrinopathiesCushing disease and syndrome-glucose intolerance and overt
- 24. examples))Drug and chemicalsEthanol – chronic pancreatitis-overt diabetes(1%
- 25. InfectionsPredisposition to type 1- enteroviruses.Direct beta- cells
- 26. Uncommon immune form of diabetes High titers
- 27. Pregnancy in women with normal
- 28. Gestational diabetes mellitus(GDM)Disbalance between insulin secretion and
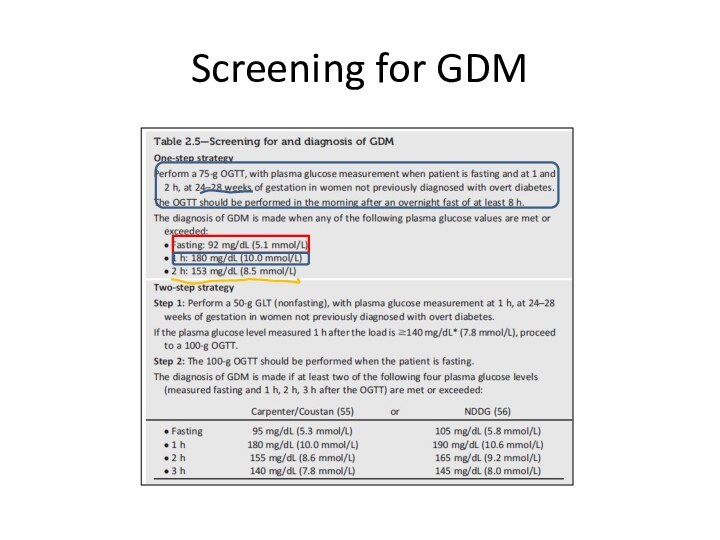
- 29. Screening for GDM
- 30. Algorithm of glucose testing in pregnancyAll women
- 31. Goals of diabetes treatmentPrevent macrovasular diabetes complication-cardiovascular
- 32. Aspects of diabetes treatmentGlycemic control Lifestyle intervention
- 33. Glycemic control and diabetic complicationType 1 study:
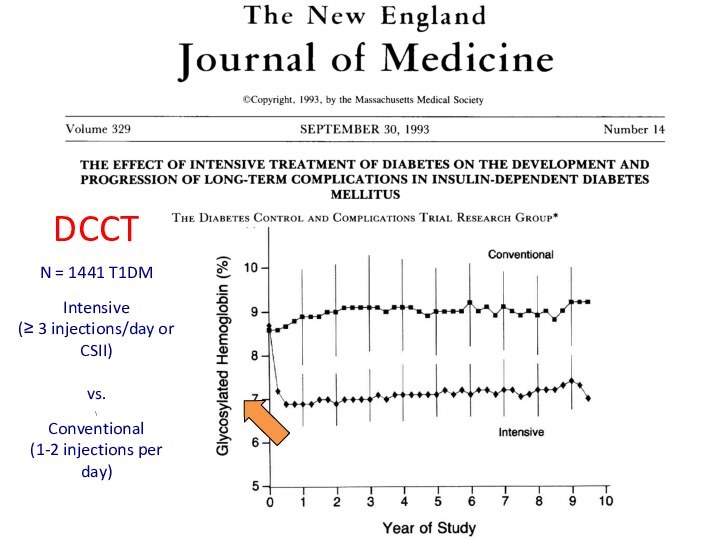
- 34. DCCT N = 1441 T1DM
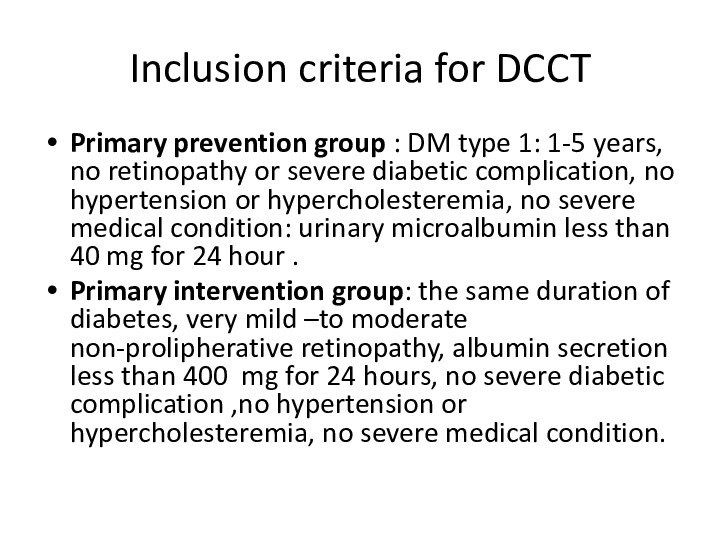
- 35. Inclusion criteria for DCCT Primary prevention group
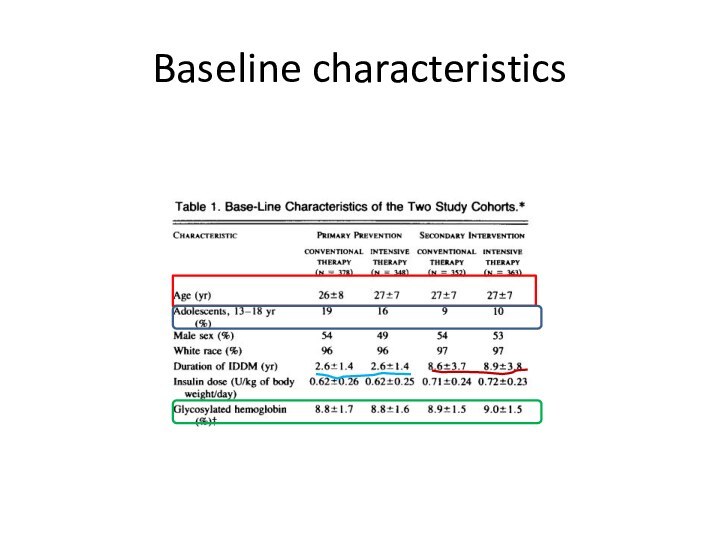
- 36. Baseline characteristics
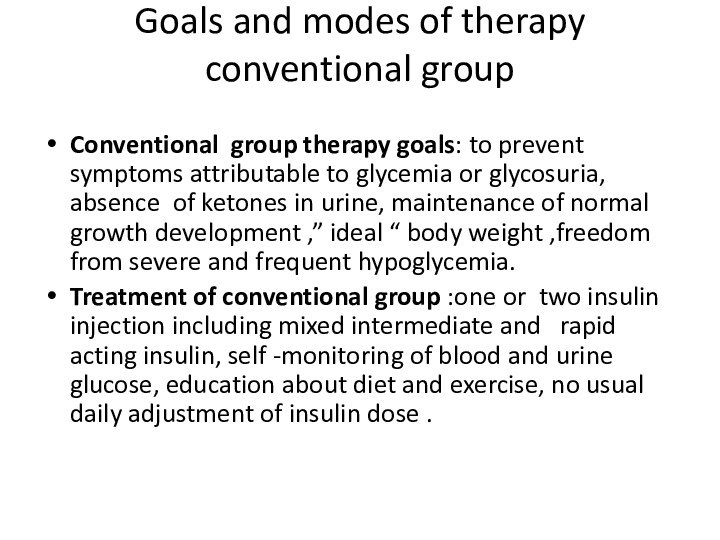
- 37. Goals and modes of therapy conventional group
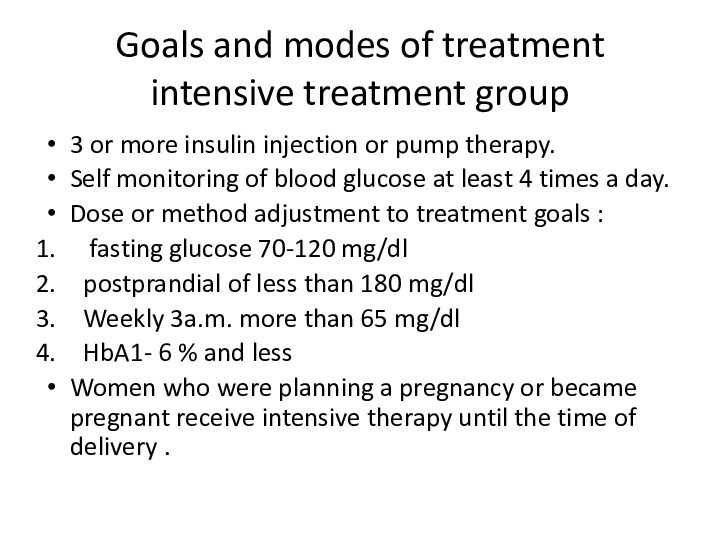
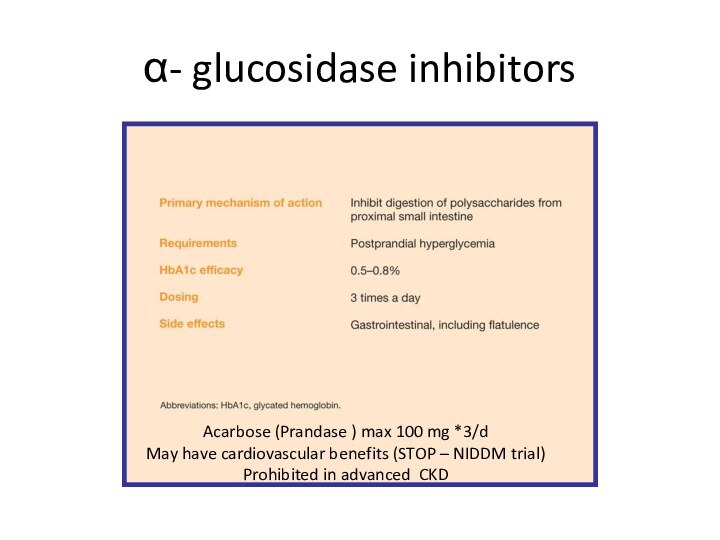
- 38. Goals and modes of treatment intensive
- 39. Study questions Prevention of diabetic retinopathy in
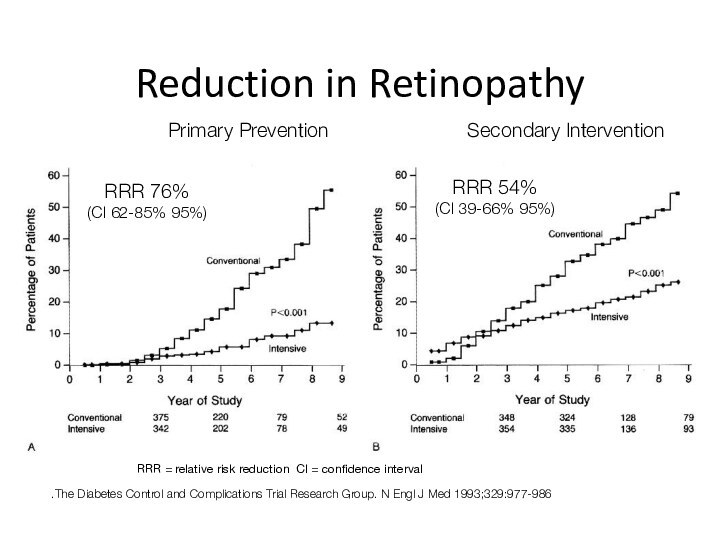
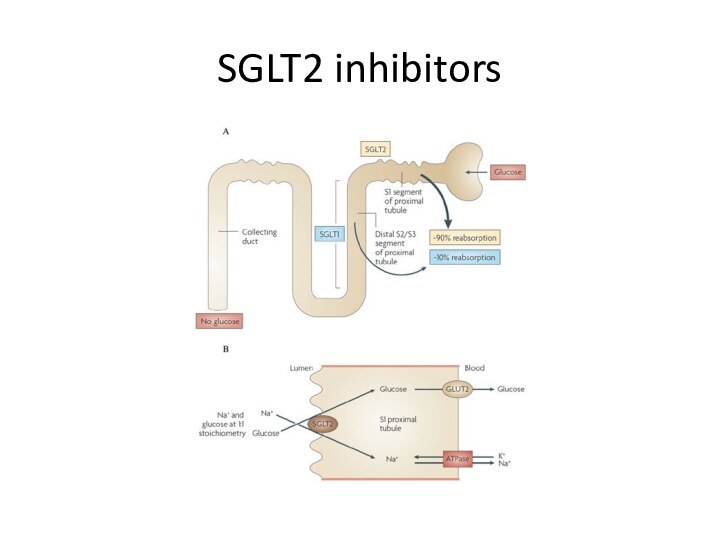
- 40. Reduction in RetinopathyThe Diabetes Control and Complications
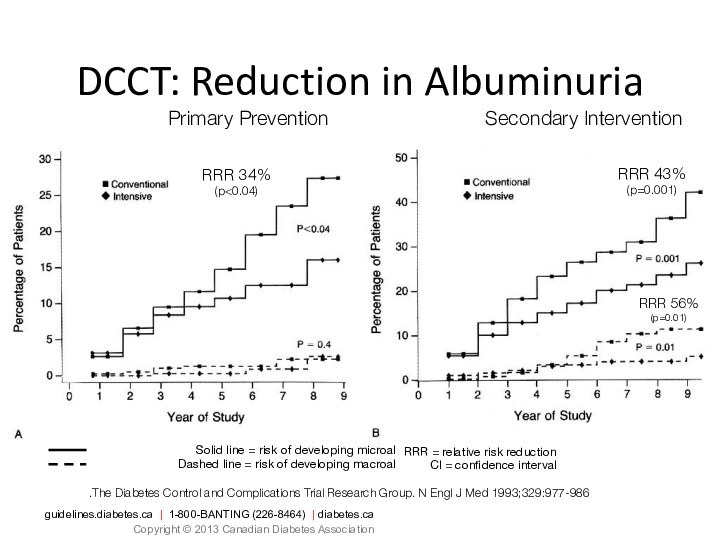
- 41. Solid line = risk of developing microalbuminuriaDashed
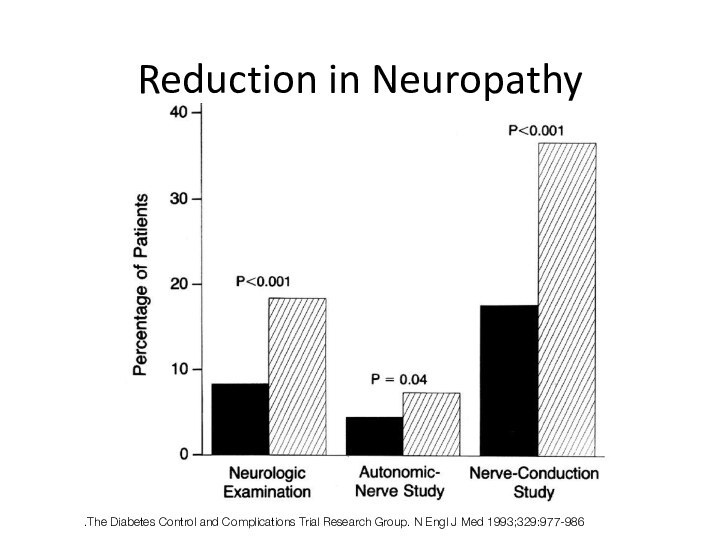
- 42. Reduction in NeuropathyThe Diabetes Control and Complications Trial Research Group. N Engl J Med 1993;329:977-986.
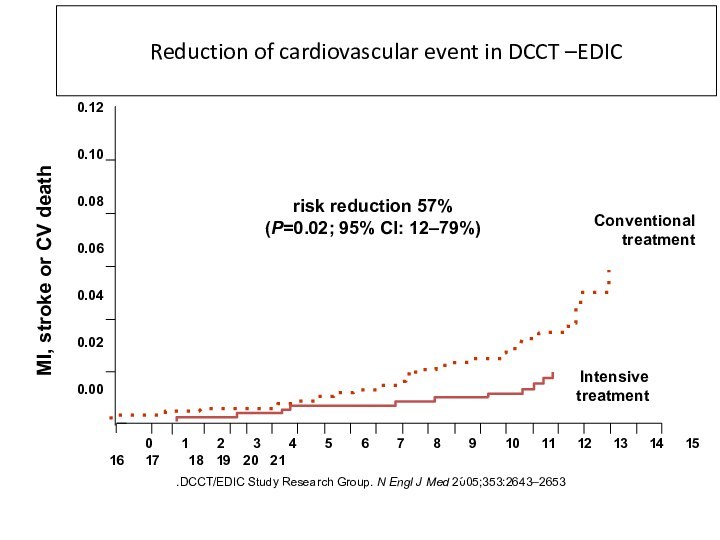
- 43. DCCT/EDIC Study Research Group. N Engl J
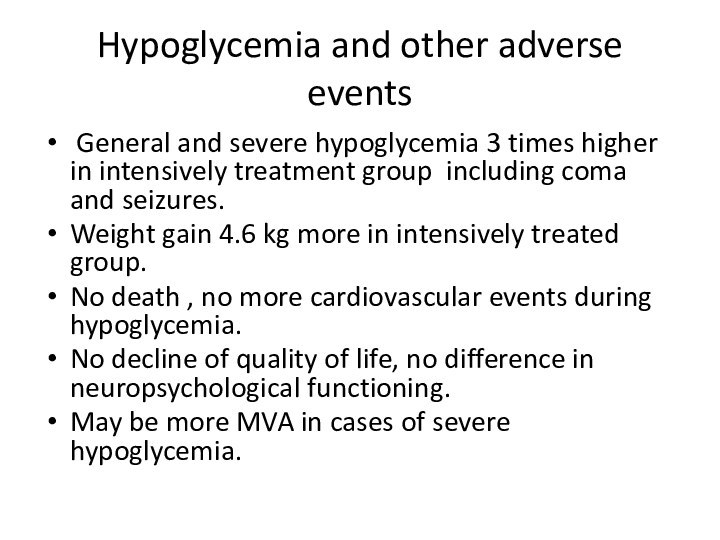
- 44. Hypoglycemia and other adverse events General and
- 45. GLYCEMIC CONTROL IN TYPE 2
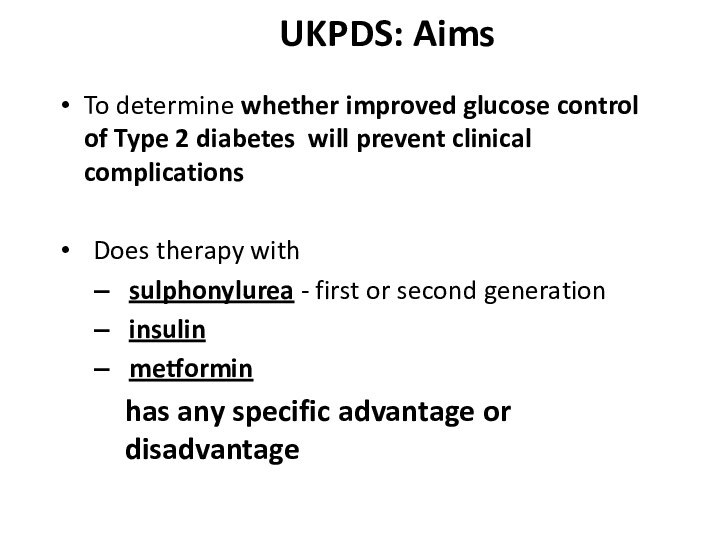
- 46. UKPDS: AimsTo determine whether improved glucose control
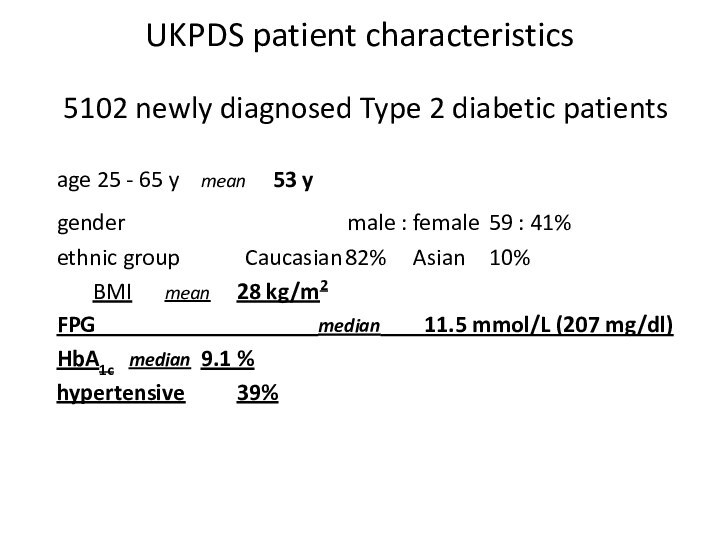
- 47. UKPDS patient characteristics5102 newly diagnosed Type 2
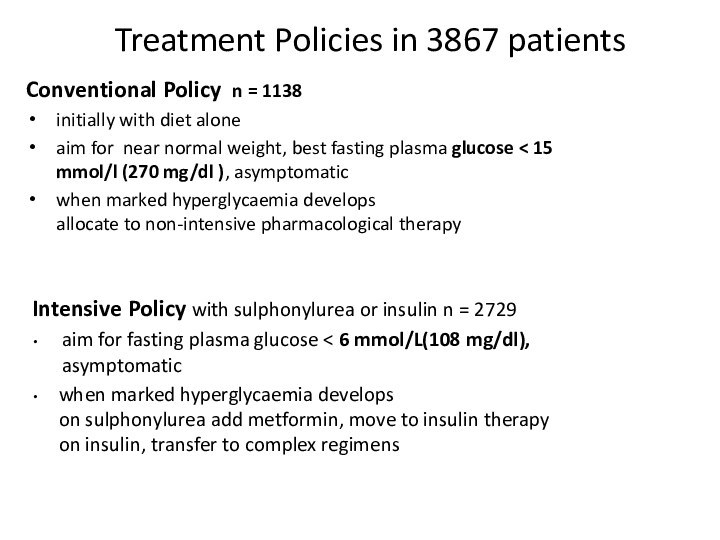
- 48. Treatment Policies in 3867 patientsConventional Policy n
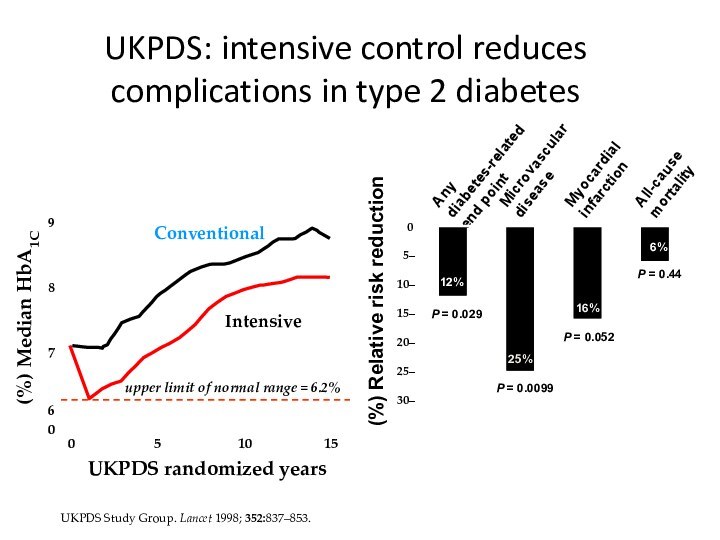
- 49. UKPDS Study Group. Lancet 1998; 352:837–853. UKPDS: intensive control reduces complications in type 2 diabetes
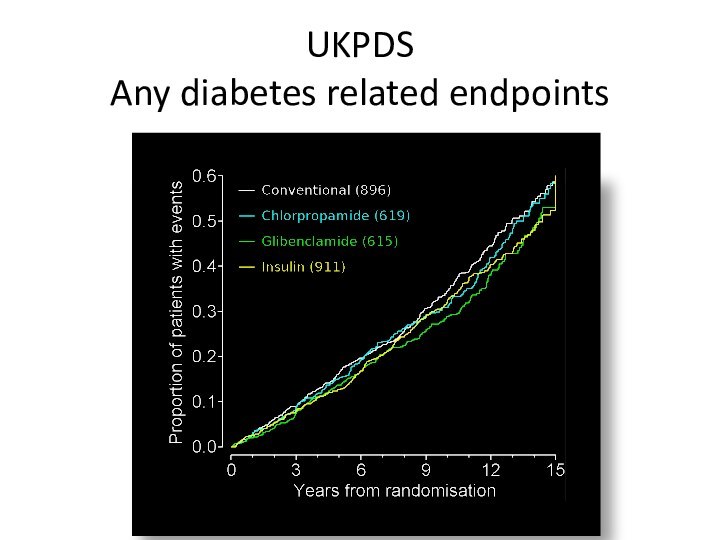
- 50. UKPDS Any diabetes related endpoints
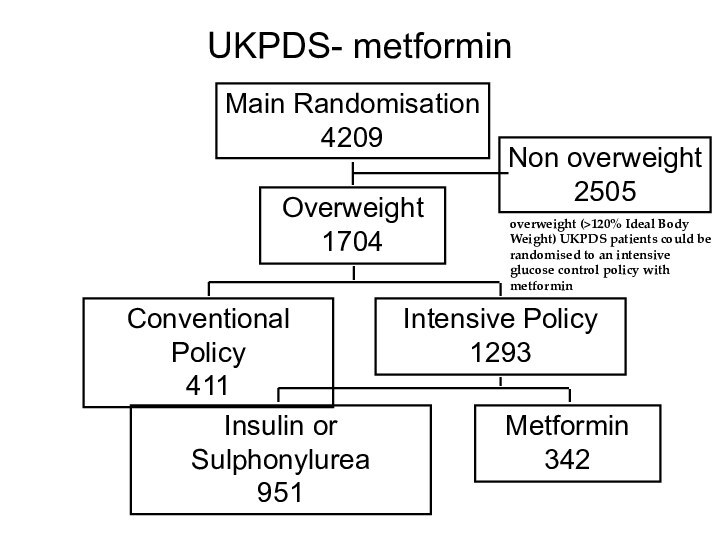
- 51. UKPDS- metformin Main Randomisation 4209Overweight 1704Non overweight
- 52. Metformin in overweight patients in comparison with
- 53. ACCORD trial 10251 patients with diabetes with
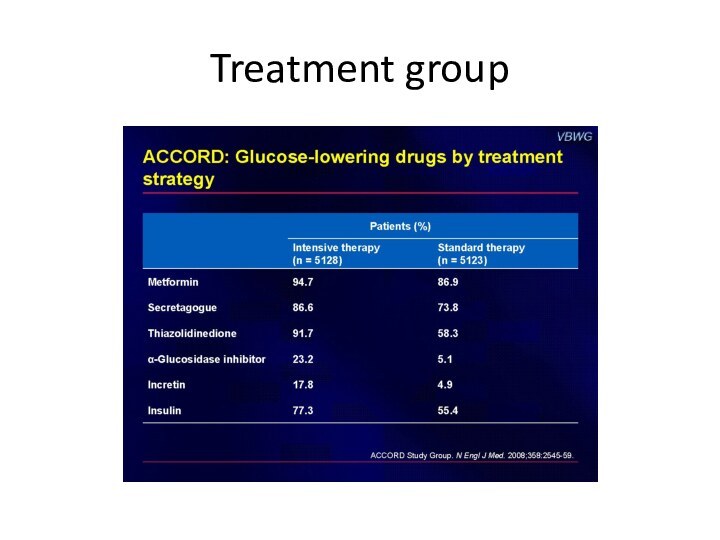
- 54. Treatment group
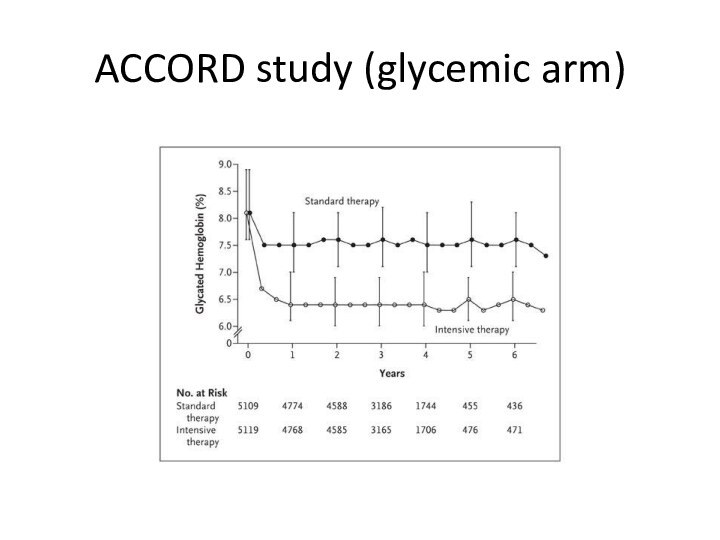
- 55. (ACCORD study (glycemic arm
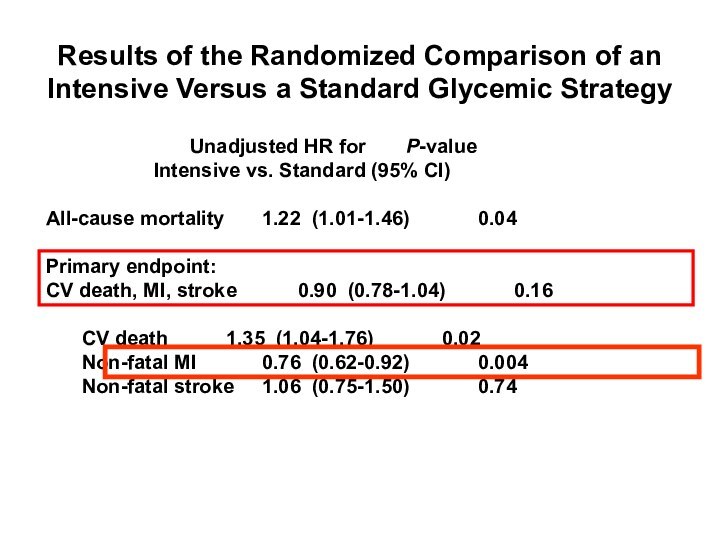
- 56. Gerstein HC et al. The ACCORD Study
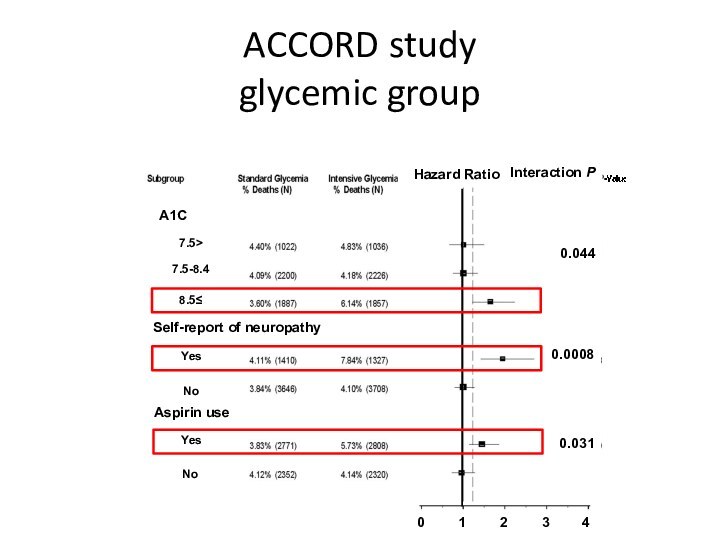
- 57. ACCORD study glycemic group
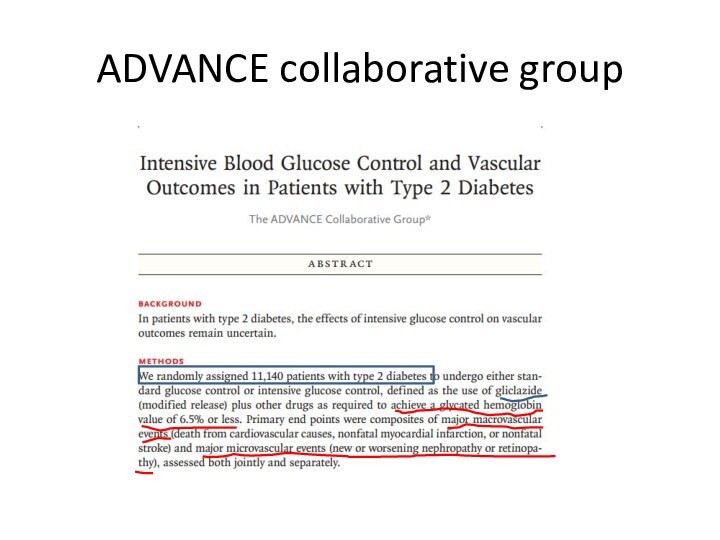
- 58. ADVANCE collaborative group
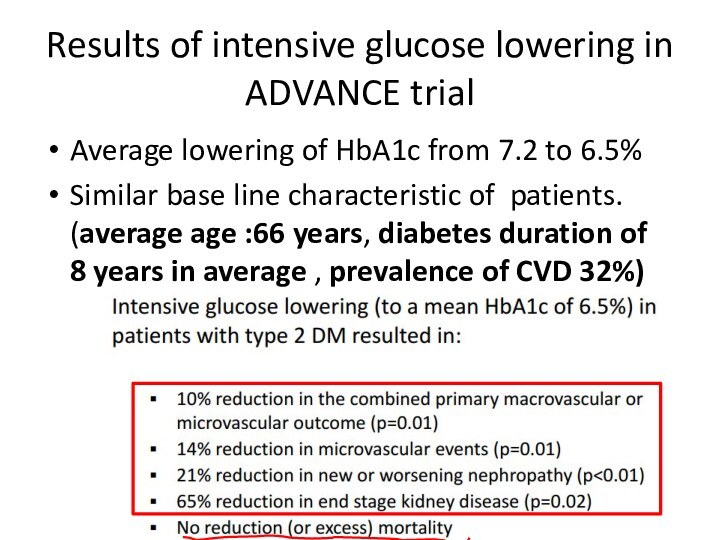
- 59. Results of intensive glucose lowering in ADVANCE
- 60. VA Diabetes Trial (VADT)Similar study design: intensive
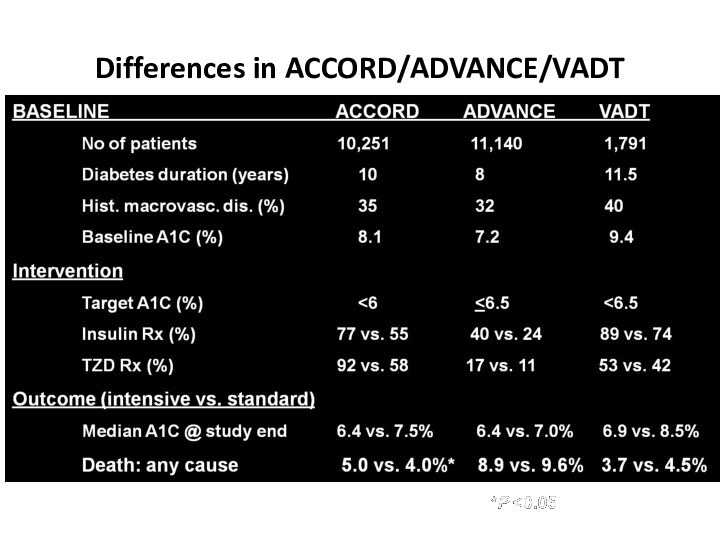
- 61. Differences in ACCORD/ADVANCE/VADTSkyler JS, Bergenstal R, Bonow RO, et al. Diabetes Care. 2009;32:187-192.
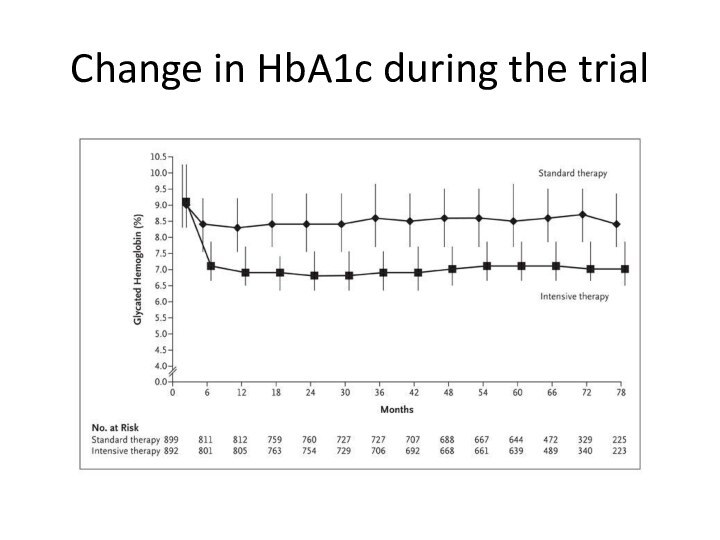
- 62. Change in HbA1c during the trial
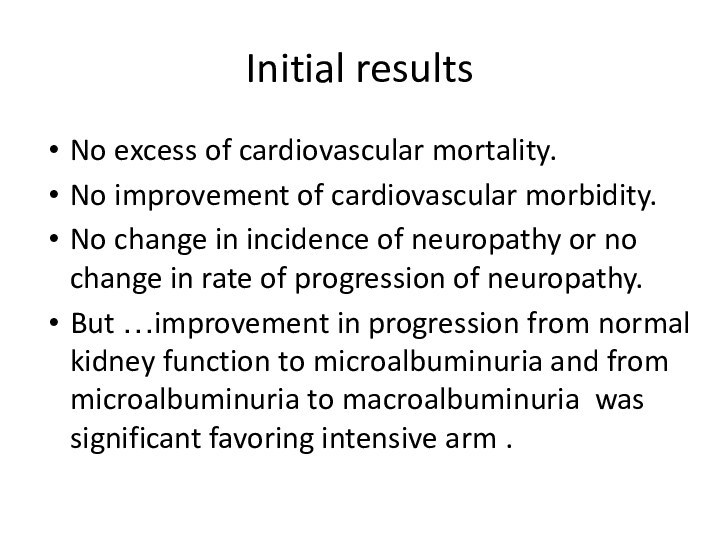
- 63. Initial resultsNo excess of cardiovascular mortality.No improvement
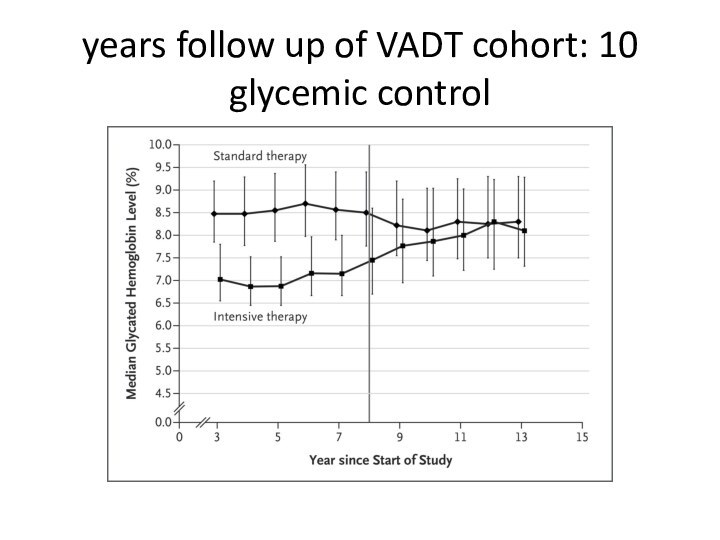
- 64. 10 years follow up of VADT cohort: glycemic control
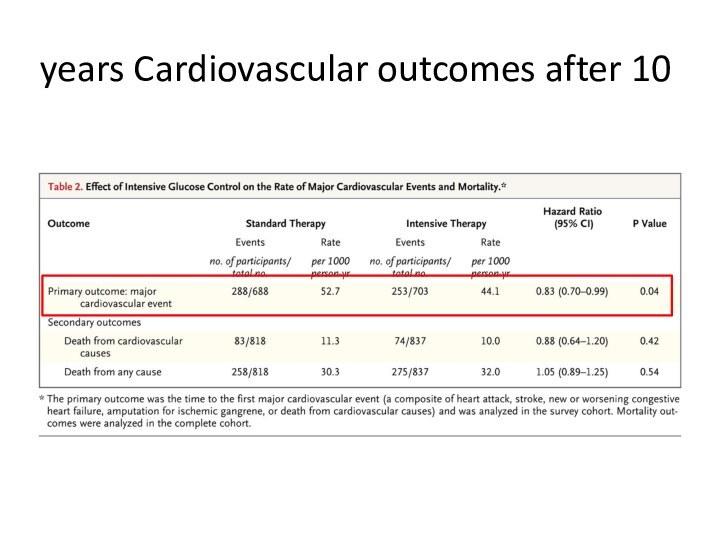
- 65. Cardiovascular outcomes after 10 years
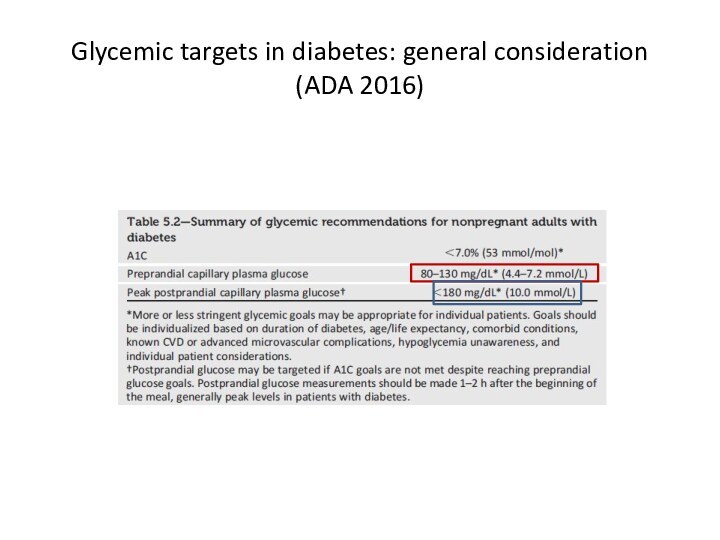
- 66. Glycemic targets in diabetes: general consideration (ADA 2016)
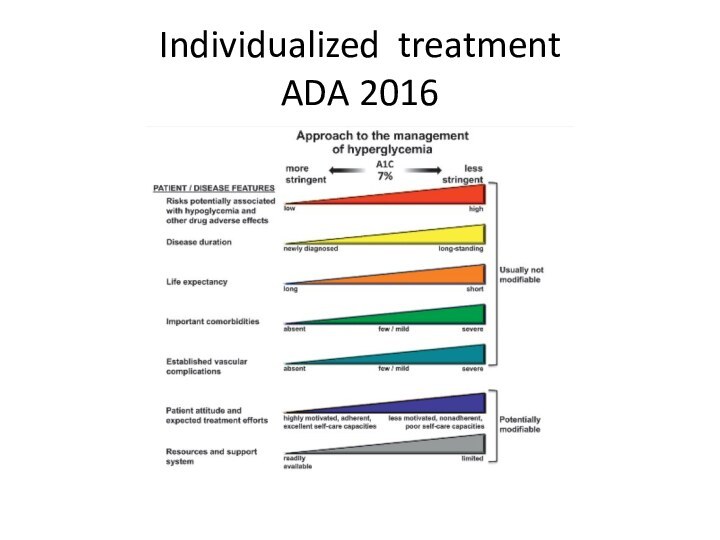
- 67. Individualized treatment ADA 2016
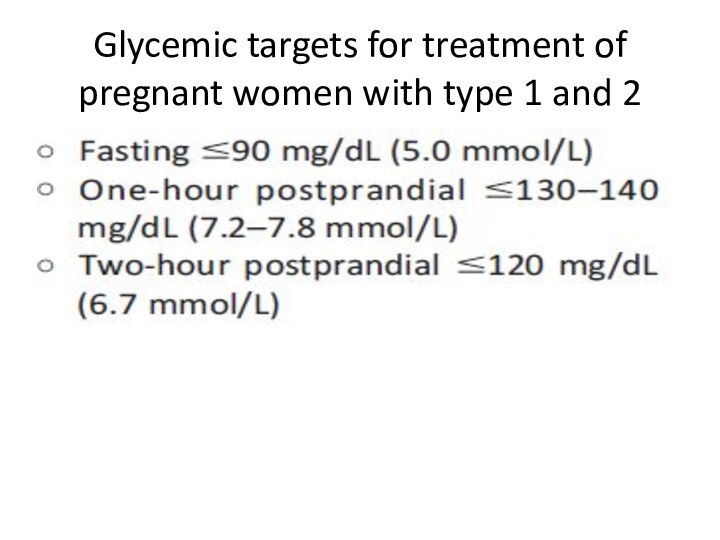
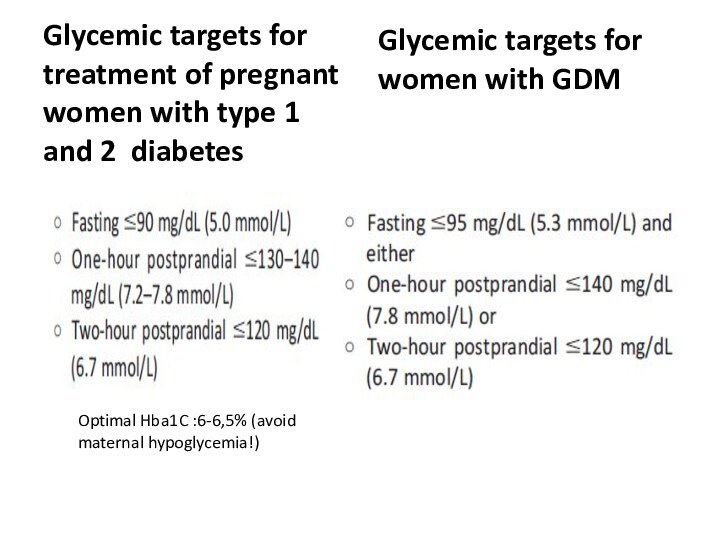
- 68. Glycemic targets for treatment of pregnant women with type 1 and 2
- 69. Glycemic targets for treatment of pregnant women
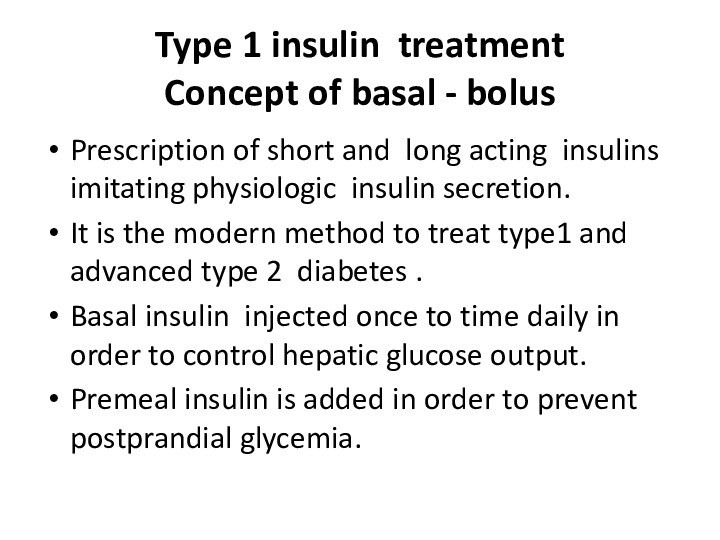
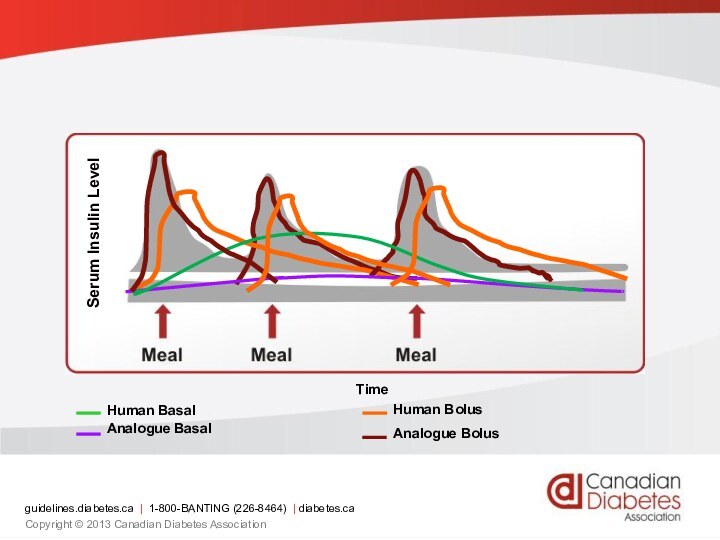
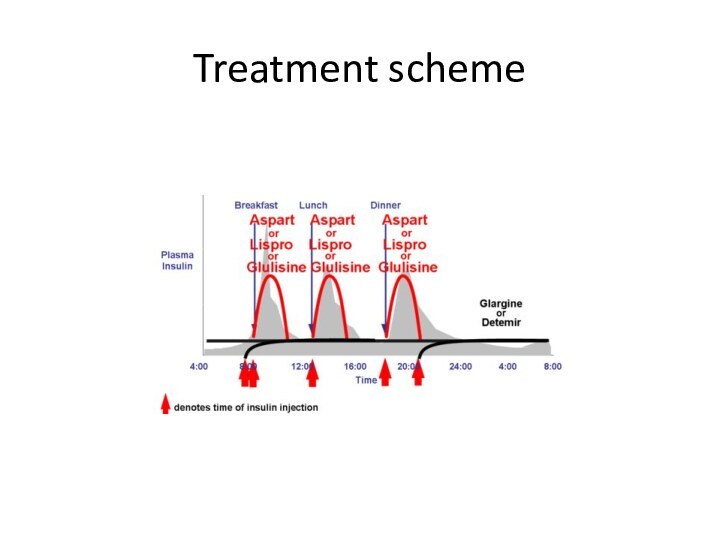
- 70. Type 1 insulin treatment Concept of
- 71. Serum Insulin LevelTimeguidelines.diabetes.ca | 1-800-BANTING (226-8464) | diabetes.caCopyright © 2013 Canadian Diabetes Association
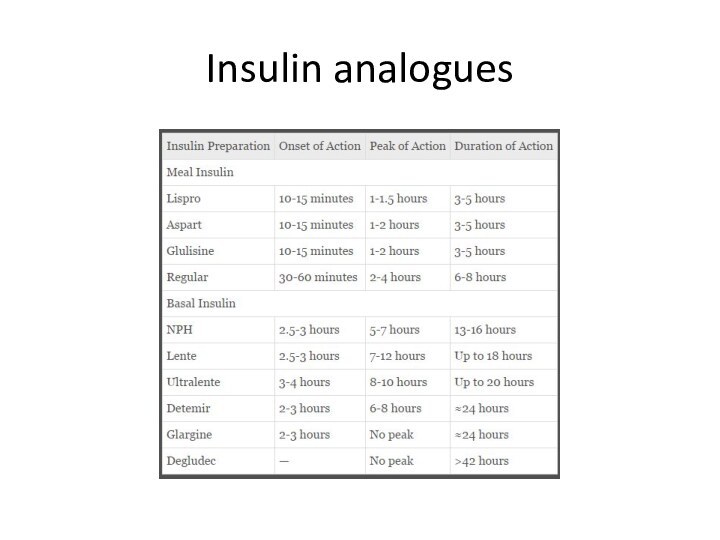
- 72. Insulin analogues
- 73. Treatment scheme
- 74. :Principles of type 2 treatment (1)non –pharmacologic
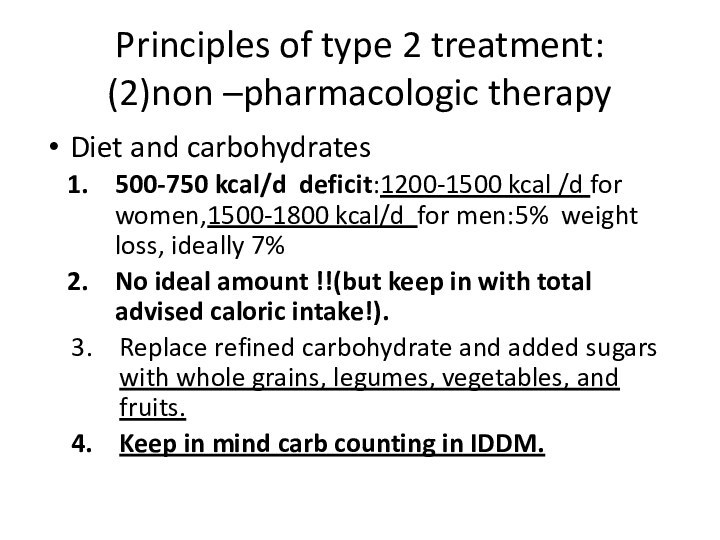
- 75. :Principles of type 2 treatment (2)non –pharmacologic
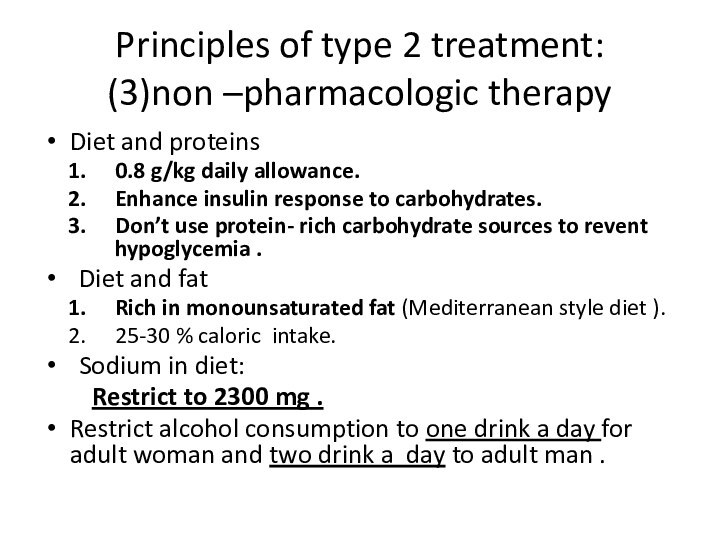
- 76. :Principles of type 2 treatment (3)non –pharmacologic
- 77. Pharmacological treatment of glycemia type 2:drug classificationBiguanidesSecretagoguesDPP4 inhibitorsα- glycosidase inhibitorThiazolidinedioneGLP1 agonistsSGLT2 inhibitorsInsulin
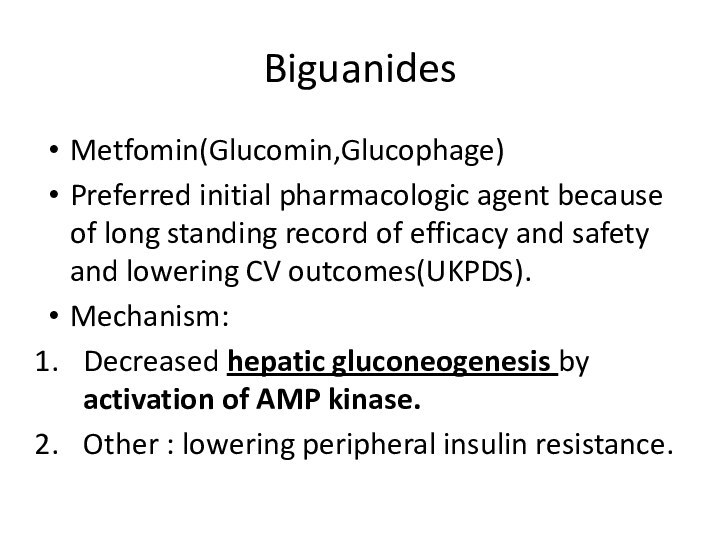
- 78. BiguanidesMetfomin(Glucomin,Glucophage)Preferred initial pharmacologic agent because of long
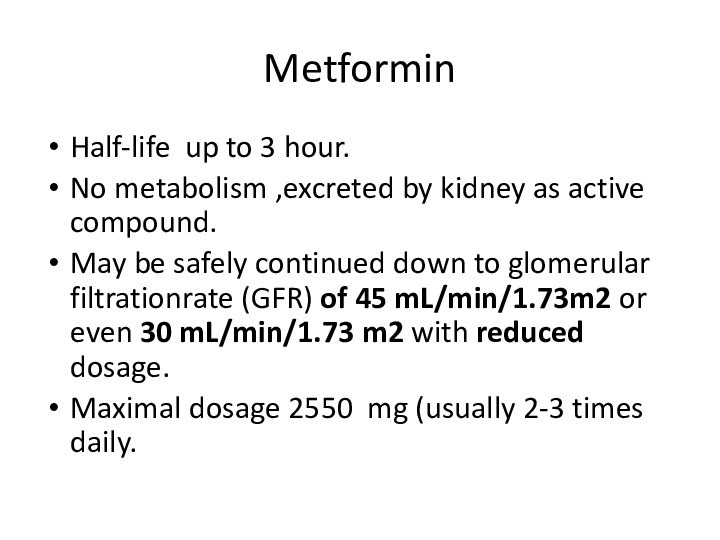
- 79. MetforminHalf-life up to 3 hour.No metabolism ,excreted
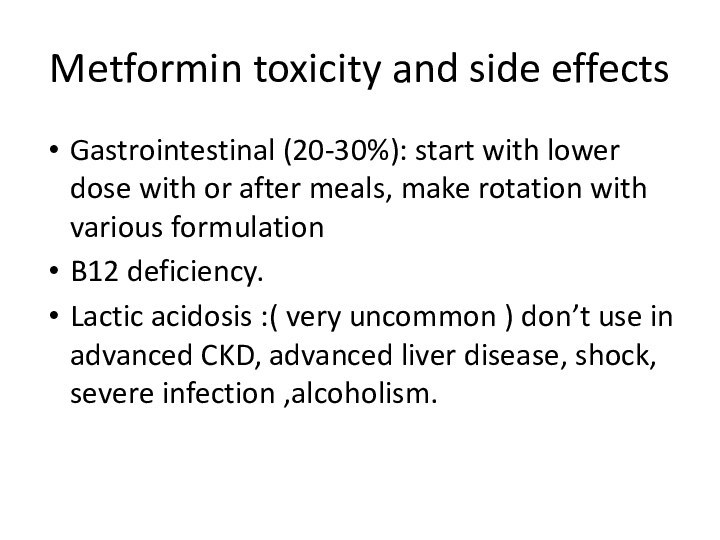
- 80. Metformin toxicity and side effectsGastrointestinal (20-30%): start
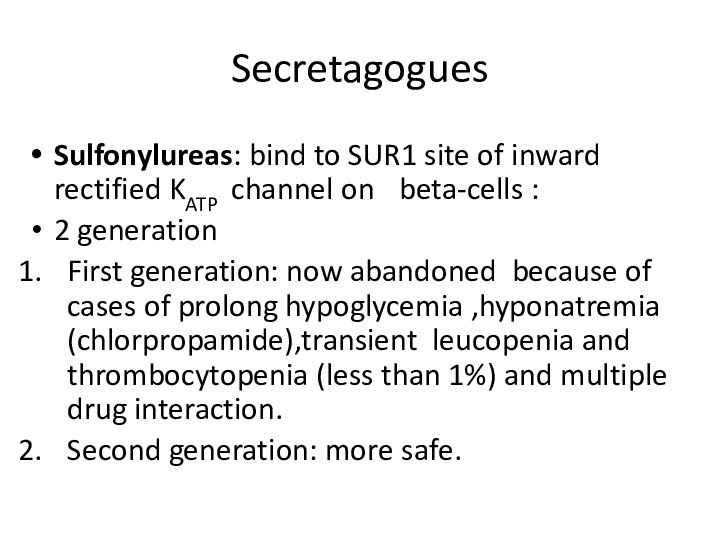
- 81. SecretagoguesSulfonylureas: bind to SUR1 site of inward
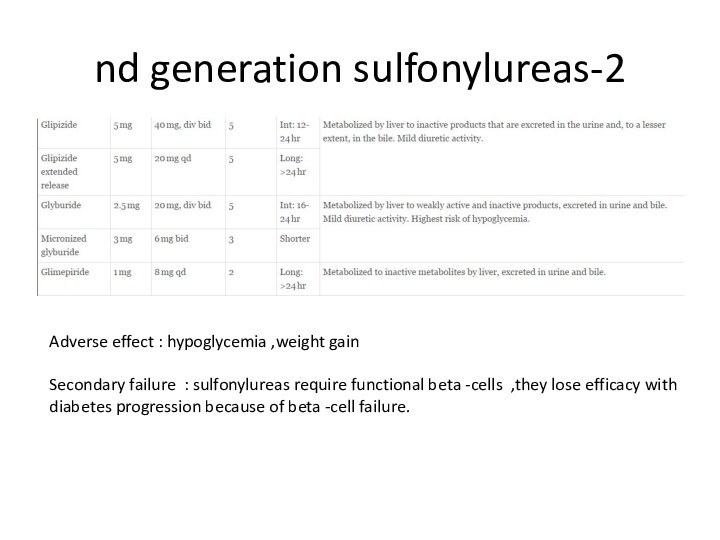
- 82. 2-nd generation sulfonylureasAdverse effect : hypoglycemia ,weight
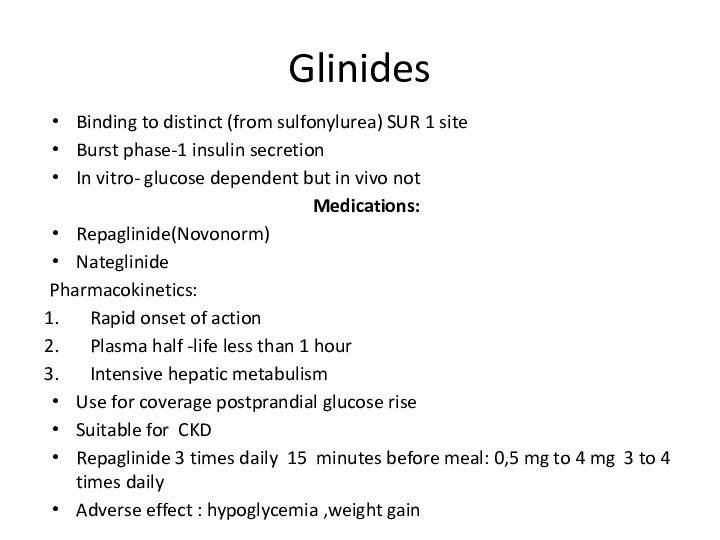
- 83. GlinidesBinding to distinct (from sulfonylurea) SUR 1
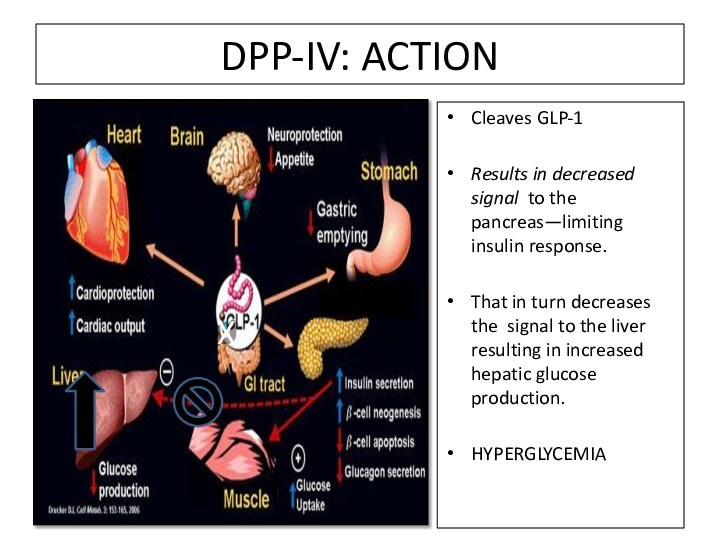
- 84. DPP-IV: ACTIONCleaves GLP-1Results in decreased signal to
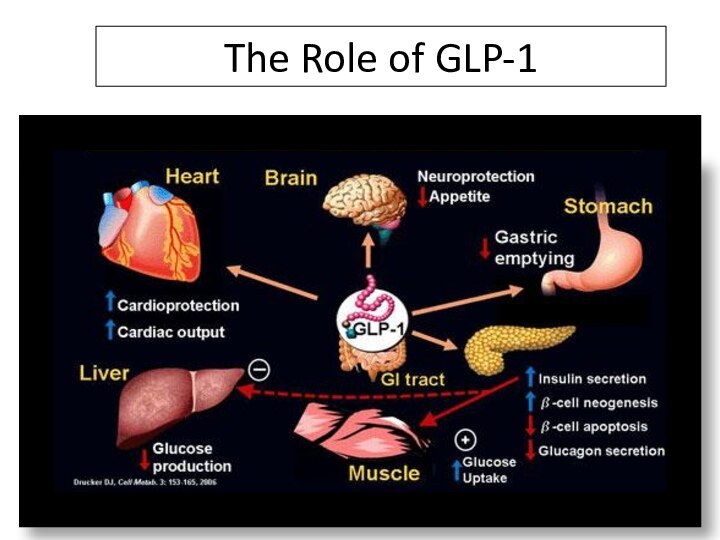
- 85. The Role of GLP-1DPP-4 Inhibitors Increase ½ Life of GLP-1
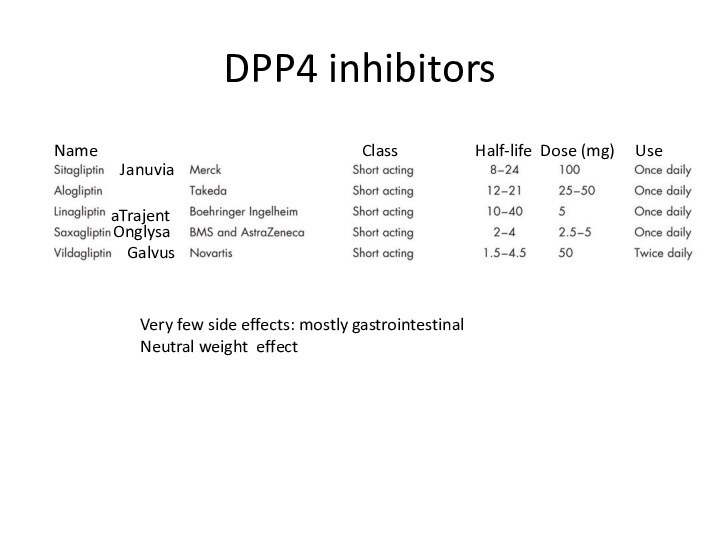
- 86. DPP4 inhibitorsJanuviaTrajentaOnglysaGalvusName
- 87. GLP1 agonists(injectable agents)Breakthrough in DM 2
- 88. α- glucosidase inhibitorsAcarbose (Prandase ) max 100
- 89. Thiazolidinediones Gamma- PPAR agonists.Increase of insulin sensitivity
- 90. SGLT2 inhibitors
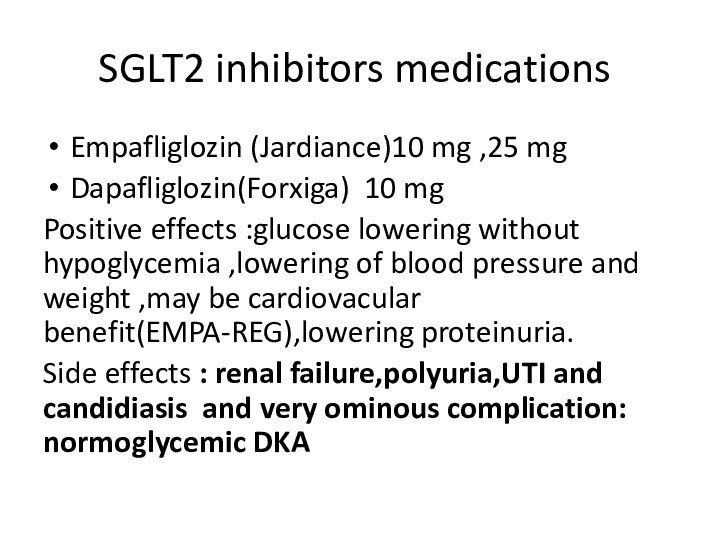
- 91. SGLT2 inhibitors medicationsEmpafliglozin (Jardiance)10 mg ,25
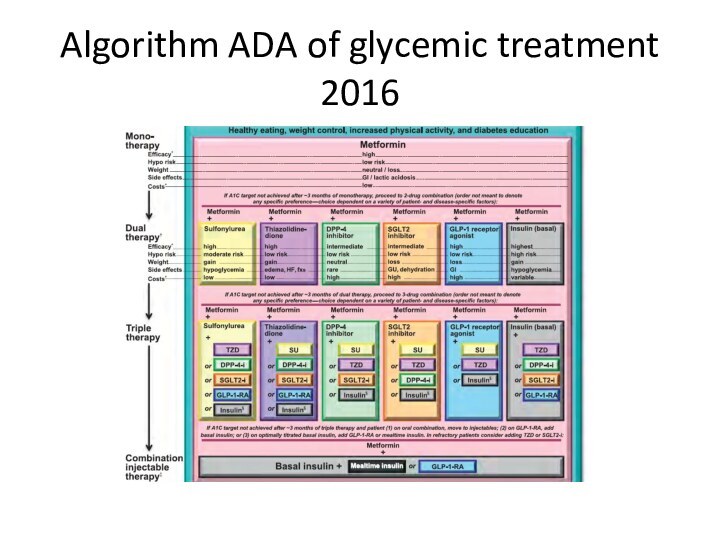
- 92. Algorithm ADA of glycemic treatment 2016
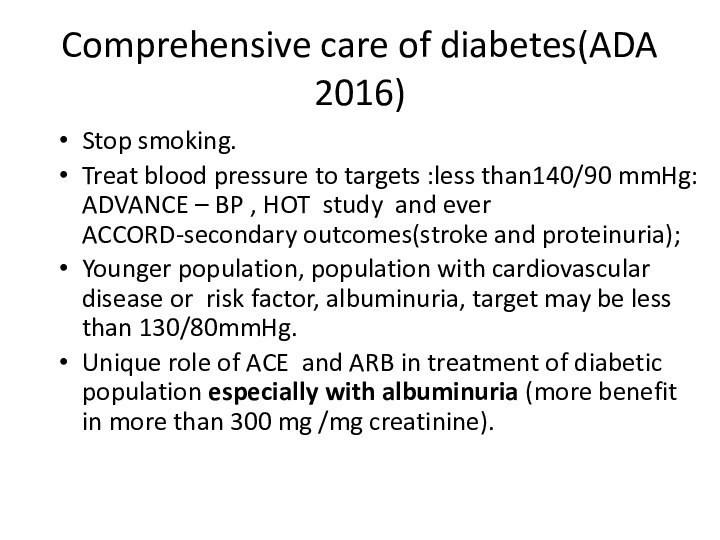
- 93. Comprehensive care of diabetes(ADA 2016) Stop smoking.Treat
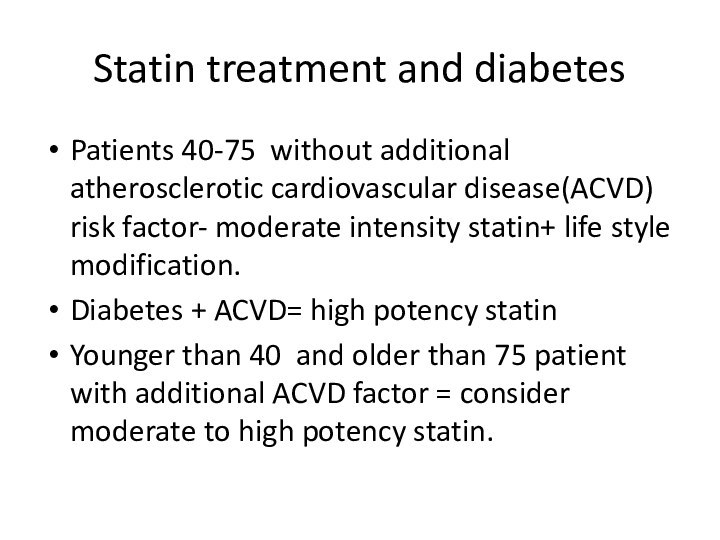
- 94. Statin treatment and diabetes Patients 40-75 without
- 95. Скачать презентацию
- 96. Похожие презентации
Слайд 2
Diabetes
Definition ,classification, type 1 and 2, acute and
chronic complications , treatment
Слайд 3
Diabetes definition
Diabetes is a heterogeneous, complex metabolic disorder
characterized by elevated blood glucose concentration secondary to either
resistance to the action of insulin, insufficient insulin secretion, or both.
Слайд 4
Classification of disorders of glycemia
Type 1- beta-cell
destruction, usually leading to absolute insulin deficiency
1. Autoimmune
2.
Idiopathic Type 2 – progressive loss of insulin secretion on background of insulin resistance
Other specific types:
Genetic defects of beta-cell function
Genetic defects in insulin action
Diseases of the exocrine pancreas
Endocrinopathies
Drug- or chemical-induced
Infections
Uncommon forms of immune-mediated diabetes
Other genetic syndromes sometimes associated with diabetes
Gestational diabetes
Слайд 5
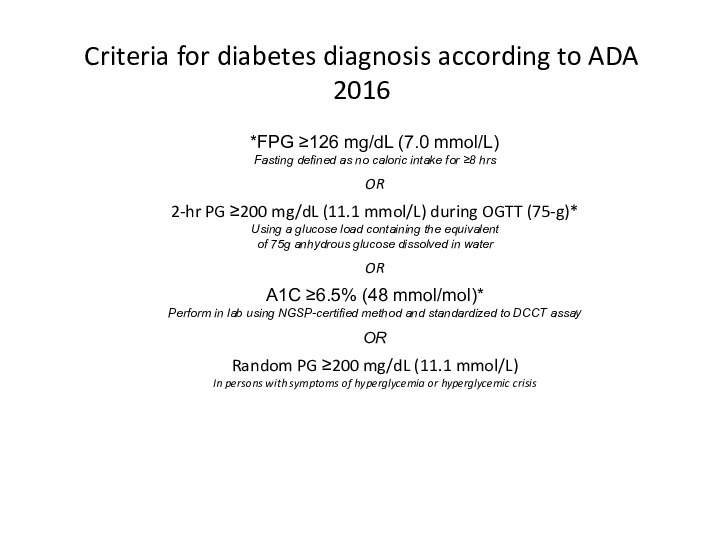
Criteria for diabetes diagnosis according to ADA 2016
*In
absence of unequivocal hyperglycemia, result to be confirmed by
repeat testing FPG=fasting plasma glucose; OGTT=oral glucose tolerance test; PG=plasma glucoseAmerican Diabetes Association.
Diabetes Care. 2016;39(suppl 1):S1-S106.
Слайд 7
Diabetes type 1
Usually caused by autoimmune heterogenic destruction
of beta-cells.
The prevailing immune process that destructs beta-cells is
cellular , mostly T-cell mediated.Pathogenic role of accompanying antibodies is less clear.
Слайд 8
Diabetes type 1
Roughly 5-15% of all cases of
diabetes.
Two peaks:5-7 year and adolescence.
Yearly incidence of 15-25 cases
per 100,000 people younger than 18 years.Finland (60 cases per 100000 people)and Sardinia has the highest prevalence rates for type 1 DM (approximately 20% of the total number of people with DM), while China and Japan have the lowest prevalence rates, with less than 1% of all people with diabetes.
Слайд 10
Autoantibodies (90% at the diagnosis of type 1)
Anti
GAD(Glutamic Acid Decarboxilase) 65 .
Anti ICA (IA-2) 512.
Anti –Insulin.
Anti
Zn T8.4% of normal persons express one of more of the four auto-antibodies.
Prior probability of disease greatly improved diagnostic value of antibodies .
Two or more auto-antibodies – risk of 90% for type 1 developement for 10 years.
Слайд 12
Diabetes type2
90 % of all diabetes in the
world
9.3% of USA population in 2014(29.1 million people),8.1 million
of them was undiagnosed(27.9%)11% of total health spending on adults.
“Epidemic” of diabetes
Слайд 14
Genetic defects of insulin secretion
2-5% of all
cases of diabetes mellitus
Heterogeneous group of diabetes mellitus including
MODY (maturity-onset diabetes of the young), mitochondrial diabetes and neonatal diabetesCommon pathophysiological pathway in monogenic disorders is impaired insulin secretion of the pancreatic beta cell
Слайд 15
High index of suspicion of MODY
A family history
of diabetes in one parent and first-degree relatives, age
at diagnosis usually before 25–30 years.Lack of islet autoantibodies (to differentiate from type 1 diabetes at a young age).
Low or no insulin requirements 2 years after diagnosis.
Absence of obesity (based on body mass index [BMI] values at diagnosis and follow-up examination).
Слайд 18
MODY 3(HNF1α mutation)
Most prevalent MODY:50-70 % of all
mutations.
Onset before age of 30.
Accented postprandial hyperglycemia (increases over
time due to decline of beta cell insulin secretion over time 1-4 % per year).Same rate of complication as type 1and 2.
Very sensitive to sulfonylurea treatment , insulin in pregnancy.
Слайд 19
MODY 2
Mild hyperglycemia started at birth.
The glucokinase enzyme
catalyzes the rate limiting step of glucose phosphorylation –”glucose
sensor” in the pancreas and liver.Mild fasting hyperglycemia.
No apparent deterioration of beta-cell function.
.
Слайд 21
Genetic defects in insulin action
Rabson Mendenhall :short stature,protuberant
abdomen ,teethand nail abnormalities
Leprehuanism: IUGR,fasting hypoglycemia ,death within the
first year of life Mutation of insulin receptor : severe insulin resistance
Type A insulin resistance: acanthosis nigricans, hyperandrogenism, milder type of resistance than other
Lipoatrophic diabetes : severe insuline resistance , lipoatrophy ,hypertygliceridemia
Слайд 22
Disorder of exocrine pancreas
Chronic pancreatitis: more than 20
years of disease -80-90% risk of DM.
Pancreatectomy, pancreatic cancer,
CF.These form of diabetes are milder than typical DM type 1 because of glucagon deficiency.
Hemochromatosis.
Слайд 23
Endocrinopathies
Cushing disease and syndrome-glucose intolerance and overt diabetes
(30 %).
Acromegaly –direct anti- insulin effect - from IGT
to overt diabetes. Pheochromocytoma
Hyperaldosteronism.
Somastatinoma and glucagonoma.
Слайд 24
examples))Drug and chemicals
Ethanol – chronic pancreatitis-overt diabetes(1% of
all diabetes in USA)
Glucocorticoids: inhibition of insulin secretion and
insulin resistance.Cytotoxic medication(e.g. cyclosporine)-inhibition of insulin release from beta-cell.
Protease inhibitors-insulin resistance.
Interferon- β- antibodies to beta cells.
Pentamidin – beta -cell destruction.
Vacor –rodentacid- beta- cell destruction.
Слайд 25
Infections
Predisposition to type 1- enteroviruses.
Direct beta- cells destruction-mumps
,coxsackieviruses B, adenoviruses .
Congenital rubella ? .
Abscess and phlegmone
of pancreas.
Слайд 26
Uncommon immune form of diabetes
High titers of
antibodies to insulin receptors - severe hyperglycemia,acanthosis nigricans
Hirata
syndrome – unusual high titers of auto-insulin antibodies- associated with hypoglycemia. Type 1 as a part of different autoimmune syndrome(APS-1,IPEX) or “ mixed type” diabetes in POEMS myeloma.
Слайд 27
Pregnancy in women with normal glucose
metabolism
Fasting levels
of blood glucose that are lower than in the
non-pregnant state due to insulin-independent glucose uptake by the placenta.
Postprandial hyperglycemia and carbohydrate intolerance as a result of diabetogenic placental hormones.(hPL).
Слайд 28
Gestational diabetes mellitus(GDM)
Disbalance between insulin secretion and increased
insulin resistance especially in the third trimester.
Any degree
of glycose intolerance that was recognized during pregnancy.The Hyperglycemia and Adverse Pregnancy Outcome (HAPO) multinational cohort study a 25,000 pregnant women, demonstrated that risk of adverse maternal, fetal, and neonatal outcomes continuously increased as a function of maternal glycemia at 24–28 weeks.
Слайд 30
Algorithm of glucose testing in pregnancy
All women have
to be screened for diabetes as essential part of
pregnancy planning and be counseled about importance of strict glycemic control in pregnancy.All women must be tested for diabetes in the first pregnancy visit (as early as possible in the first trimester).
6-12 week after delivery all women with GDM have to undergo OGTT with 75 gram glucose load in order to rule out or rule in persistent diabetes or prediabetes(IGT).
Treatment of woman with previous GDM and IGT with lifestyle intervention and metformin can delay or prevent diabetes in the future(30-40% for 10 years comparing with placebo , for 3 years NNT is 5-6 for 1 case ) .
Слайд 31
Goals of diabetes treatment
Prevent macrovasular diabetes complication-cardiovascular disease
(IHD, diabetic cardiomyopathy, TIA, fatal and non- fatal CVA).
Prevent
microvascular diabetes complication:Retinopathy
Neuropathy
Nephropathy- diabetic kidney disease
Alleviate hyperglycemic symptoms.
Prevent/treat diabetic ketoacidosis(DKA) and non-ketotic hyperosmolar state (coma).
Слайд 32
Aspects of diabetes treatment
Glycemic control
Lifestyle intervention include
obesity treatment
Medical nutritional therapy
Control of high blood
pressureControl of dyslipidemia
Anti-agreggant therapy
Слайд 33
Glycemic control and diabetic complication
Type 1 study:
DCCT –EDIC(Diabetes Control and Complication Trial-
Epidemiology
of Diabetes Control and Complications)Principal type 2 studies:
UKPDS(The UK Prospective Diabetes Study).
ADVANCE (Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation ).
ACCORD (Action to Control Cardiovascular Risk in Diabetes).
VADT(Veteran Affairs Diabetes Trial).
Be careful of new “wonder” drugs for diabetes and “smashing hit” studies!!!
Слайд 34
DCCT
N = 1441 T1DM
Intensive
(≥ 3 injections/day or CSII)
vs.
\
Conventional
(1-2 injections per day)
Слайд 35
Inclusion criteria for DCCT
Primary prevention group :
DM type 1: 1-5 years, no retinopathy or severe
diabetic complication, no hypertension or hypercholesteremia, no severe medical condition: urinary microalbumin less than 40 mg for 24 hour .Primary intervention group: the same duration of diabetes, very mild –to moderate non-prolipherative retinopathy, albumin secretion less than 400 mg for 24 hours, no severe diabetic complication ,no hypertension or hypercholesteremia, no severe medical condition.
Слайд 37
Goals and modes of therapy
conventional group
Conventional group therapy
goals: to prevent symptoms attributable to glycemia or glycosuria,
absence of ketones in urine, maintenance of normal growth development ,” ideal “ body weight ,freedom from severe and frequent hypoglycemia.Treatment of conventional group :one or two insulin injection including mixed intermediate and rapid acting insulin, self -monitoring of blood and urine glucose, education about diet and exercise, no usual daily adjustment of insulin dose .
Слайд 38 Goals and modes of treatment intensive treatment group
3 or more insulin injection or pump therapy.
Self monitoring
of blood glucose at least 4 times a day.Dose or method adjustment to treatment goals :
fasting glucose 70-120 mg/dl
postprandial of less than 180 mg/dl
Weekly 3a.m. more than 65 mg/dl
HbA1- 6 % and less
Women who were planning a pregnancy or became pregnant receive intensive therapy until the time of delivery .
Слайд 39
Study questions
Prevention of diabetic retinopathy in primary
prevention group by intensive treatment versus conventional group .
Influence
on progression of diabetic retinopathy in secondary intervention groupintensive treatment versus conventional group .Renal, neurologic, neuropsychological cardiovascular outcomes in two groups.
Adverse effect of two modes of treatment.
Слайд 40
Reduction in Retinopathy
The Diabetes Control and Complications Trial
Research Group. N Engl J Med 1993;329:977-986.
Primary Prevention
Secondary
Intervention 76% RRR
(95% CI 62-85%)
54% RRR
(95% CI 39-66%)
RRR = relative risk reduction CI = confidence interval
Слайд 41
Solid line = risk of developing microalbuminuria
Dashed line
= risk of developing macroalbuminuria
DCCT: Reduction in Albuminuria
The Diabetes
Control and Complications Trial Research Group. N Engl J Med 1993;329:977-986.34% RRR (p<0.04)
43% RRR
(p=0.001)
56% RRR
(p=0.01)
Primary Prevention
Secondary Intervention
guidelines.diabetes.ca | 1-800-BANTING (226-8464) | diabetes.ca
Copyright © 2013 Canadian Diabetes Association
RRR = relative risk reduction
CI = confidence interval
Слайд 42
Reduction in Neuropathy
The Diabetes Control and Complications Trial
Research Group. N Engl J Med 1993;329:977-986.
Слайд 43 DCCT/EDIC Study Research Group. N Engl J Med
2005;353:2643–2653.
Reduction of cardiovascular event in DCCT –EDIC
57% risk
reduction
(P=0.02; 95% CI: 12–79%)
MI, stroke or CV death
Conventional
treatment
Intensive
treatment
Years since entry
0.12
0.10
0.08
0.06
0.04
0.02
0.00
0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21
Слайд 44
Hypoglycemia and other adverse events
General and
severe hypoglycemia 3 times higher in intensively treatment group
including coma and seizures.Weight gain 4.6 kg more in intensively treated group.
No death , no more cardiovascular events during hypoglycemia.
No decline of quality of life, no difference in neuropsychological functioning.
May be more MVA in cases of severe hypoglycemia.
Слайд 45
GLYCEMIC CONTROL IN TYPE 2
UKPDS
20-year interventional
trial from 1977 to 1997.
5,102 patients with newly-diagnosed type
2 diabetes recruited between 1977 and 1991.Median follow-up 10.0 years, range 6 to 20 years.
Слайд 46
UKPDS: Aims
To determine whether improved glucose control of
Type 2 diabetes will prevent clinical complications
Does therapy
withsulphonylurea - first or second generation
insulin
metformin
has any specific advantage or disadvantage
Слайд 47
UKPDS patient characteristics
5102 newly diagnosed Type 2 diabetic
patients
age 25 - 65 y mean 53 y
gender
male : female 59 : 41% ethnic group Caucasian 82% Asian 10%
BMI mean 28 kg/m2
FPG median 11.5 mmol/L (207 mg/dl)
HbA1c median 9.1 %
hypertensive 39%
Слайд 48
Treatment Policies in 3867 patients
Conventional Policy n =
1138
initially with diet alone
aim for near normal weight, best
fasting plasma glucose < 15 mmol/l (270 mg/dl ), asymptomatic when marked hyperglycaemia develops allocate to non-intensive pharmacological therapy
Intensive Policy with sulphonylurea or insulin n = 2729
aim for fasting plasma glucose < 6 mmol/L(108 mg/dl), asymptomatic
when marked hyperglycaemia develops
on sulphonylurea add metformin, move to insulin therapy
on insulin, transfer to complex regimens
Слайд 49
UKPDS Study Group. Lancet 1998; 352:837–853.
UKPDS: intensive
control reduces complications in type 2 diabetes
Слайд 51
UKPDS- metformin
Main Randomisation
4209
Overweight
1704
Non overweight
2505
Conventional Policy
411
Intensive Policy
1293
Metformin
342
Insulin or
Sulphonylurea
951
overweight (>120% Ideal Body Weight) UKPDS patients could be
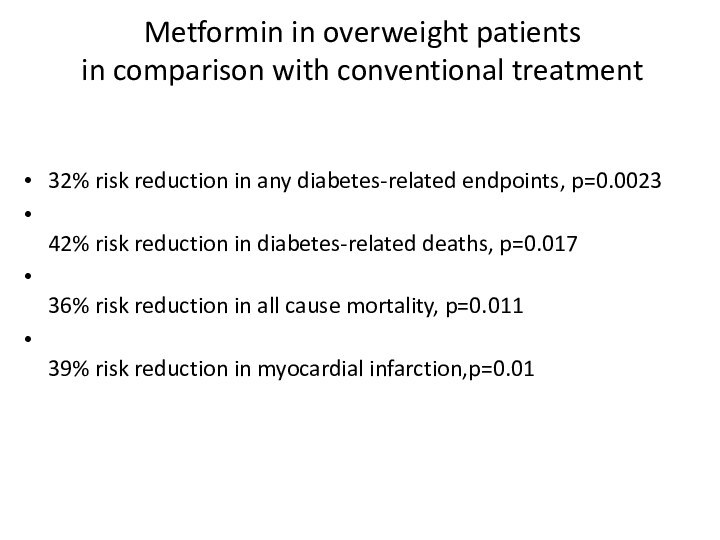
randomised to an intensive glucose control policy with metforminСлайд 52 Metformin in overweight patients in comparison with conventional treatment
32% risk reduction in any diabetes-related endpoints, p=0.0023
42% risk
reduction in diabetes-related deaths, p=0.01736% risk reduction in all cause mortality, p=0.011
39% risk reduction in myocardial infarction,p=0.01
Слайд 53
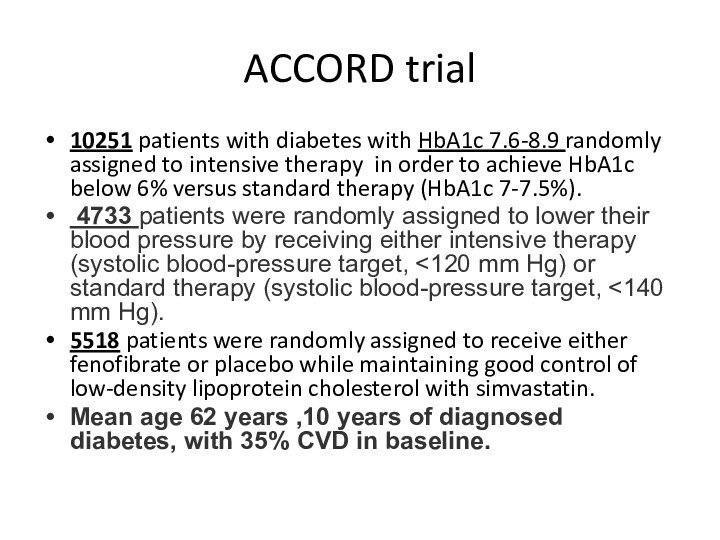
ACCORD trial
10251 patients with diabetes with HbA1c
7.6-8.9 randomly assigned to intensive therapy in order to
achieve HbA1c below 6% versus standard therapy (HbA1c 7-7.5%).4733 patients were randomly assigned to lower their blood pressure by receiving either intensive therapy (systolic blood-pressure target, <120 mm Hg) or standard therapy (systolic blood-pressure target, <140 mm Hg).
5518 patients were randomly assigned to receive either fenofibrate or placebo while maintaining good control of low-density lipoprotein cholesterol with simvastatin.
Mean age 62 years ,10 years of diagnosed diabetes, with 35% CVD in baseline.
Слайд 56
Gerstein HC et al. The ACCORD Study Group.
N Engl J Med. 2008;358:2545–2559.
Results of the Randomized Comparison
of an Intensive Versus a Standard Glycemic Strategy Unadjusted HR for P-value
Intensive vs. Standard (95% CI)
All-cause mortality 1.22 (1.01-1.46) 0.04
Primary endpoint:
CV death, MI, stroke 0.90 (0.78-1.04) 0.16
CV death 1.35 (1.04-1.76) 0.02
Non-fatal MI 0.76 (0.62-0.92) 0.004
Non-fatal stroke 1.06 (0.75-1.50) 0.74
Слайд 59
Results of intensive glucose lowering in ADVANCE trial
Average
lowering of HbA1c from 7.2 to 6.5%
Similar base line
characteristic of patients. (average age :66 years, diabetes duration of 8 years in average , prevalence of CVD 32%)
Слайд 60
VA Diabetes Trial (VADT)
Similar study design: intensive therapy
versus standard therapy.
Primary endpoint: first CVD event after randomization.
Subjects
with longer durations of diabetes, more CVD, higher baseline A1C.Duckworth W, Abraira C, Moritz T, et al. N Engl J Med. 2009;360:129-139.
Слайд 61
Differences in ACCORD/ADVANCE/VADT
Skyler JS, Bergenstal R, Bonow
RO, et al. Diabetes Care. 2009;32:187-192.
Слайд 63
Initial results
No excess of cardiovascular mortality.
No improvement of
cardiovascular morbidity.
No change in incidence of neuropathy or no
change in rate of progression of neuropathy.But …improvement in progression from normal kidney function to microalbuminuria and from microalbuminuria to macroalbuminuria was significant favoring intensive arm .
Слайд 69
Glycemic targets for treatment of pregnant women with
type 1 and 2 diabetes
Glycemic targets for women with
GDM Optimal Hba1C :6-6,5% (avoid maternal hypoglycemia!)
Слайд 70 Type 1 insulin treatment Concept of basal -
bolus
Prescription of short and long acting insulins imitating physiologic
insulin secretion.It is the modern method to treat type1 and advanced type 2 diabetes .
Basal insulin injected once to time daily in order to control hepatic glucose output.
Premeal insulin is added in order to prevent postprandial glycemia.
Слайд 71
Serum Insulin Level
Time
guidelines.diabetes.ca | 1-800-BANTING (226-8464) | diabetes.ca
Copyright
© 2013 Canadian Diabetes Association
Слайд 74
:Principles of type 2 treatment
(1)non –pharmacologic therapy
Physical activity.
1.1Minimum 150 minutes weekly moderate intensity physical activity (50-70%
of maximal heart rate ) at least 3 days weekly . 1.2 Reduce sedentary time to 90 min.
1.3Minimum two session in week of resistance exercise : set of 5 exercise involving large muscle group.
Слайд 75
:Principles of type 2 treatment
(2)non –pharmacologic therapy
Diet and
carbohydrates
500-750 kcal/d deficit:1200-1500 kcal /d for women,1500-1800 kcal/d for
men:5% weight loss, ideally 7% No ideal amount !!(but keep in with total advised caloric intake!).
Replace refined carbohydrate and added sugars with whole grains, legumes, vegetables, and fruits.
Keep in mind carb counting in IDDM.
Слайд 76
:Principles of type 2 treatment
(3)non –pharmacologic therapy
Diet and
proteins
0.8 g/kg daily allowance.
Enhance insulin response to carbohydrates.
Don’t use
protein- rich carbohydrate sources to revent hypoglycemia .Diet and fat
Rich in monounsaturated fat (Mediterranean style diet ).
25-30 % caloric intake.
Sodium in diet:
Restrict to 2300 mg .
Restrict alcohol consumption to one drink a day for adult woman and two drink a day to adult man .
Слайд 77
Pharmacological treatment of glycemia type 2:drug classification
Biguanides
Secretagogues
DPP4 inhibitors
α-
glycosidase inhibitor
Thiazolidinedione
GLP1 agonists
SGLT2 inhibitors
Insulin
Слайд 78
Biguanides
Metfomin(Glucomin,Glucophage)
Preferred initial pharmacologic agent because of long standing
record of efficacy and safety and lowering CV outcomes(UKPDS).
Mechanism:
Decreased hepatic gluconeogenesis by activation of AMP kinase.
Other : lowering peripheral insulin resistance.
Слайд 79
Metformin
Half-life up to 3 hour.
No metabolism ,excreted by
kidney as active compound.
May be safely continued down to
glomerular filtrationrate (GFR) of 45 mL/min/1.73m2 or even 30 mL/min/1.73 m2 with reduced dosage.Maximal dosage 2550 mg (usually 2-3 times daily.
Слайд 80
Metformin toxicity and side effects
Gastrointestinal (20-30%): start with
lower dose with or after meals, make rotation with
various formulationB12 deficiency.
Lactic acidosis :( very uncommon ) don’t use in advanced CKD, advanced liver disease, shock, severe infection ,alcoholism.
Слайд 81
Secretagogues
Sulfonylureas: bind to SUR1 site of inward rectified
KATP channel on beta-cells :
2 generation
First generation: now
abandoned because of cases of prolong hypoglycemia ,hyponatremia (chlorpropamide),transient leucopenia and thrombocytopenia (less than 1%) and multiple drug interaction.Second generation: more safe.
Слайд 82
2-nd generation sulfonylureas
Adverse effect : hypoglycemia ,weight gain
Secondary
failure : sulfonylureas require functional beta -cells ,they lose
efficacy with diabetes progression because of beta -cell failure.
Слайд 83
Glinides
Binding to distinct (from sulfonylurea) SUR 1 site
Burst phase-1 insulin secretion
In vitro- glucose dependent but
in vivo notMedications:
Repaglinide(Novonorm)
Nateglinide
Pharmacokinetics:
Rapid onset of action
Plasma half -life less than 1 hour
Intensive hepatic metabulism
Use for coverage postprandial glucose rise
Suitable for CKD
Repaglinide 3 times daily 15 minutes before meal: 0,5 mg to 4 mg 3 to 4 times daily
Adverse effect : hypoglycemia ,weight gain
Слайд 84
DPP-IV: ACTION
Cleaves GLP-1
Results in decreased signal to the
pancreas—limiting insulin response.
That in turn decreases the signal to
the liver resulting in increased hepatic glucose production.HYPERGLYCEMIA
X
Слайд 86
DPP4 inhibitors
Januvia
Trajenta
Onglysa
Galvus
Name
Class Half-life Dose (mg) Use
Very few side effects: mostly gastrointestinal
Neutral weight effect
Слайд 87
GLP1 agonists(injectable agents)
Breakthrough in DM 2 treatment
Glycemic
,cardiovascular (LEADER study)benefit , significant weight loss .
Side
effects :Gastrointestinal side effects , weakness , mild tachycardia ,local injection reaction .Exenatide (Byetta) 5-10 mg twice daily SC
Exenatide SR (Bydureon) 2mg once weekly SC
Liraglutide (Victoza)0.6 -1.8 mg once daily
Dulaglutide (Trulicity) 0,75 mg- 1.5 mg once weekly
Слайд 88
α- glucosidase inhibitors
Acarbose (Prandase ) max 100 mg
*3/d
May have cardiovascular benefits (STOP – NIDDM trial)
Prohibited in
advanced CKD
Слайд 89
Thiazolidinediones
Gamma- PPAR agonists.
Increase of insulin sensitivity in adipose
tissue skeletal muscle and liver.
Warning about potential increase of
acute MI (ACCORD) Side effects : weight gain because of fluid retention, worsening of heart failure ,anemia, increased risk of fracture.
Medication :
Rosiglitazone (Avandia)4,8 ,16 mg once daily.
Pioglitazone(Actos)15- 45 mg once daily.
Слайд 91
SGLT2 inhibitors medications
Empafliglozin (Jardiance)10 mg ,25 mg
Dapafliglozin(Forxiga) 10 mg
Positive effects :glucose lowering without hypoglycemia ,lowering
of blood pressure and weight ,may be cardiovacular benefit(EMPA-REG),lowering proteinuria.Side effects : renal failure,polyuria,UTI and candidiasis and very ominous complication: normoglycemic DKA
Слайд 93
Comprehensive care of diabetes(ADA 2016)
Stop smoking.
Treat blood
pressure to targets :less than140/90 mmHg: ADVANCE – BP
, HOT study and ever ACCORD-secondary outcomes(stroke and proteinuria);Younger population, population with cardiovascular disease or risk factor, albuminuria, target may be less than 130/80mmHg.
Unique role of ACE and ARB in treatment of diabetic population especially with albuminuria (more benefit in more than 300 mg /mg creatinine).
Слайд 94
Statin treatment and diabetes
Patients 40-75 without additional
atherosclerotic cardiovascular disease(ACVD) risk factor- moderate intensity statin+ life
style modification.Diabetes + ACVD= high potency statin
Younger than 40 and older than 75 patient with additional ACVD factor = consider moderate to high potency statin.